Clin Exp Otorhinolaryngol.
2021 Aug;14(3):312-320. 10.21053/ceo.2020.02369.
Predictive Value of Olfactory and Taste Symptoms in the Diagnosis of COVID-19: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Department of Physiology and Biomedical Engineering, Mayo Clinic, Rochester, MN, USA
- 3Department of Otolaryngology-Head and Neck Surgery, Bucheon St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2519186
- DOI: http://doi.org/10.21053/ceo.2020.02369
Abstract
Objectives
. This study evaluated the diagnostic value of various symptoms of coronavirus disease 2019 (COVID-19) in screening for this disease.
Methods
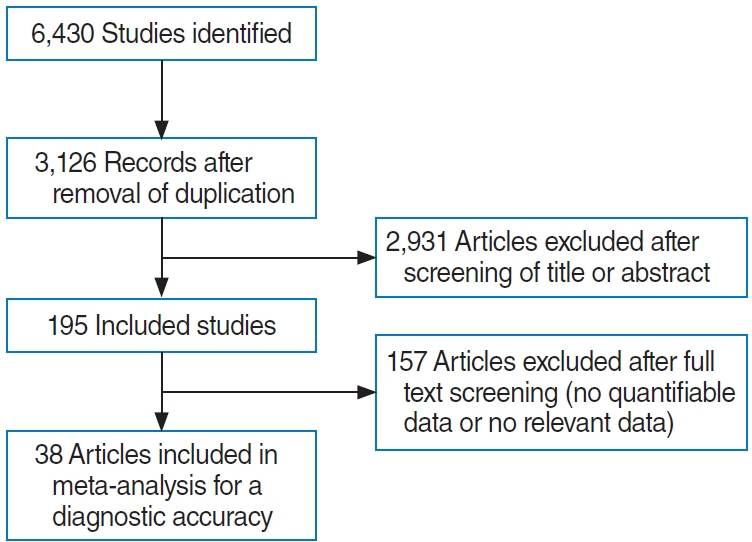
. Two authors (working independently) comprehensively reviewed six databases (PubMed, Cochrane Database, Embase, Web of Science, Scopus, and Google Scholar) from their dates of inception until November 2020. The predictive value of patient-reported symptoms, including otolaryngologic and general symptoms, was evaluated in adults who underwent testing for COVID-19. True-positive, true-negative, false-positive, and false-negative data were extracted from each study. The methodological quality of the included studies was evaluated using the quality assessment of diagnostic accuracy studies tool (ver. 2).
Results
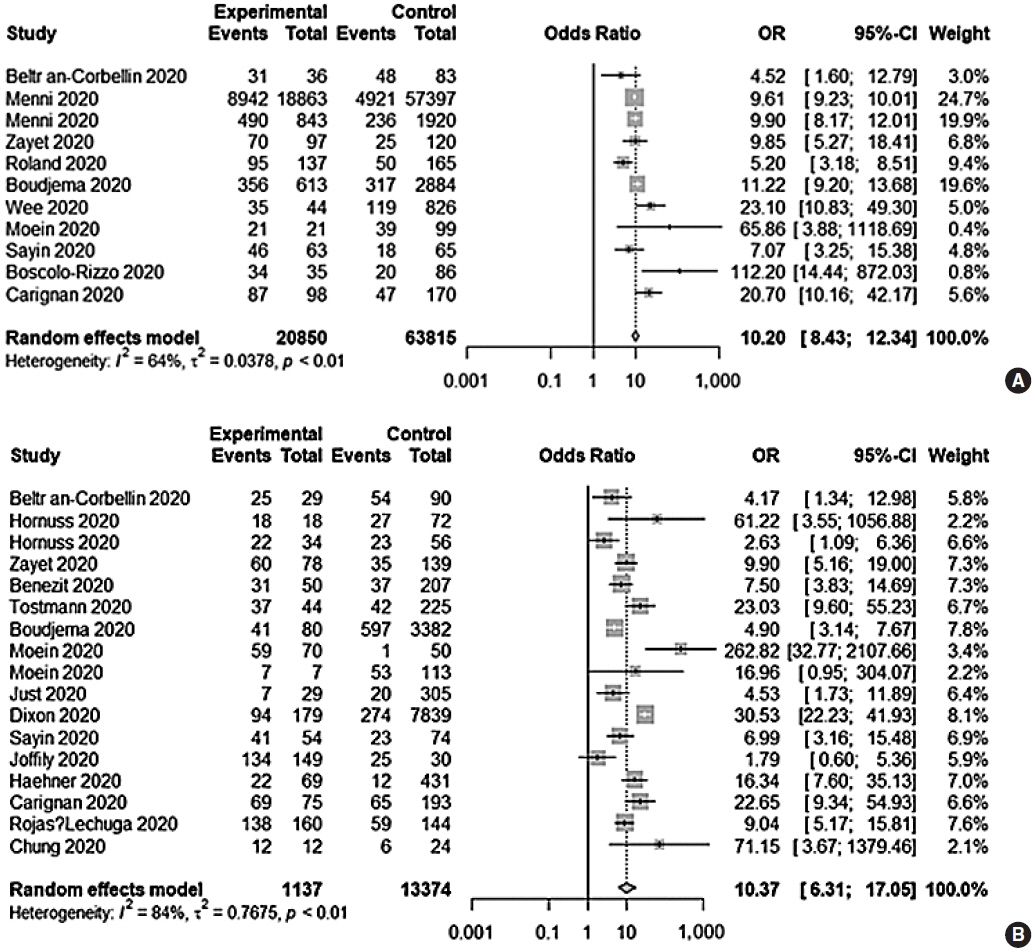
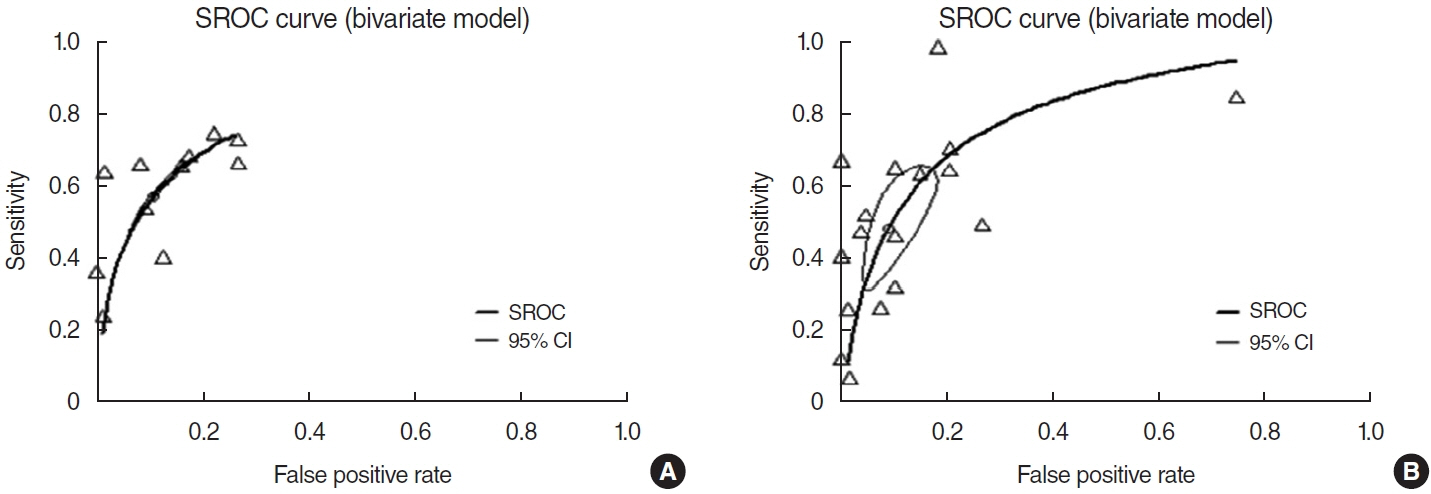
. Twenty-eight prospective and retrospective studies were included in the meta-analysis. The diagnostic odds ratio (DOR) of a change in olfaction and/or taste was 10.20 (95% confidence interval [CI], 8.43–12.34). The area under the summary receiver operating characteristic curve was 0.8. Olfactory and/or taste changes had a low sensitivity (0.57; 95% CI, 0.47–0.66) but moderate negative (0.78; 95% CI, 0.69–0.85] and positive (0.78; 95% CI, 0.66–0.87) predictive values and a high specificity (0.91; 95% CI, 0.83–0.96). Olfactory and/or taste changes had a higher diagnostic value than the other otolaryngologic symptoms, a higher DOR and specificity, and a similar or higher diagnostic value than the other general symptoms.
Conclusion
. Among otolaryngologic symptoms, olfactory and/or taste dysfunction was the most closely associated with COVID-19 and its general symptoms, and should therefore be considered when screening for the disease.
Figure
Cited by 1 articles
-
Practical Review of Olfactory Training and COVID-19
Se Hwan Hwang, Ji-Sun Kim, Bo Yoon Choi, Jin Kook Kim, Byung Guk Kim
J Rhinol. 2022;29(3):127-133. doi: 10.18787/jr.2022.00407.
Reference
-
1. Joffily L, Ungierowicz A, David AG, Melo B, Brito CL, Mello L, et al. The close relationship between sudden loss of smell and COVID-19. Braz J Otorhinolaryngol. 2020; Sep-Oct. 86(5):632–8.
Article2. Zayet S, Klopfenstein T, Mercier J, Kadiane-Oussou NJ, Lan Cheong Wah L, Royer PY, et al. Contribution of anosmia and dysgeusia for diagnostic of COVID-19 in outpatients. Infection. 2021; Apr. 49(2):361–5.
Article3. Yan CH, Faraji F, Prajapati DP, Boone CE, DeConde AS. Association of chemosensory dysfunction and COVID-19 in patients presenting with influenza-like symptoms. Int Forum Allergy Rhinol. 2020; Jul. 10(7):806–13.
Article4. Sayin I, Yazici ZM. Taste and smell impairment in SARS-CoV-2 recovers early and spontaneously: experimental data strongly linked to clinical data. ACS Chem Neurosci. 2020; Jul. 11(14):2031–3.
Article5. Roland LT, Gurrola JG 2nd, Loftus PA, Cheung SW, Chang JL. Smell and taste symptom-based predictive model for COVID-19 diagnosis. Int Forum Allergy Rhinol. 2020; Jul. 10(7):832–8.
Article6. Benezit F, Le Turnier P, Declerck C, Paille C, Revest M, Dubee V, et al. Utility of hyposmia and hypogeusia for the diagnosis of COVID-19. Lancet Infect Dis. 2020; Sep. 20(9):1014–5.7. Park JH, Jang W, Kim SW, Lee J, Lim YS, Cho CG, et al. The clinical manifestations and chest computed tomography findings of coronavirus disease 2019 (COVID-19) patients in china: a proportion meta-analysis. Clin Exp Otorhinolaryngol. 2020; May. 13(2):95–105.8. Kim SY, Kim DW. Does the clinical spectrum of coronavirus disease 2019 (COVID-19) show regional differences? Clin Exp Otorhinolaryngol. 2020; May. 13(2):83–4.
Article9. Menni C, Valdes AM, Freidin MB, Sudre CH, Nguyen LH, Drew DA, et al. Real-time tracking of self-reported symptoms to predict potential COVID-19. Nat Med. 2020; Jul. 26(7):1037–40.
Article10. Beltran-Corbellini A, Chico-Garcia JL, Martinez-Poles J, RodriguezJorge F, Natera-Villalba E, Gomez-Corral J, et al. Acute-onset smell and taste disorders in the context of COVID-19: a pilot multicentre polymerase chain reaction based case-control study. Eur J Neurol. 2020; Sep. 27(9):1738–41.
Article11. Just J, Puth MT, Regenold F, Weckbecker K, Bleckwenn M. Risk factors for a positive SARS-CoV-2 PCR in patients with common cold symptoms in a primary care setting: a retrospective analysis based on a joint documentation standard. BMC Fam Pract. 2020; Dec. 21(1):251.
Article12. Boudjema S, Finance J, Coulibaly F, Meddeb L, Tissot-Dupont H, Michel M, et al. Olfactory and gustative disorders for the diagnosis of COVID-19. Travel Med Infect Dis. 2020; Sep-Oct. 37:101875.
Article13. Clemency BM, Varughese R, Scheafer DK, Ludwig B, Welch JV, McCormack RF, et al. Symptom criteria for COVID-19 testing of heath care workers. Acad Emerg Med. 2020; Jun. 27(6):469–74.
Article14. Dixon BE, Wools-Kaloustian KK, Fadel WF, Duszynski TJ, Yiannoutsos C, Halverson PK, et al. Symptoms and symptom clusters associated with SARS-CoV-2 infection in community-based populations: Results from a statewide epidemiological study. PLoS One. 2021; Mar. 16(3):e0241875.
Article15. Haehner A, Draf J, Drager S, de With K, Hummel T. Predictive value of sudden olfactory loss in the diagnosis of COVID-19. ORL J Otorhinolaryngol Relat Spec. 2020; 82(4):175–80.
Article16. Hornuss D, Lange B, Schroter N, Rieg S, Kern WV, Wagner D. Anosmia in COVID-19 patients. Clin Microbiol Infect. 2020; Oct. 26(10):1426–7.
Article17. Jiang J, Wan R, Pan P, Hu C, Zhou R, Yin Y, et al. Comparison of clinical, laboratory and radiological characteristics between COVID-19 and adenovirus pneumonia: a retrospective study. Infect Drug Resist. 2020; Oct. 13:3401–8.18. Menni C, Sudre CH, Steves CJ, Ourselin S, Spector TD. Quantifying additional COVID-19 symptoms will save lives. Lancet. 2020; Jun. 395(10241):e107–8.
Article19. Moein ST, Hashemian SM, Mansourafshar B, Khorram-Tousi A, Tabarsi P, Doty RL. Smell dysfunction: a biomarker for COVID-19. Int Forum Allergy Rhinol. 2020; Aug. 10(8):944–50.
Article20. Tong JY, Wong A, Zhu D, Fastenberg JH, Tham T. The Prevalence of olfactory and gustatory dysfunction in COVID-19 patients: a systematic review and meta-analysis. Otolaryngol Head Neck Surg. 2020; Jul. 163(1):3–11.
Article21. Tostmann A, Bradley J, Bousema T, Yiek WK, Holwerda M, Bleeker-Rovers C, et al. Strong associations and moderate predictive value of early symptoms for SARS-CoV-2 test positivity among healthcare workers, the Netherlands, March 2020. Euro Surveill. 2020; Apr. 25(16):2000508.
Article22. Wee LE, Chan YF, Teo NW, Cherng BP, Thien SY, Wong HM, et al. The role of self-reported olfactory and gustatory dysfunction as a screening criterion for suspected COVID-19. Eur Arch Otorhinolaryngol. 2020; Aug. 277(8):2389–90.
Article23. Zhao D, Yao F, Wang L, Zheng L, Gao Y, Ye J, et al. A comparative study on the clinical features of coronavirus 2019 (COVID-19) pneumonia with other pneumonias. Clin Infect Dis. 2020; Jul. 71(15):756–61.
Article24. Zhu W, Xie K, Lu H, Xu L, Zhou S, Fang S. Initial clinical features of suspected coronavirus disease 2019 in two emergency departments outside of Hubei, China. J Med Virol. 2020; Sep. 92(9):1525–32.
Article25. Cheng Z, Lu Y, Cao Q, Qin L, Pan Z, Yan F, et al. Clinical features and chest CT manifestations of coronavirus disease 2019 (COVID-19) in a single-center study in Shanghai, China. AJR Am J Roentgenol. 2020; Jul. 215(1):121–6.
Article26. Sun Y, Koh V, Marimuthu K, Ng OT, Young B, Vasoo S, et al. Epidemiological and clinical predictors of COVID-19. Clin Infect Dis. 2020; Jul. 71(15):786–92.
Article27. Tolia VM, Chan TC, Castillo EM. Preliminary results of initial testing for coronavirus (COVID-19) in the emergency department. West J Emerg Med. 2020; Mar. 21(3):503–6.
Article28. Peng L, Liu KY, Xue F, Miao YF, Tu PA, Zhou C. Improved early recognition of coronavirus disease-2019 (COVID-19): single-center data from a shanghai screening hospital. Arch Iran Med. 2020; Apr. 23(4):272–6.
Article29. Nobel YR, Phipps M, Zucker J, Lebwohl B, Wang TC, Sobieszczyk ME, et al. Gastrointestinal symptoms and coronavirus disease 2019: a case-control study from the United States. Gastroenterology. 2020; Jul. 159(9):373–5.e2.30. Chen X, Tang Y, Mo Y, Li S, Lin D, Yang Z, et al. A diagnostic model for coronavirus disease 2019 (COVID-19) based on radiological semantic and clinical features: a multi-center study. Eur Radiol. 2020; Sep. 30(9):4893–902.
Article31. Boscolo-Rizzo P, Borsetto D, Spinato G, Fabbris C, Menegaldo A, Gaudioso P, et al. New onset of loss of smell or taste in household contacts of home-isolated SARS-CoV-2-positive subjects. Eur Arch Otorhinolaryngol. 2020; Sep. 277(9):2637–40.
Article32. Carignan A, Valiquette L, Grenier C, Musonera JB, Nkengurutse D, Marcil-Heguy A, et al. Anosmia and dysgeusia associated with SARSCoV-2 infection: an age-matched case-control study. CMAJ. 2020; Jun. 192(26):E702–7.
Article33. Chung TW, Sridhar S, Zhang AJ, Chan KH, Li HL, Wong FK, et al. Olfactory dysfunction in coronavirus disease 2019 patients: observational cohort study and systematic review. Open Forum Infect Dis. 2020; Jun. 7(6):ofaa199.
Article34. Hoang MP, Kanjanaumporn J, Aeumjaturapat S, Chusakul S, Seresirikachorn K, Snidvongs K. Olfactory and gustatory dysfunctions in COVID-19 patients: a systematic review and meta-analysis. Asian Pac J Allergy Immunol. 2020; Sep. 38(3):162–9.
Article35. Rojas-Lechuga MJ, Izquierdo-Dominguez A, Chiesa-Estomba C, Calvo-Henriquez C, Villarreal IM, Cuesta-Chasco G, et al. Chemosensory dysfunction in COVID-19 out-patients. Eur Arch Otorhinolaryngol. 2021; Mar. 278(3):695–702.
Article36. Feng C, Wang L, Chen X, Zhai Y, Zhu F, Chen H, et al. A novel artificial intelligence-assisted triage tool to aid in the diagnosis of suspected COVID-19 pneumonia cases in fever clinics. Ann Transl Med. 2021; Feb. 9(3):201.
Article37. Song CY, Xu J, He JQ, Lu YQ. COVID-19 early warning score: a multi-parameter screening tool to identify highly suspected patients. medRxiv. 20031906 [Preprint]. 2020 [cited 2021 Mar 31]. Available from: https://doi.org/10.1101/2020.03.05.20031906.
Article38. Yang Z, Lin D, Chen X, Qiu J, Li S, Huang R, et al. Distinguishing COVID-19 from influenza pneumonia in the early stage through CT imaging and clinical features. medRxiv. 20061242 [Preprint]. 2020 [cited 2021 Mar 31]. Available from: https://doi.org/10.1101/2020.04.17.20061242.
Article39. Ai JW, Zhang HC, Xu T, Wu J, Zhu M, Yu YQ, et al. Optimizing diagnostic strategy for novel coronavirus pneumonia, a multi-center study in Eastern China. medRxiv. 20022673 [Preprint]. 2020 [cited 2021 Mar 31]. Available from: https://doi.org/10.1101/2020.02.13.20022673.
Article40. Rentsch CT, Kidwai-Khan F, Tate JP, Park LS, King JT, Skanderson M, et al. Covid-19 testing, hospital admission, and intensive care among 2,026,227 United States veterans aged 54-75 years. medRxiv. 2005-9964 [Preprint]. 2020 [cited 2021 Mar 31]. Available from: https://doi.org/10.1101/2020.04.09.20059964.
Article41. Liang Y, Liang J, Zhou Q, Li X, Lin F, Deng Z, et al. Prevalence and clinical features of 2019 novel coronavirus disease (COVID-19) in the Fever Clinic of a teaching hospital in Beijing: a single-center, retrospective study. medRxiv. 20027763 [Preprint]. 2020 [cited 2021 Mar 31]. Available from: https://doi.org/10.1101/2020.02.25.20027763.
Article42. Kim DH, Kim Y, Kim SW, Hwang SH. Use of narrowband imaging for the diagnosis and screening of laryngeal cancer: a systematic review and meta-analysis. Head Neck. 2020; Sep. 42(9):2635–43.
Article43. Vijayakumar V, Reghunathan D, Edacheriyan B, Mukundan A. Role of toluidine blue staining in suspicious lesions of oral cavity and oropharynx. Indian J Otolaryngol Head Neck Surg. 2019; Oct. 71(Suppl 1):142–6.
Article44. Trikalinos TA, Balion CM, Coleman CI, Griffith L, Santaguida PL, Vandermeer B, et al. AHRQ methods for effective health care metaanalysis of test performance when there is a “gold standard”. In : Chang SM, Matchar DB, Smetana GW, Umscheid CA, editors. Methods guide for medical test reviews. Rockville (MD): Agency for Healthcare Research and Quality (US);2012. p. 105–10.45. Trikalinos TA, Balion CM, Coleman CI, Griffith L, Santaguida PL, Vandermeer B, et al. Chapter 8: meta-analysis of test performance when there is a “gold standard”. J Gen Intern Med. 2012; Jun. 27 Suppl 1(Suppl 1):S56–66.
Article46. Yang J, Pinto JM. The epidemiology of olfactory disorders. Curr Otorhinolaryngol Rep. 2016; May. 4(2):130–41.
Article47. Hall A, Frauenfelder C, Butler C, Coyle P, Hopkins C. Paediatric olfactory dysfunction: a chance to detect COVID-19. Arch Dis Child. 2021; Mar. 106(3):e17.
Article48. von Bartheld CS, Hagen MM, Butowt R. Prevalence of chemosensory dysfunction in COVID-19 patients: a systematic review and metaanalysis reveals significant ethnic differences. ACS Chem Neurosci. 2020; Oct. 11(19):2944–61.
Article49. Borsetto D, Hopkins C, Philips V, Obholzer R, Tirelli G, Polesel J, et al. Self-reported alteration of sense of smell or taste in patients with COVID-19: a systematic review and meta-analysis on 3563 patients. Rhinology. 2020; Oct. 58(5):430–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Analysis of Olfactory and Gustatory Function of Patients With COVID-19 Olfactory Dysfunction and Non-COVID-19 Postinfectious Olfactory Dysfunction
- Contemporary Review of Olfactory Dysfunction in COVID-19
- Characteristics and Prognosis of COVID-19 Induced Olfactory and Gustatory Dysfunction in Daegu
- Regional and Chronological Variation of Chemosensory Dysfunction in COVID-19: a Meta-Analysis
- The Prevalence of Post-Traumatic Stress Disorder in the General Population during the COVID-19 Pandemic: A Systematic Review and Single-Arm Meta-Analysis