Endocrinol Metab.
2021 Aug;36(4):800-809. 10.3803/EnM.2021.1040.
High Fibrosis-4 Index Is Related with Worse Clinical Outcome in Patients with Coronavirus Disease 2019 and Diabetes Mellitus: A Multicenter Observational Study
- Affiliations
-
- 1Department of Internal Medicine, Daegu Catholic University Hospital, Daegu Catholic University School of Medicine, Daegu, Korea
- 2Department of Internal Medicine, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- 3Department of Internal Medicine, Yeungnam University Hospital, Yeungnam University College of Medicine, Daegu, Korea
- 4Department of Internal Medicine, Keimyung University Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea
- KMID: 2519668
- DOI: http://doi.org/10.3803/EnM.2021.1040
Abstract
- Background
Based on recent evidence on the importance of the presence of diabetes mellitus (DM) and fibrosis-4 (FIB-4) index in coronavirus disease 2019 (COVID-19) mortality, we analyzed whether these factors could additively predict such mortality.
Methods
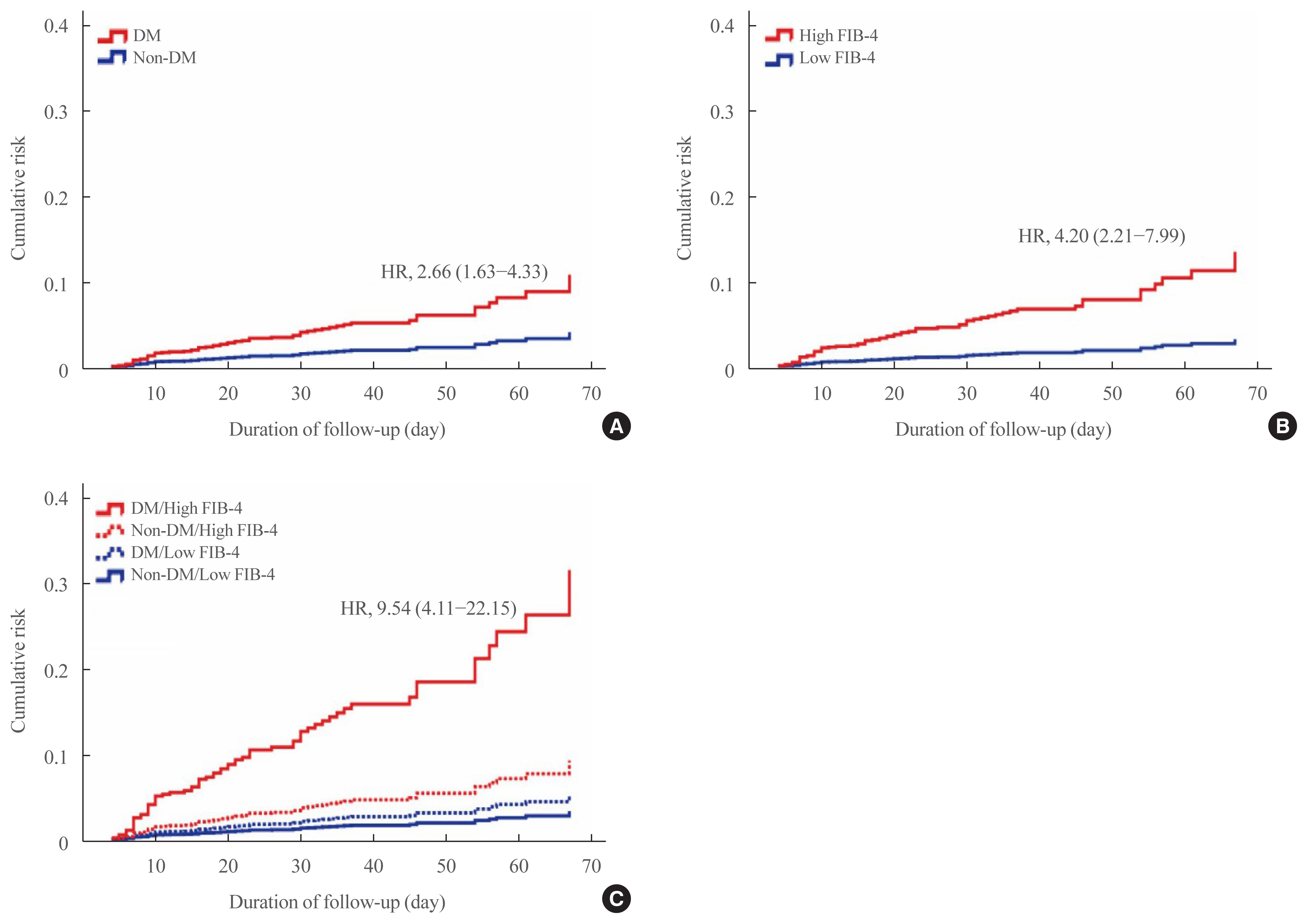
This multicenter observational study included 1,019 adult inpatients admitted to university hospitals in Daegu. The demographic and laboratory findings, mortality, prevalence of severe disease, and duration of quarantine were compared between patients with and without DM and/or a high FIB-4 index. The mortality risk and corresponding hazard ratio (HR) were analyzed using the Kaplan-Meier method and Cox proportional hazard models.
Results
The patients with DM (n=217) exhibited significantly higher FIB-4 index and mortality compared to those without DM. Although DM (HR, 2.66; 95% confidence interval [CI], 1.63 to 4.33) and a high FIB-4 index (HR, 4.20; 95% CI, 2.21 to 7.99) were separately identified as risk factors for COVID-19 mortality, the patients with both DM and high FIB-4 index had a significantly higher mortality (HR, 9.54; 95% CI, 4.11 to 22.15). Higher FIB-4 indices were associated with higher mortality regardless of DM. A high FIB-4 index with DM was more significantly associated with a severe clinical course with mortality (odds ratio, 11.24; 95% CI, 5.90 to 21.41) than a low FIB-4 index without DM, followed by a high FIB-4 index alone and DM alone. The duration of quarantine and hospital stay also tended to be longer in those with both DM and high FIB-4 index.
Conclusion
Both DM and high FIB-4 index are independent and additive risk factors for COVID-19 mortality.
Figure
Reference
-
1. Fu L, Wang B, Yuan T, Chen X, Ao Y, Fitzpatrick T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect. 2020; 80:656–65.
Article2. Kim DW, Byeon KH, Kim J, Cho KD, Lee N. The correlation of comorbidities on the mortality in patients with covid-19: an observational study based on the Korean National Health Insurance Big Data. J Korean Med Sci. 2020; 35:e243.
Article3. Kumar A, Arora A, Sharma P, Anikhindi SA, Bansal N, Singla V, et al. Is diabetes mellitus associated with mortality and severity of COVID-19? A meta-analysis. Diabetes Metab Syndr. 2020; 14:535–45.
Article4. Cai Q, Huang D, Yu H, Zhu Z, Xia Z, Su Y, et al. COVID-19: abnormal liver function tests. J Hepatol. 2020; 73:566–74.
Article5. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382:1708–20.
Article6. Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, et al. Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol. 2018; 15:11–20.
Article7. Eslam M, Newsome PN, Sarin SK, Anstee QM, Targher G, Romero-Gomez M, et al. A new definition for metabolic dysfunction-associated fatty liver disease: an international expert consensus statement. J Hepatol. 2020; 73:202–9.
Article8. Fouad Y, Waked I, Bollipo S, Gomaa A, Ajlouni Y, Attia D. What’s in a name? Renaming ‘NAFLD’ to ‘MAFLD’. Liver Int. 2020; 40:1254–61.
Article9. Kim MK, Jeon JH, Kim SW, Moon JS, Cho NH, Han E, et al. The clinical characteristics and outcomes of patients with moderate-to-severe coronavirus disease 2019 infection and diabetes in Daegu, South Korea. Diabetes Metab J. 2020; 44:602–13.
Article10. Zhou YJ, Zheng KI, Wang XB, Yan HD, Sun QF, Pan KH, et al. Younger patients with MAFLD are at increased risk of severe COVID-19 illness: a multicenter preliminary analysis. J Hepatol. 2020; 73:719–21.
Article11. Gao F, Zheng KI, Wang XB, Yan HD, Sun QF, Pan KH, et al. Metabolic associated fatty liver disease increases coronavirus disease 2019 disease severity in nondiabetic patients. J Gastroenterol Hepatol. 2021; 36:204–7.
Article12. Targher G, Mantovani A, Byrne CD, Wang XB, Yan HD, Sun QF, et al. Risk of severe illness from COVID-19 in patients with metabolic dysfunction-associated fatty liver disease and increased fibrosis scores. Gut. 2020; 69:1545–7.
Article13. Saito Y, Okumura Y, Nagashima K, Fukamachi D, Yokoyama K, Matsumoto N, et al. Impact of the fibrosis-4 index on risk stratification of cardiovascular events and mortality in patients with atrial fibrillation: findings from a Japanese multicenter registry. J Clin Med. 2020; 9:584.
Article14. Jin JL, Zhang HW, Cao YX, Liu HH, Hua Q, Li YF, et al. Liver fibrosis scores and coronary atherosclerosis: novel findings in patients with stable coronary artery disease. Hepatol Int. 2021; 15:413–23.
Article15. Schonmann Y, Yeshua H, Bentov I, Zelber-Sagi S. Liver fibrosis marker is an independent predictor of cardiovascular morbidity and mortality in the general population. Dig Liver Dis. 2021; 53:79–85.
Article16. Park JG, Kang MK, Lee YR, Song JE, Kim NY, Kweon YO, et al. Fibrosis-4 index as a predictor for mortality in hospitalised patients with COVID-19: a retrospective multicentre cohort study. BMJ Open. 2020; 10:e041989.
Article17. Lopez-Mendez I, Aquino-Matus J, Gall SM, Prieto-Nava JD, Juarez-Hernandez E, Uribe M, et al. Association of liver steatosis and fibrosis with clinical outcomes in patients with SARS-CoV-2 infection (COVID-19). Ann Hepatol. 2021; 20:100271.
Article18. Forlano R, Mullish BH, Mukherjee SK, Nathwani R, Harlow C, Crook P, et al. In-hospital mortality is associated with inflammatory response in NAFLD patients admitted for COVID-19. PLoS One. 2020; 15:e0240400.
Article19. Kim MK, Ko SH, Kim BY, Kang ES, Noh J, Kim SK, et al. 2019 Clinical practice guidelines for type 2 diabetes mellitus in Korea. Diabetes Metab J. 2019; 43:398–406.
Article20. Vilar-Gomez E, Chalasani N. Non-invasive assessment of non-alcoholic fatty liver disease: clinical prediction rules and blood-based biomarkers. J Hepatol. 2018; 68:305–15.
Article21. Chung SM, Lee YY, Ha E, Yoon JS, Won KC, Lee HW, et al. The risk of diabetes on clinical outcomes in patients with coronavirus disease 2019: a retrospective cohort study. Diabetes Metab J. 2020; 44:405–13.
Article22. Guo W, Li M, Dong Y, Zhou H, Zhang Z, Tian C, et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diabetes Metab Res Rev. 2020; 36:e3319.23. Cristelo C, Azevedo C, Marques JM, Nunes R, Sarmento B. SARS-CoV-2 and diabetes: new challenges for the disease. Diabetes Res Clin Pract. 2020; 164:108228.
Article24. Li Y, Regan J, Fajnzylber J, Coxen K, Corry H, Wong C, et al. Liver fibrosis index fib-4 is associated with mortality in COVID-19. Hepatol Commun. 2020; 5:434–45.25. Sterling RK, Oakes T, Gal TS, Stevens MP, DeWit M, Sanyal AJ. The fibrosis-4 index is associated with need for mechanical ventilation and 30-day mortality in patients admitted with coronavirus disease 2019. J Infect Dis. 2020; 222:1794–7.
Article26. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395:497–506.
Article27. Fan Z, Chen L, Li J, Cheng X, Yang J, Tian C, et al. Clinical features of COVID-19-related liver functional abnormality. Clin Gastroenterol Hepatol. 2020; 18:1561–6.
Article28. Xu L, Liu J, Lu M, Yang D, Zheng X. Liver injury during highly pathogenic human coronavirus infections. Liver Int. 2020; 40:998–1004.
Article29. Li D, Ding X, Xie M, Tian D, Xia L. COVID-19-associated liver injury: from bedside to bench. J Gastroenterol. 2021; 56:218–30.
Article30. Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018; 67:328–57.
Article31. Sy-Janairo ML, Cua YIH. Association of metabolic-associated fatty liver disease and risk of severe coronavirus disease 2019 illness. JGH Open. 2020; 5:4–10.
Article32. Parikh NS, Kamel H, Navi BB, Iadecola C, Merkler AE, Jesudian A, et al. Liver fibrosis indices and outcomes after primary intracerebral hemorrhage. Stroke. 2020; 51:830–7.
Article33. Cao YX, Zhang M, Zhang HW, Jin JL, Liu HH, Zhang Y, et al. Impact of liver fibrosis score on prognosis in patients with previous myocardial infarction: a prospective cohort study. Liver Int. 2021; 41:1294–304.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dipeptidyl Peptidase-4 Inhibitors and COVID-19-Related Deaths among Patients with Type 2 Diabetes Mellitus: A Meta-Analysis of Observational Studies
- Diabetes Mellitus and COVID-19
- Management of Diabetes in Coronavirus Disease 2019: Prognosis and Practical Issues
- Diabetes and Vitamin D
- Post–Coronavirus Disease 2019 Pulmonary Fibrosis: Wait or Needs Intervention