J Korean Med Sci.
2021 Aug;36(34):e217. 10.3346/jkms.2021.36.e217.
Respiratory Viruses in Acute Exacerbations of Bronchiectasis
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Laboratory Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2519594
- DOI: http://doi.org/10.3346/jkms.2021.36.e217
Abstract
- Background
Bacterial infections are well known factors underlying acute exacerbations in bronchiectasis. However, viral infections may also contribute to acute exacerbations. We aimed to assess the rate of viral detection in acute exacerbations of bronchiectasis, and the associated clinical factors.
Methods
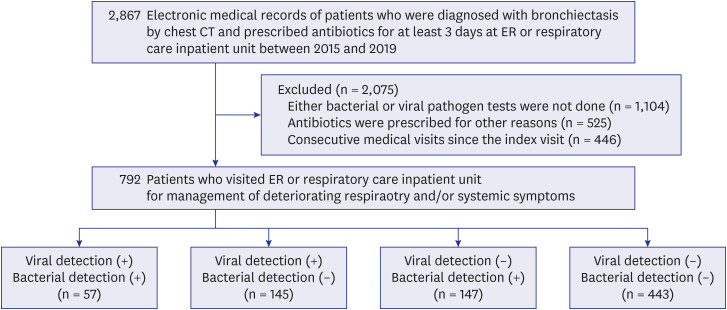
Diagnostic tests for viral and bacterial etiologies were performed in 792 patients with bronchiectasis who visited the emergency room or the respiratory care inpatient unit in a tertiary referral center in South Korea. All patients were diagnosed with bronchiectasis by chest computerized tomography and were prescribed antibiotics for a minimum of 3 days.
Results
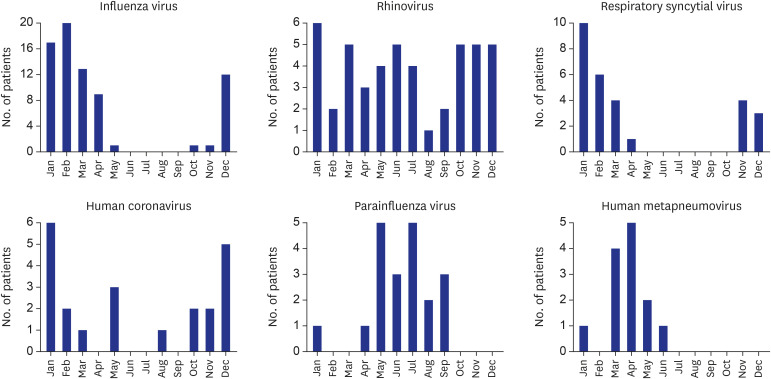
Viral pathogens were detected in 202 of the 792 enrolled patients (25.5%). The most common viral pathogen isolated was influenza A virus (24.8%), followed by rhinovirus (22.4%), influenza B virus (9.8%), respiratory syncytial virus B (8.9%), and human metapneumovirus (6.1%). In 145 patients, a viral, but not bacterial, pathogen was detected, whereas no pathogens were found in 443 patients with exacerbations. Multivariable analysis revealed that female sex and chronic heart disease as a comorbidity were positively associated with viral detection in acute exacerbations of patients with bronchiectasis, whereas the presence of radiographic infiltration was negatively associated.
Conclusion
Respiratory viruses were identified in approximately 25% of the acute exacerbations observed among patients with bronchiectasis. Of the viruses detected, influenza viruses and rhinovirus made up over 50%. More attention to viruses as possible causative pathogens for acute deteriorating symptoms in patients with bronchiectasis is warranted.
Figure
Reference
-
1. Hill AT, Sullivan AL, Chalmers JD, De Soyza A, Elborn SJ, Floto AR, et al. British Thoracic Society guideline for bronchiectasis in adults. Thorax. 2019; 74:1–69.
Article2. Hill AT, Haworth CS, Aliberti S, Barker A, Blasi F, Boersma W, et al. Pulmonary exacerbation in adults with bronchiectasis: a consensus definition for clinical research. Eur Respir J. 2017; 49(6):1700051. PMID: 28596426.
Article3. Chalmers JD, Aliberti S, Polverino E, Vendrell M, Crichton M, Loebinger M, et al. The EMBARC European Bronchiectasis Registry: protocol for an international observational study. ERJ Open Res. 2016; 2(1):00081-2015. PMID: 27730179.
Article4. Chalmers JD, Goeminne P, Aliberti S, McDonnell MJ, Lonni S, Davidson J, et al. The bronchiectasis severity index. An international derivation and validation study. Am J Respir Crit Care Med. 2014; 189(5):576–585. PMID: 24328736.
Article5. Loebinger MR, Wells AU, Hansell DM, Chinyanganya N, Devaraj A, Meister M, et al. Mortality in bronchiectasis: a long-term study assessing the factors influencing survival. Eur Respir J. 2009; 34(4):843–849. PMID: 19357155.
Article6. Goeminne PC, Cox B, Finch S, Loebinger MR, Bedi P, Hill AT, et al. The impact of acute air pollution fluctuations on bronchiectasis pulmonary exacerbation: a case-crossover analysis. Eur Respir J. 2018; 52(1):1702557. PMID: 29903857.
Article7. Mitchell AB, Mourad B, Buddle L, Peters MJ, Oliver BGG, Morgan LC. Viruses in bronchiectasis: a pilot study to explore the presence of community acquired respiratory viruses in stable patients and during acute exacerbations. BMC Pulm Med. 2018; 18(1):84. PMID: 29788952.
Article8. Gao YH, Guan WJ, Xu G, Lin ZY, Tang Y, Lin ZM, et al. The role of viral infection in pulmonary exacerbations of bronchiectasis in adults: a prospective study. Chest. 2015; 147(6):1635–1643. PMID: 25412225.9. Murray PR, Washington JA. Microscopic and baceriologic analysis of expectorated sputum. Mayo Clin Proc. 1975; 50(6):339–344. PMID: 1127999.10. Polverino E, Goeminne PC, McDonnell MJ, Aliberti S, Marshall SE, Loebinger MR, et al. European Respiratory Society guidelines for the management of adult bronchiectasis. Eur Respir J. 2017; 50(3):1700629. PMID: 28889110.
Article11. Price RHM, Graham C, Ramalingam S. Association between viral seasonality and meteorological factors. Sci Rep. 2019; 9(1):929. PMID: 30700747.
Article12. Shek LP, Lee BW. Epidemiology and seasonality of respiratory tract virus infections in the tropics. Paediatr Respir Rev. 2003; 4(2):105–111. PMID: 12758047.
Article13. Dela Cruz CS, Pasnick S, Gross JE, Keller J, Carlos WG, Cao B, et al. Adenovirus infection and outbreaks: what you need to know. Am J Respir Crit Care Med. 2019; 199(7):P13–14. PMID: 30932693.
Article14. Jacobs SE, Lamson DM, St George K, Walsh TJ. Human rhinoviruses. Clin Microbiol Rev. 2013; 26(1):135–162. PMID: 23297263.
Article15. Fisman D. Seasonality of viral infections: mechanisms and unknowns. Clin Microbiol Infect. 2012; 18(10):946–954. PMID: 22817528.
Article16. Dowell SF. Seasonal variation in host susceptibility and cycles of certain infectious diseases. Emerg Infect Dis. 2001; 7(3):369–374. PMID: 11384511.
Article17. Greer A, Ng V, Fisman D. Climate change and infectious diseases in North America: the road ahead. CMAJ. 2008; 178(6):715–722. PMID: 18332386.18. Altizer S, Dobson A, Hosseini P, Hudson P, Pascual M, Rohani P. Seasonality and the dynamics of infectious diseases. Ecol Lett. 2006; 9(4):467–484. PMID: 16623732.
Article19. Seemungal T, Harper-Owen R, Bhowmik A, Moric I, Sanderson G, Message S, et al. Respiratory viruses, symptoms, and inflammatory markers in acute exacerbations and stable chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001; 164(9):1618–1623. PMID: 11719299.
Article20. Wark PA, Johnston SL, Moric I, Simpson JL, Hensley MJ, Gibson PG. Neutrophil degranulation and cell lysis is associated with clinical severity in virus-induced asthma. Eur Respir J. 2002; 19(1):68–75. PMID: 11852895.
Article21. Wedzicha JA. Role of viruses in exacerbations of chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2004; 1(2):115–120. PMID: 16113423.
Article22. Widmer K, Zhu Y, Williams JV, Griffin MR, Edwards KM, Talbot HK. Rates of hospitalizations for respiratory syncytial virus, human metapneumovirus, and influenza virus in older adults. J Infect Dis. 2012; 206(1):56–62. PMID: 22529314.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Roflumilast in Bronchiectasis Patients with Frequent Exacerbations: A Double-Blinded, Randomized, Placebo-Controlled Pilot Clinical Trial
- New Tread of Association of Rhinovirus and Asthma
- Viral Infections and Associated Factors That Promote Acute Exacerbations of Asthma
- Prevalence of respiratory viral infection in children hospitalized for acute lower respiratory tract diseases, and association of rhinovirus and influenza virus with asthma exacerbations
- Infection Frequency and Mixed infection on Eight Viruses from Patients with Acute Respiratory Syndromes in Seoul