Yonsei Med J.
2012 Nov;53(6):1203-1210. 10.3349/ymj.2012.53.6.1203.
Histological Analysis of Benign Breast Imaging Reporting and Data System Categories 4c and 5 Breast Lesions in Imaging Study
- Affiliations
-
- 1Department of Radiology, Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul, Korea.
- 2Department of Pathology, Yonsei University College of Medicine, Seoul, Korea. kjs1976@yuhs.ac
- KMID: 1414265
- DOI: http://doi.org/10.3349/ymj.2012.53.6.1203
Abstract
- PURPOSE
The objective of this study was to analyze the histology of breast lesions categorized as Breast Imaging Reporting and Data System (BI-RADS) 4c or 5 breast lesions during the imaging evaluation, but diagnosed as benign during the histological evaluation.
MATERIALS AND METHODS
We retrospectively reviewed 71 breast lesions categorized as BI-RADS 4c or 5 during imaging study, but diagnosed as benign upon histological evaluation.
RESULTS
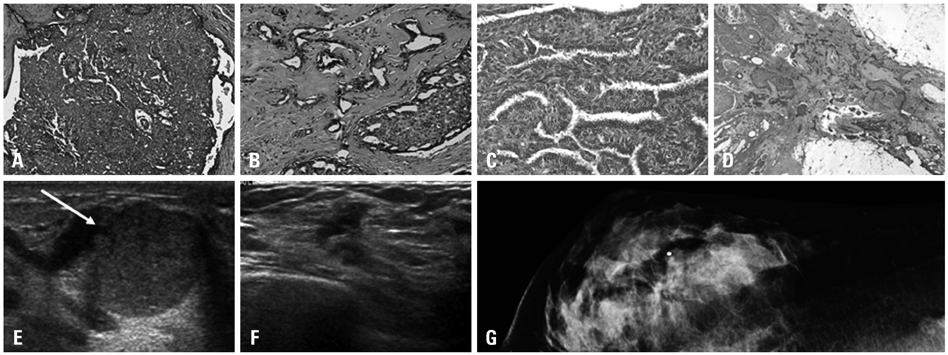
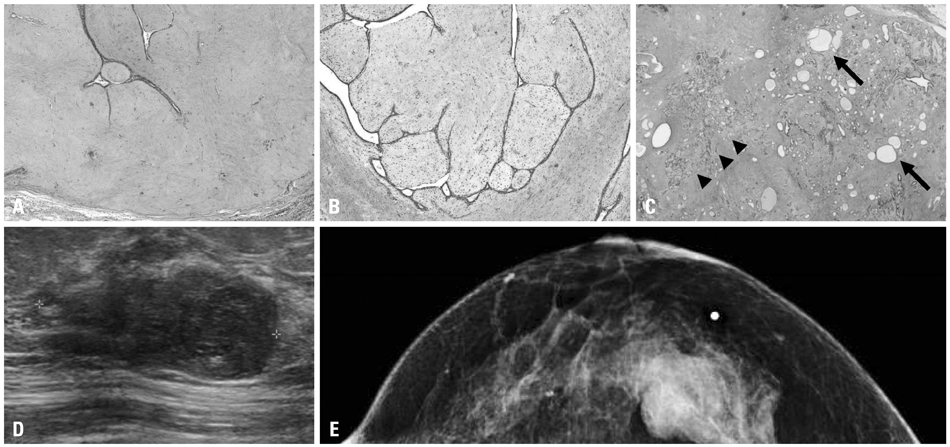
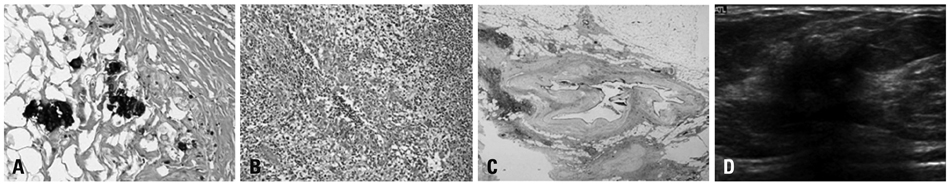
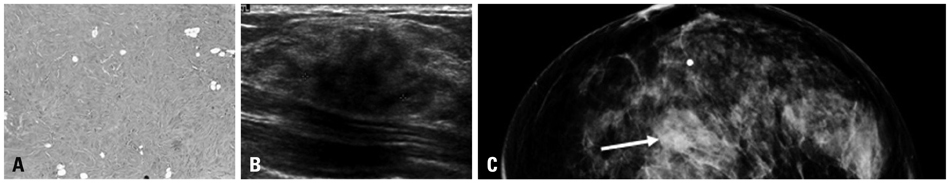
Breast lesions were classified into six groups upon histological analysis: intraductal papilloma (18 cases), inflammatory group (15 cases), fibroepithelial tumor (14 cases), clustered microcalcification (10 cases), minimal histological alteration (10 cases), and adenosis (4 cases). Sclerosis and architectural complexity were associated with most of the biopsies that were morphologically similar to malignancy.
CONCLUSION
Among 71 cases categorized as 4c or 5 during the imaging study, but diagnosed as benign upon histological examination, intraductal papilloma was the most frequently identified histological lesion. These 71 cases exhibited histological characteristics of sclerosis and/or complex/complicated features that should be histologically differentiated from malignancy during evaluation.
MeSH Terms
Figure
Reference
-
1. Buchberger W, DeKoekkoek-Doll P, Springer P, Obrist P, Dünser M. Incidental findings on sonography of the breast: clinical significance and diagnostic workup. AJR Am J Roentgenol. 1999. 173:921–927.
Article2. Poplack SP, Tosteson AN, Grove MR, Wells WA, Carney PA. Mammography in 53,803 women from the New Hampshire mammography network. Radiology. 2000. 217:832–840.
Article3. Berg WA, Blume JD, Cormack JB, Mendelson EB, Lehrer D, Böhm-Vélez M, et al. Combined screening with ultrasound and mammography vs mammography alone in women at elevated risk of breast cancer. JAMA. 2008. 299:2151–2163.
Article4. Houssami N, Lord SJ, Ciatto S. Breast cancer screening: emerging role of new imaging techniques as adjuncts to mammography. Med J Aust. 2009. 190:493–497.
Article5. Obenauer S, Hermann KP, Grabbe E. Applications and literature review of the BI-RADS classification. Eur Radiol. 2005. 15:1027–1036.
Article6. Lazarus E, Mainiero MB, Schepps B, Koelliker SL, Livingston LS. BI-RADS lexicon for US and mammography: interobserver variability and positive predictive value. Radiology. 2006. 239:385–391.
Article7. Mendelson E, Baum J, Berg W, Merritt C, Rubin E. Ultrasound. Breast Imaging Reporting and Data System (BI-RADS). 2003. 4th ed. Reston, VA: American College of Radiology.8. Kim EK, Ko KH, Oh KK, Kwak JY, You JK, Kim MJ, et al. Clinical application of the BI-RADS final assessment to breast sonography in conjunction with mammography. AJR Am J Roentgenol. 2008. 190:1209–1215.
Article9. Yoon JH, Kim MJ, Moon HJ, Kwak JY, Kim EK. Subcategorization of ultrasonographic BI-RADS category 4: positive predictive value and clinical factors affecting it. Ultrasound Med Biol. 2011. 37:693–699.
Article10. ACR BI-RADS, breast imaging and reporting data systems: breast imaging atlas; mammography, breast ultrasound, magnetic resonance imaging. 2003. Reston, VA: American College of Radiology.11. Raza S, Chikarmane SA, Neilsen SS, Zorn LM, Birdwell RL. BI-RADS 3, 4, and 5 lesions: value of US in management--follow-up and outcome. Radiology. 2008. 248:773–781.
Article12. Stavros AT, Thickman D, Rapp CL, Dennis MA, Parker SH, Sisney GA. Solid breast nodules: use of sonography to distinguish between benign and malignant lesions. Radiology. 1995. 196:123–134.
Article13. Baek SE, Kim MJ, Kim EK, Youk JH, Lee HJ, Son EJ. Effect of clinical information on diagnostic performance in breast sonography. J Ultrasound Med. 2009. 28:1349–1356.
Article14. Lee HJ, Kim EK, Kim MJ, Youk JH, Lee JY, Kang DR, et al. Observer variability of Breast Imaging Reporting and Data System (BI-RADS) for breast ultrasound. Eur J Radiol. 2008. 65:293–298.
Article15. Park CS, Lee JH, Yim HW, Kang BJ, Kim HS, Jung JI, et al. Observer agreement using the ACR Breast Imaging Reporting and Data System (BI-RADS)-ultrasound, First Edition (2003). Korean J Radiol. 2007. 8:397–402.
Article16. You JK, Kim EK, Kwak JY, Kim MJ, Oh KK, Park BW, et al. Focal fibrosis of the breast diagnosed by a sonographically guided core biopsy of nonpalpable lesions: imaging findings and clinical relevance. J Ultrasound Med. 2005. 24:1377–1384.
Article17. Stavros A. Breast Ultrasound. 2004. Philadelphia: Lippincott Williams & Wilkins.18. Han BK, Choe YH, Park JM, Moon WK, Ko YH, Yang JH, et al. Granulomatous mastitis: mammographic and sonographic appearances. AJR Am J Roentgenol. 1999. 173:317–320.
Article19. Sweeney DJ, Wylie EJ. Mammographic appearances of mammary duct ectasia that mimic carcinoma in a screening programme. Australas Radiol. 1995. 39:18–23.
Article20. Schnitt SJ, Collins LC. Biopsy Interpretation of the Breast. 2009. 1st ed. New York: Lippincott Williams & Wilkins.21. Mitnick JS, Vazquez MF, Harris MN, Roses DF. Differentiation of radial scar from scirrhous carcinoma of the breast: mammographic-pathologic correlation. Radiology. 1989. 173:697–700.
Article22. Adler DD, Helvie MA, Oberman HA, Ikeda DM, Bhan AO. Radial sclerosing lesion of the breast: mammographic features. Radiology. 1990. 176:737–740.
Article23. Shah VI, Flowers CI, Douglas-Jones AG, Dallimore NS, Rashid M. Immunohistochemistry increases the accuracy of diagnosis of benign papillary lesions in breast core needle biopsy specimens. Histopathology. 2006. 48:683–691.
Article24. Ichihara S, Fujimoto T, Hashimoto K, Moritani S, Hasegawa M, Yokoi T. Double immunostaining with p63 and high-molecular-weight cytokeratins distinguishes borderline papillary lesions of the breast. Pathol Int. 2007. 57:126–132.
Article25. Tse GM, Tan PH, Lui PC, Gilks CB, Poon CS, Ma TK, et al. The role of immunohistochemistry for smooth-muscle actin, p63, CD10 and cytokeratin 14 in the differential diagnosis of papillary lesions of the breast. J Clin Pathol. 2007. 60:315–320.
Article26. Grin A, O'Malley FP, Mulligan AM. Cytokeratin 5 and estrogen receptor immunohistochemistry as a useful adjunct in identifying atypical papillary lesions on breast needle core biopsy. Am J Surg Pathol. 2009. 33:1615–1623.
Article27. Resetkova E, Hoda SA. "Ossifying-type" mammary calcifications. Arch Pathol Lab Med. 2002. 126:995–996.
Article28. Hoda SA, Gopalan A. Mammary calcifications of the ossifying type. Breast J. 2003. 9:129–130.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Breast Imaging Reporting and Data System (BI-RADS): Advantages and Limitations
- Scoring System to Stratify Malignancy Risks for Mammographic Microcalcifications Based on Breast Imaging Reporting and Data System 5th Edition Descriptors
- Thyroid Imaging Reporting and Data System (TIRADS)
- Optical Imaging of the Breast
- Shear-wave elastography in breast ultrasonography: the state of the art