Ann Hepatobiliary Pancreat Surg.
2021 Aug;25(3):408-413. 10.14701/ahbps.2021.25.3.408.
Funneling venoplasty for anomalous graft left hepatic vein in living donor liver transplantation using a split left lateral section graft for an infant patient
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2519300
- DOI: http://doi.org/10.14701/ahbps.2021.25.3.408
Abstract
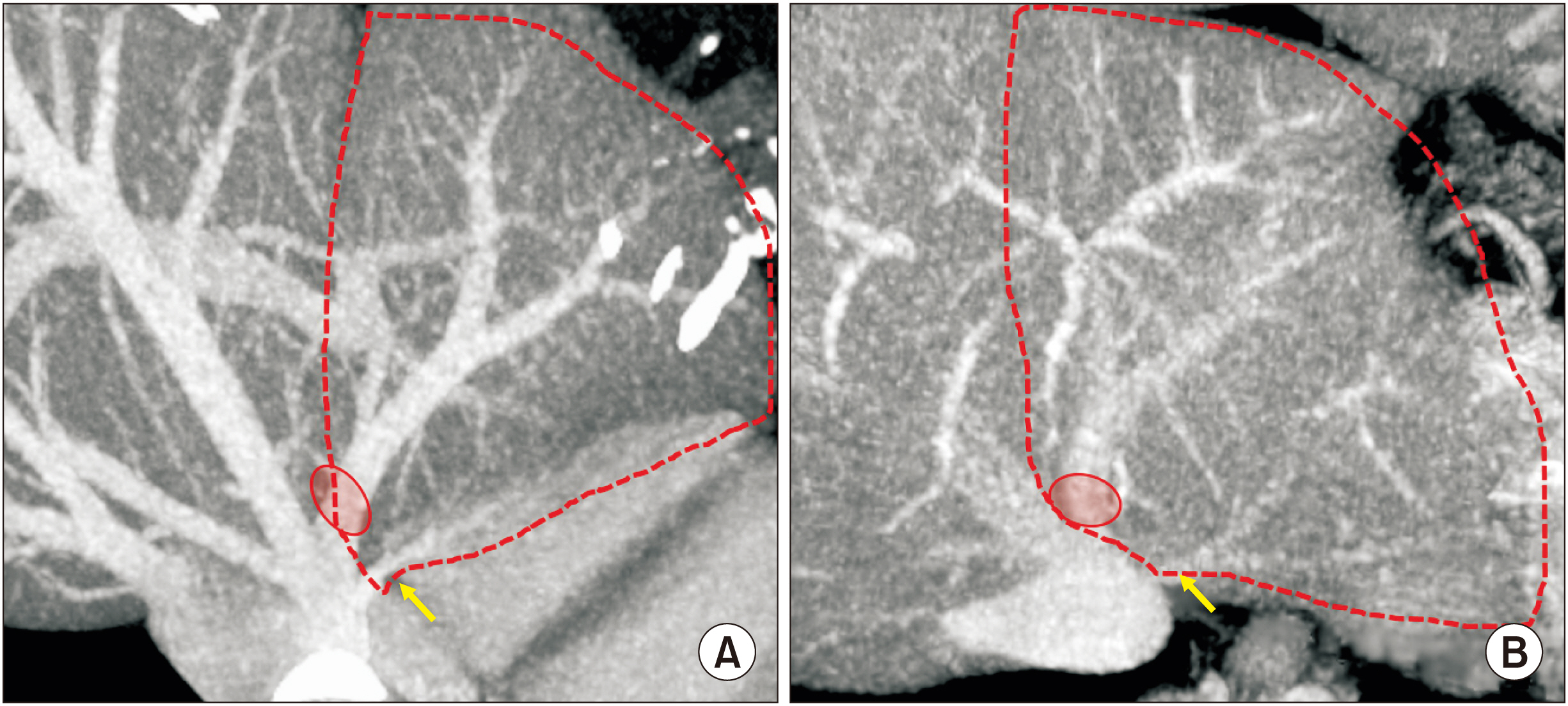
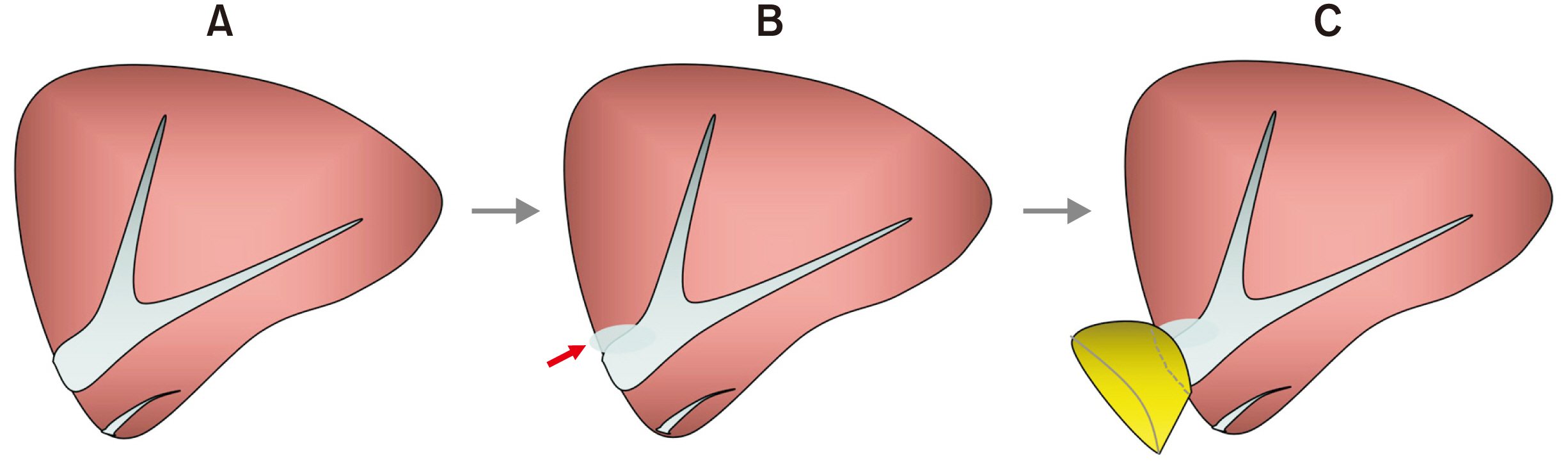
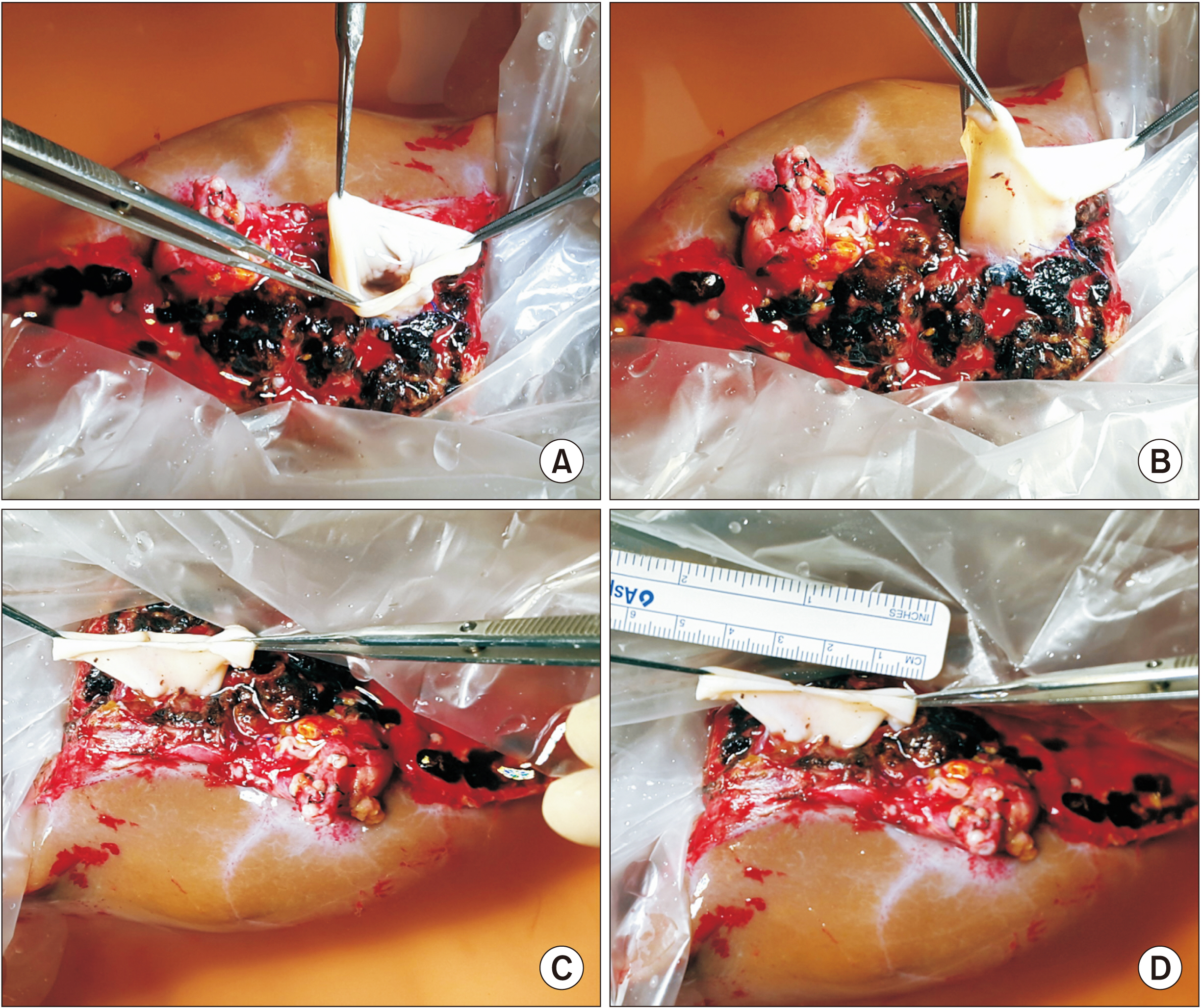
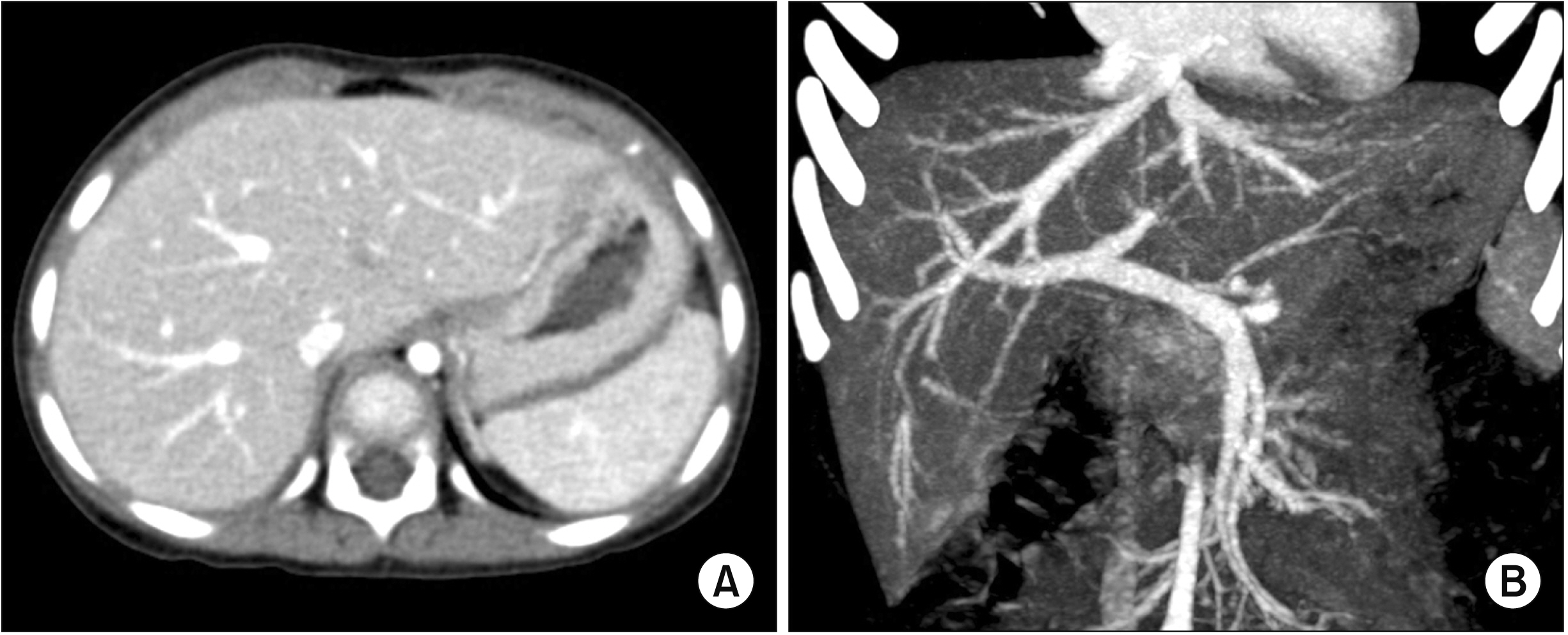
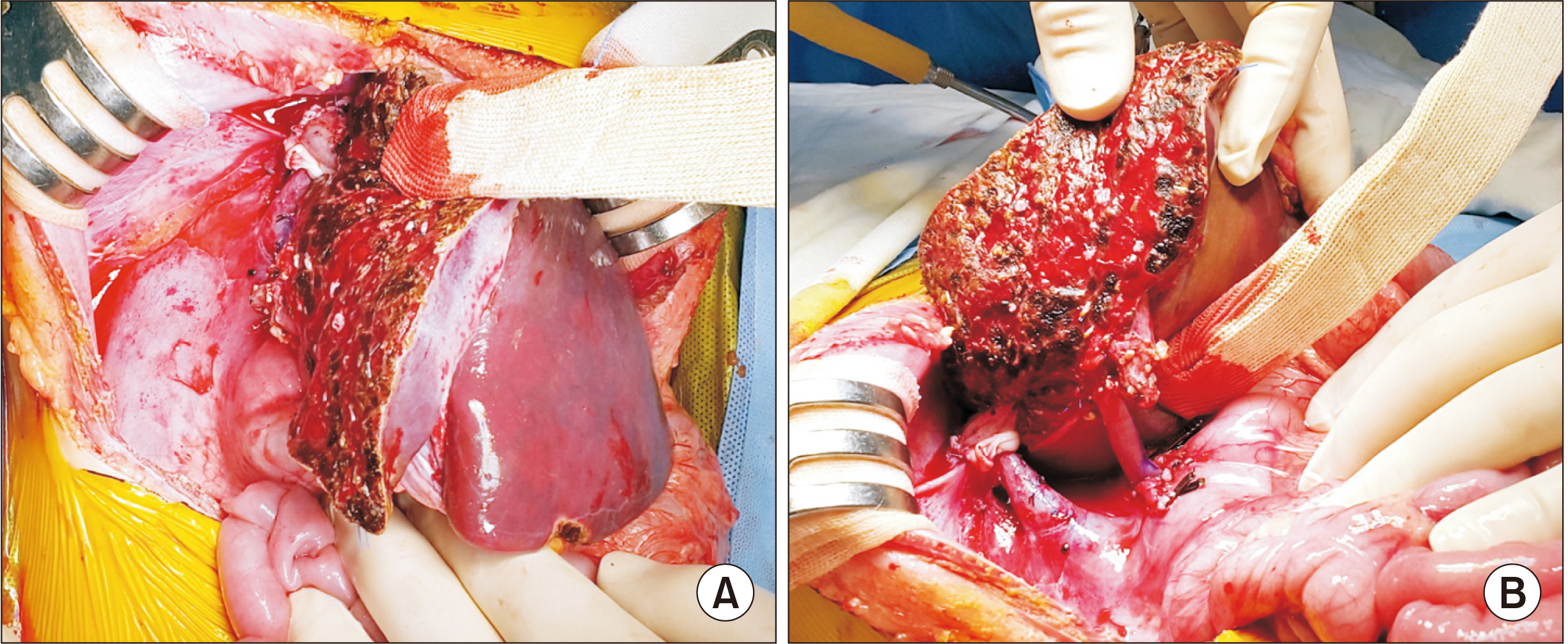
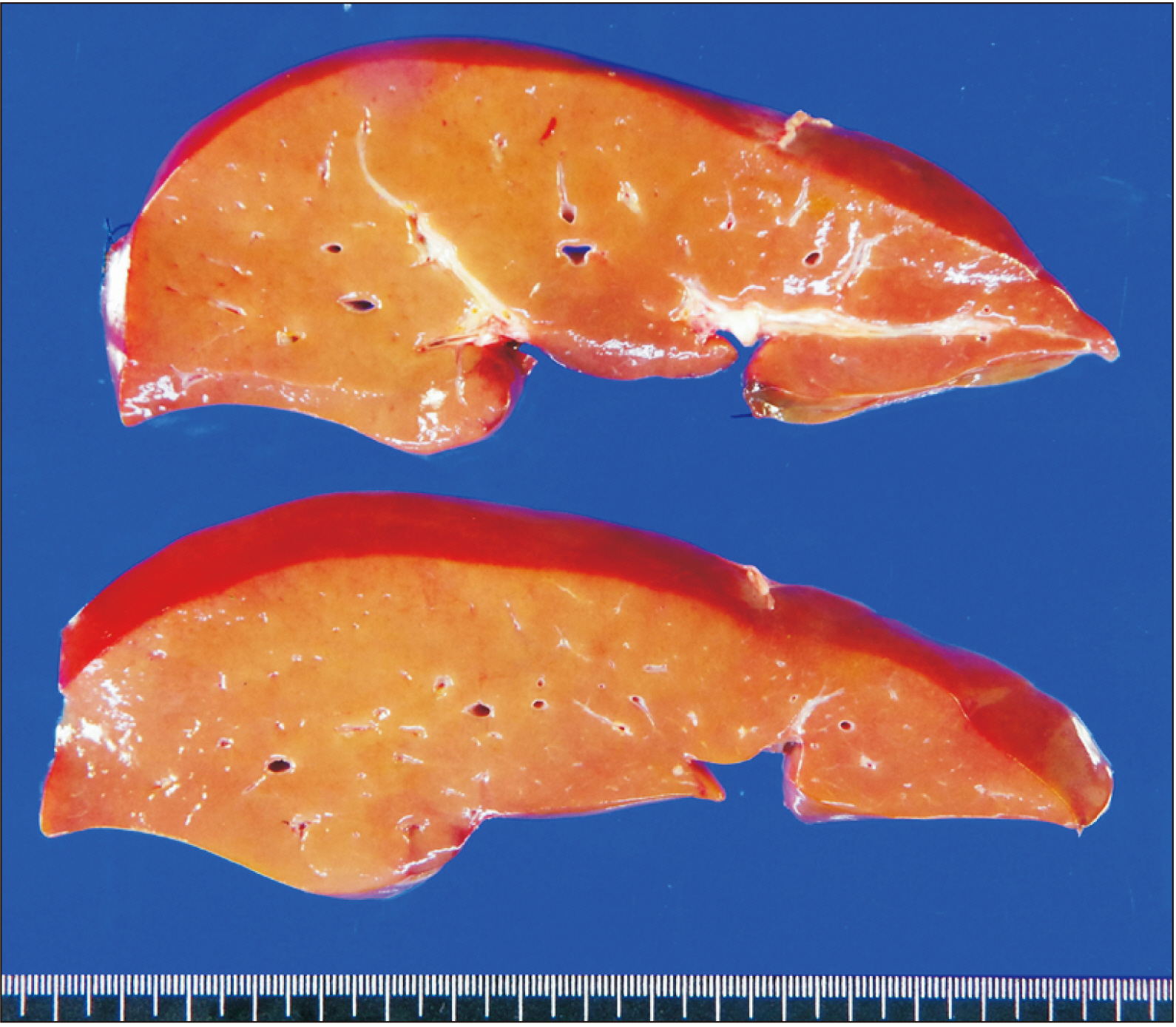
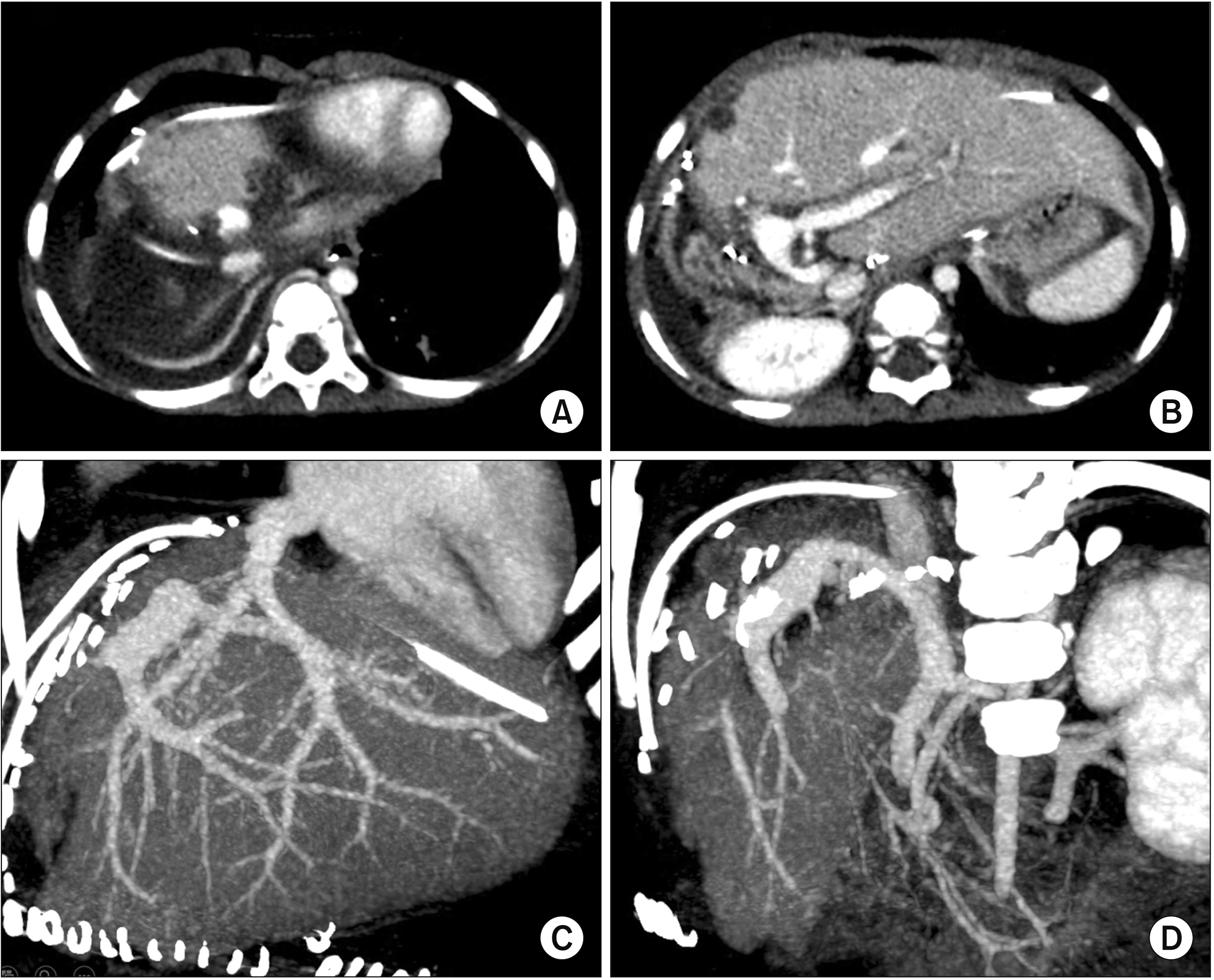
- The left lateral section (LLS) can have an unusual variant left hepatic vein (LHV) anatomy. We present a case of customized funneling venoplasty of the graft LHV in a 22-month-old girl diagnosed with ornithine transcarbamylase deficiency undergoing deceased donor liver transplantation (LT) using a split LLS graft. The split LLS graft weighed 350 g, yielding a graft-to-recipient weight ratio of 3.2%.Notably, the graft LHV opening was located at the graft liver cut surface, which was only 1 cm in size and 2 cm away from the cephalad apex of the LLS graft. Since such a variant location of the small LHV opening was unsuitable for direct anastomosis, we performed a funneling venoplasty using an inferior vena cava fragment homograft obtained from the same donor. The graft implantation was performed according to standard procedures of infant split LT. Follow-up imaging studies showed no vascular complications. The patient recovered uneventfully from the LT operation. She had normal blood test findings, including normal ammonia level. She has been doing well for 6 months after the transplantation. In conclusion, our surgical technique using a funneling venoplasty enabled successful reconstruction of the anomalous graft LHV. Our results suggest that individualized reconstruction techniques should be applied to infant patients undergoing LT using a LLS graft with variant types of graft LHV anatomy.
Keyword
Figure
Cited by 1 articles
-
Modified left liver graft with funneling venoplasty of middle hepatic vein branches for pediatric living donor liver transplantation
Jung-Man Namgoong, Gil-Chun Park, Shin Hwang, Sang-Hoon Kim, Suhyeon Ha, Kyung Mo Kim, Seak Hee Oh
Ann Liver Transplant. 2023;3(1):44-49. doi: 10.52604/alt.23.0002.
Reference
-
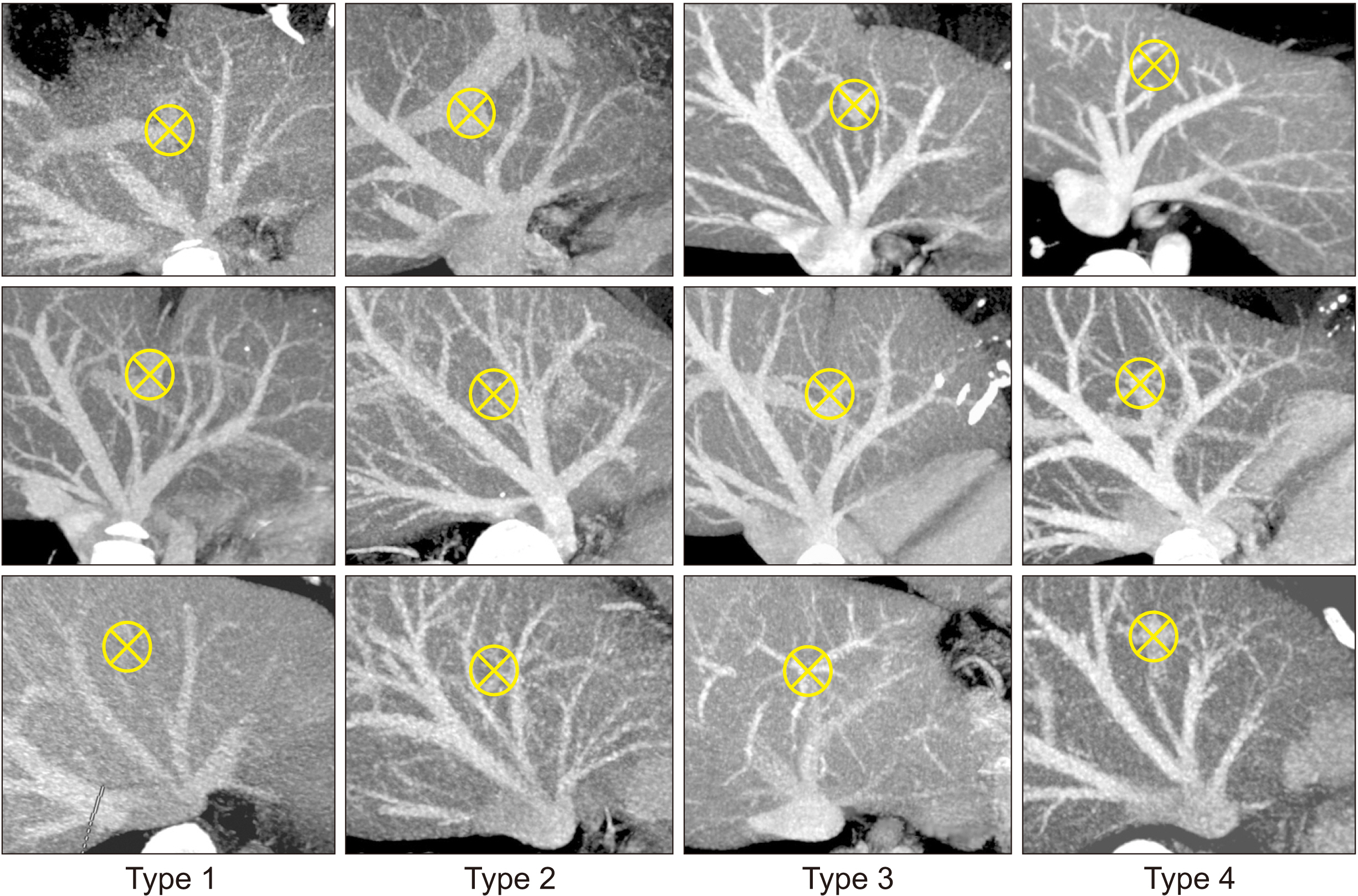
1. Hwang S, Kim KH, Kim DY, Kim KM, Ahn CS, Moon DB, et al. 2013; Anomalous hepatic vein anatomy of left lateral section grafts and customized unification venoplasty for pediatric living donor liver transplantation. Liver Transpl. 19:184–190. DOI: 10.1002/lt.23557. PMID: 23045153.
Article2. Hwang S, Lee SG, Choi ST, Moon DB, Ha TY, Lee YJ, et al. 2005; Hepatic vein anatomy of the medial segment for living donor liver transplantation using extended right lobe graft. Liver Transpl. 11:449–455. DOI: 10.1002/lt.20387. PMID: 15776411.
Article3. Radtke A, Sotiropoulos GC, Sgourakis G, Molmenti EP, Schroeder T, Saner FH, et al. 2010; Hepatic venous drainage: how much can we learn from imaging studies? Anatomic-functional classification derived from three-dimensional computed tomography reconstructions. Transplantation. 89:1518–1525. DOI: 10.1097/TP.0b013e3181dd6bac. PMID: 20410853.
Article4. Mochizuki K, Takatsuki M, Soyama A, Hidaka M, Obatake M, Eguchi S. 2012; The usefulness of a high-speed 3D-image analysis system in pediatric living donor liver transplantation. Ann Transplant. 17:31–34. DOI: 10.12659/AOT.882633. PMID: 22466906.
Article5. Hwang S, Lee SG, Lee YJ, Park KM, Ahn CS, Kim KH. 2006; Postoperative changes in remnant medial segment parenchyma of living donor livers after procurement of left lateral segment graft. Hepatogastroenterology. 53:773–777. PMID: 17086886.6. Seda-Neto J, Godoy AL, Carone E, Pugliese V, Fonseca EA, Porta G, et al. 2008; Left lateral segmentectomy for pediatric live-donor liver transplantation: special attention to segment IV complications. Transplantation. 86:697–701. DOI: 10.1097/TP.0b013e318183ed22. PMID: 18791451.
Article7. Namgoong JM, Hwang S, Park GC, Ahn CS, Kim KH, Kim KM, et al. 2021; Outflow vein venoplasty of left lateral section graft for living donor liver transplantation in infant recipients. Pediatr Transplant. 25:e13970. DOI: 10.1111/petr.13970. PMID: 33433048.
Article8. Galloux A, Pace E, Franchi-Abella S, Branchereau S, Gonzales E, Pariente D. 2018; Diagnosis, treatment and outcome of hepatic venous outflow obstruction in paediatric liver transplantation: 24-year experience at a single centre. Pediatr Radiol. 48:667–679. DOI: 10.1007/s00247-018-4079-y. PMID: 29468367.
Article9. Katano T, Sanada Y, Hirata Y, Yamada N, Okada N, Onishi Y, et al. 2019; Endovascular stent placement for venous complications following pediatric liver transplantation: outcomes and indications. Pediatr Surg Int. 35:1185–1195. DOI: 10.1007/s00383-019-04551-9. PMID: 31535198.
Article10. Zhang ZY, Jin L, Chen G, Su TH, Zhu ZJ, Sun LY, et al. 2017; Balloon dilatation for treatment of hepatic venous outflow obstruction following pediatric liver transplantation. World J Gastroenterol. 23:8227–8234. DOI: 10.3748/wjg.v23.i46.8227. PMID: 29290659. PMCID: PMC5739929.
Article11. Lu KT, Cheng YF, Chen TY, Tsang LC, Ou HY, Yu CY, et al. 2018; Efficiency of transluminal angioplasty of hepatic venous outflow obstruction in pediatric liver transplantation. Transplant Proc. 50:2715–2717. DOI: 10.1016/j.transproceed.2018.04.022. PMID: 30401383.
Article12. Yeh YT, Chen CY, Tseng HS, Wang HK, Tsai HL, Lin NC, et al. 2017; Enlarging vascular stents after pediatric liver transplantation. J Pediatr Surg. 52:1934–1939. DOI: 10.1016/j.jpedsurg.2017.08.060. PMID: 28927979.
Article13. Namgoong JM, Hwang S, Yoon YI, Cho YP, Kang WH, Kwon YJ, et al. 2021; Third retransplantation using a whole liver graft for late graft failure from hepatic vein stent stenosis in a pediatric patient who underwent split liver retransplantation. Ann Hepatobiliary Pancreat Surg. 25:299–306. DOI: 10.14701/ahbps.2021.25.2.299. PMID: 34053936. PMCID: PMC8180402.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tailored techniques of graft outflow vein reconstruction in pediatric liver transplantation at Asan Medical Center
- Modified left liver graft with funneling venoplasty of middle hepatic vein branches for pediatric living donor liver transplantation
- Graft outflow vein unification venoplasty with superficial left hepatic vein branch in pediatric living donor liver transplantation using a left lateral section graft
- Graft outflow vein venoplasty for a laparoscopically harvested left lateral section graft in pediatric living donor liver transplantation
- Outflow vein venoplasty of left lateral section graft for living donor liver transplantation in infant recipients