Acute Crit Care.
2021 Aug;36(3):249-255. 10.4266/acc.2020.01102.
Effects of high-flow nasal cannula in patients with mild to moderate hypercapnia: a prospective observational study
- Affiliations
-
- 1Department of Medicine, Ajou University Intermediate Care Hospital, Suwon, Korea
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
- 3Department of Pulmonary and Critical Care Medicine, Kyung Hee University Hospital at Gangdong, Seoul, Korea
- 4Department of Pulmonology, Ewha Womans University Seoul Hospital, Seoul, Korea
- 5Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 6Intensive Care Nursing Team, Asan Medical Center, Seoul, Korea
- 7Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2519452
- DOI: http://doi.org/10.4266/acc.2020.01102
Abstract
- Background
Evidence for using high-flow nasal cannula (HFNC) in hypercapnia is still limited. Most of the clinical studies had been conducted retrospectively, and there had been conflicting reports for the effects of HFNC on hypercapnia correction in prospective studies. Therefore, more evidence is needed to understand the effect of the HFNC in hypercapnia.
Methods
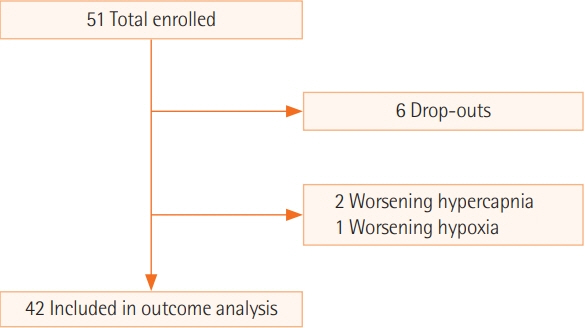
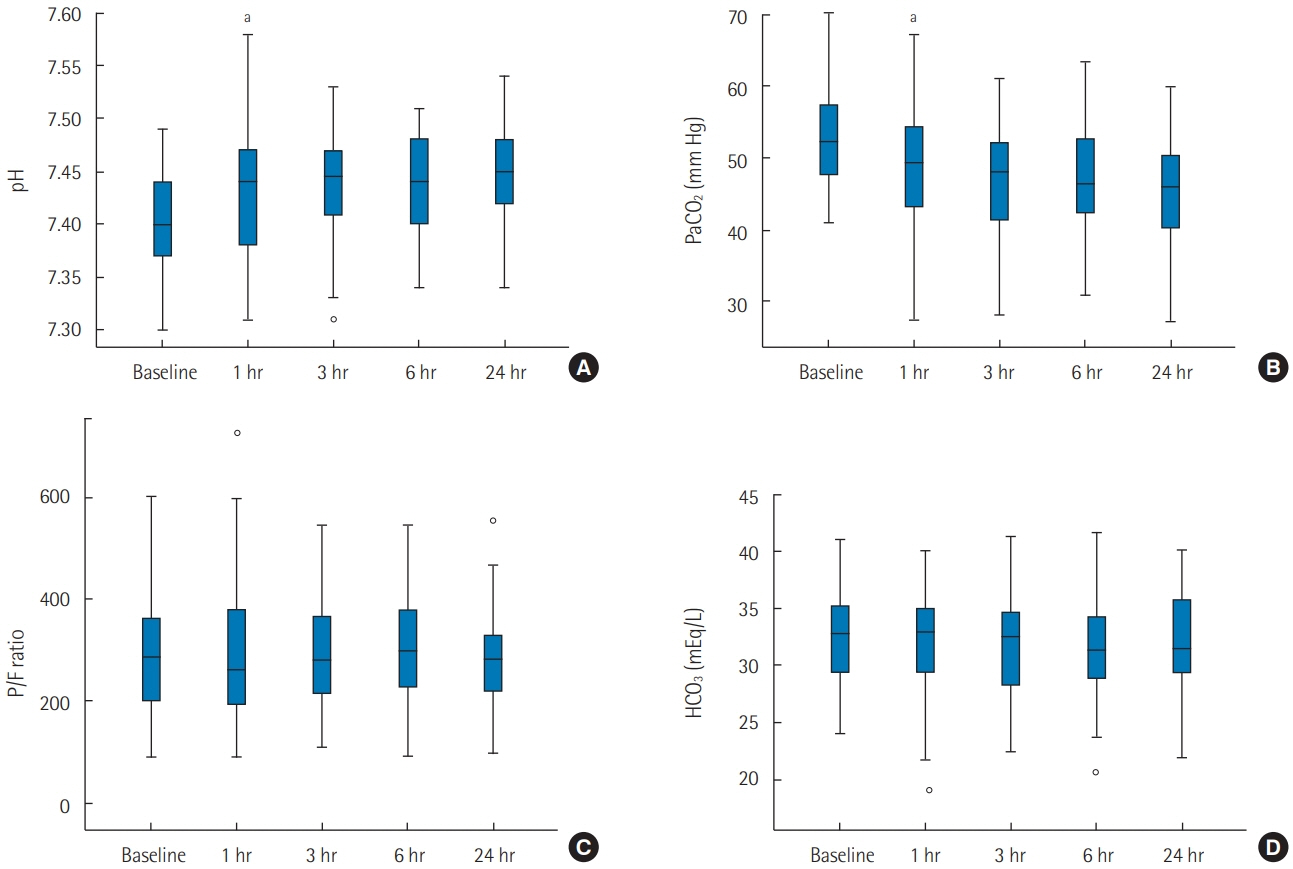
We conducted a multicenter prospective observational study after applying HFNC to 45 hospitalized subjects who had moderate hypercapnia (arterial partial pressure of carbon dioxide [PaCO2], 43–70 mm Hg) without severe respiratory acidosis (pH <7.30). The primary outcome was a change in PaCO2 level in the first 24 hours of HFNC use. The secondary outcomes were changes in other parameters of arterial blood gas analysis, changes in respiration rates, and clinical outcomes.
Results
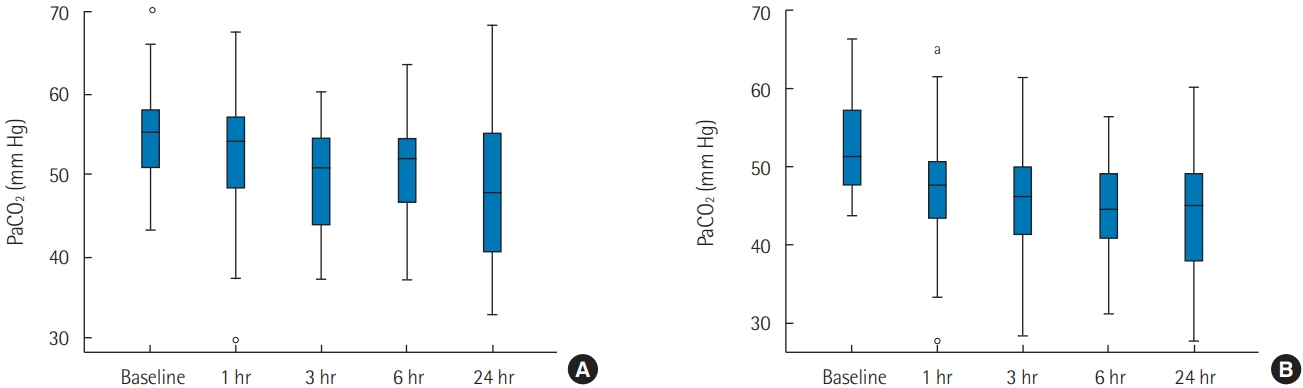
There was a significant decrease in PaCO2 in the first hour of HFNC application (-3.80 mm Hg; 95% confidence interval, -6.35 to -1.24; P<0.001). Reduction of PaCO2 was more prominent in subjects who did not have underlying obstructive lung disease. There was a correction in pH, but no significant changes in respiratory rate, bicarbonate, and arterial partial pressure of oxygen/fraction of inspired oxygen ratio. Mechanical ventilation was not required for 93.3% (42/45) of our study population.
Conclusions
We suggest that HFNC could be a safe alternative for oxygen delivery in hypercapnia patients who do not need immediate mechanical ventilation. With HFNC oxygenation, correction of hypercapnia could be expected, especially in patients who do not have obstructive lung diseases.
Figure
Reference
-
1. Drake MG. High-flow nasal cannula oxygen in adults: an evidence-based assessment. Ann Am Thorac Soc. 2018; 15:145–55.
Article2. Möller W, Celik G, Feng S, Bartenstein P, Meyer G, Oliver E, et al. Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol (1985). 2015; 118:1525–32.
Article3. Bräunlich J, Goldner F, Wirtz H. Nasal highflow eliminates CO2 from lower airways. Respir Physiol Neurobiol. 2017; 242:86–8.4. Biselli PJ, Kirkness JP, Grote L, Fricke K, Schwartz AR, Smith P, et al. Nasal high-flow therapy reduces work of breathing compared with oxygen during sleep in COPD and smoking controls: a prospective observational study. J Appl Physiol (1985). 2017; 122:82–8.
Article5. Patel A, Nouraei SA. Transnasal humidified rapid-insufflation ventilatory exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia. 2015; 70:323–9.
Article6. Jeong JH, Kim DH, Kim SC, Kang C, Lee SH, Kang TS, et al. Changes in arterial blood gases after use of high-flow nasal cannula therapy in the ED. Am J Emerg Med. 2015; 33:1344–9.
Article7. Kim ES, Lee H, Kim SJ, Park J, Lee YJ, Park JS, et al. Effectiveness of high-flow nasal cannula oxygen therapy for acute respiratory failure with hypercapnia. J Thorac Dis. 2018; 10:882–8.
Article8. Sztrymf B, Messika J, Mayot T, Lenglet H, Dreyfuss D, Ricard JD. Impact of high-flow nasal cannula oxygen therapy on intensive care unit patients with acute respiratory failure: a prospective observational study. J Crit Care. 2012; 27:324.e9–13.
Article9. Frat JP, Thille AW, Mercat A, Girault C, Ragot S, Perbet S, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015; 372:2185–96.
Article10. Rochwerg B, Granton D, Wang DX, Helviz Y, Einav S, Frat JP, et al. High flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: a systematic review and meta-analysis. Intensive Care Med. 2019; 45:563–72.
Article11. Nilius G, Franke KJ, Domanski U, Rühle KH, Kirkness JP, Schneider H. Effects of nasal insufflation on arterial gas exchange and breathing pattern in patients with chronic obstructive pulmonary disease and hypercapnic respiratory failure. Adv Exp Med Biol. 2013; 755:27–34.
Article12. Roussos C, Koutsoukou A. Respiratory failure. Eur Respir J Suppl. 2003; 47:3s–14s.
Article13. Davidson AC, Banham S, Elliott M, Kennedy D, Gelder C, Glossop A. BTS/ICS guideline for the ventilatory management of acute hypercapnic respiratory failure in adults. Thorax. 2016; 71 Suppl 2:ii1–35.
Article14. Papachatzakis Y, Nikolaidis PT, Kontogiannis S, Trakada G. High-flow oxygen through nasal cannula vs. non-invasive ventilation in hypercapnic respiratory failure: a randomized clinical trial. Int J Environ Res Public Health. 2020; 17:5994.
Article15. Lee MK, Choi J, Park B, Kim B, Lee SJ, Kim SH, et al. High flow nasal cannulae oxygen therapy in acute-moderate hypercapnic respiratory failure. Clin Respir J. 2018; 12:2046–56.
Article16. Huang Y, Lei W, Zhang W, Huang JA. High-flow nasal cannula in hypercapnic respiratory failure: a systematic review and meta-analysis. Can Respir J. 2020; 2020:7406457.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Study on the Changes of SaO2, According to the Different Type of Oxygen Suppliers
- High-flow nasal cannula oxygen therapy in children: a clinical review
- Reduction of PaCOâ‚‚ by high-flow nasal cannula in acute hypercapnic respiratory failure patients receiving conventional oxygen therapy
- Factors about Failure after High Flow Oxygen through Nasal Cannula Therapy in Hypoxic Respiratory Failure Patients at Emergency Department Presentation
- High-Flow Nasal Cannula Oxygen Therapy Can Be Effective for Patients in Acute Hypoxemic Respiratory Failure with Hypercapnia: a Retrospective, Propensity Score-Matched Cohort Study