Clin Exp Otorhinolaryngol.
2021 Aug;14(3):278-286. 10.21053/ceo.2021.00325.
Hearing Impairment Increases Economic Inequality
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- 2Hallym Data Science Laboratory, Hallym University College of Medicine, Anyang, Korea
- 3Graduate School of Public Health, Seoul National University, Seoul, Korea
- 4Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University Medical Center, Hallym University College of Medicine, Seoul, Korea
- 5Department of Otorhinolaryngology-Head and Neck Surgery, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea
- KMID: 2519182
- DOI: http://doi.org/10.21053/ceo.2021.00325
Abstract
Objectives
. We evaluated changes in income levels in a hearing-impaired population.
Methods
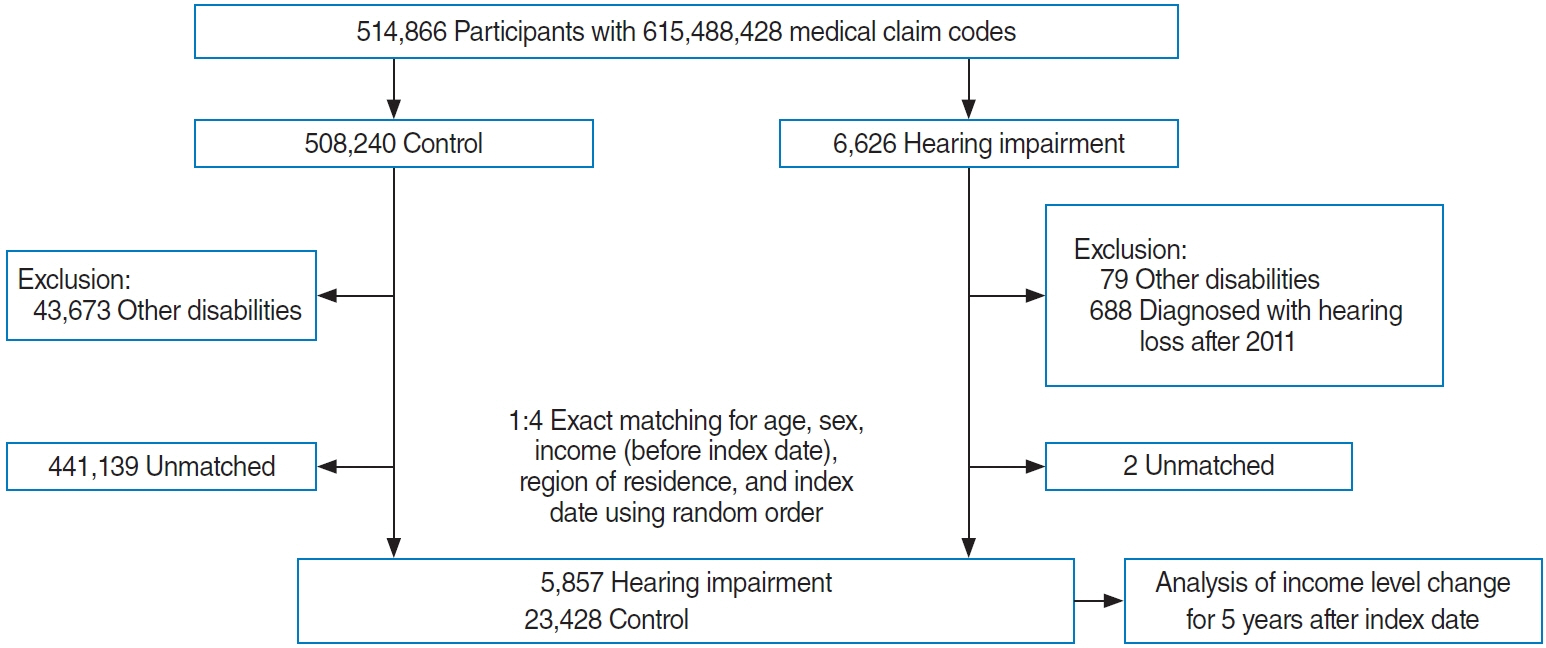
. The study subjects were selected from the Korean National Health Insurance Service-Health Screening Cohort data from 2002 to 2015 of Koreans ≥40 years old. In total, 5,857 hearing-impaired subjects were matched with 23,428 comparison participants. Differences between the initial income level and income levels at 1, 2, 3, 4, and 5 years post-enrollment were compared between the hearing-impaired and comparison groups. The interaction of time and hearing impairment/comparison was estimated.
Results
. Both the hearing-impaired group and the comparison group showed increased income levels over time. In the hearing-impaired group, the income levels at 4 and 5 years post-enrollment were higher than the initial income level (each P<0.001). In the comparison group, the income levels of all the participants after 1–5 years were higher than the initial income level (each P<0.001). The interaction of time and hearing impairment was statistically significant (P=0.021).
Conclusion
. The increase in income over time was relatively lower in the hearing-impaired adult population; therefore, the income gap widened between this population and the normal-hearing population.
Keyword
Figure
Cited by 1 articles
-
Part 1. Current Status of Hearing Loss Patients in Korea Using National Data: National Health Insurance Service-Database, 2010 to 2020
Junhun Lee, Chul Young Yoon, Jiwon Kim, In-Ki Jin, Michelle J. Suh, Wan-Ho Cho, Hyo-Jeong Lee, Seong Jun Choi, Dongchul Cha, Kyung Ho Park, Soo Hee Oh, Young Joon Seo, Tae Hoon Kong
Korean J Otorhinolaryngol-Head Neck Surg. 2025;68(1):7-18. doi: 10.3342/kjorl-hns.2024.00157.
Reference
-
1. Kontis V, Cobb LK, Mathers CD, Frieden TR, Ezzati M, Danaei G. Three public health interventions could save 94 million lives in 25 years. Circulation. 2019; Aug. 140(9):715–25.
Article2. GBD 2015 disease and injury incidence and prevalence collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016; Oct. 388(10053):1545–602.3. Goman AM, Lin FR. Prevalence of hearing loss by severity in the united states. Am J Public Health. 2016; Oct. 106(10):1820–2.
Article4. Sharma RK, Lalwani AK, Golub JS. Prevalence and severity of hearing loss in the older old population. JAMA Otolaryngol Head Neck Surg. 2020; Aug. 146(8):762–3.
Article5. Exeter DJ, Wu B, Lee AC, Searchfield GD. The projected burden of hearing loss in New Zealand (2011-2061) and the implications for the hearing health workforce. N Z Med J. 2015; Aug. 128(1419):12–21.6. GBD 2016 disease and injury incidence and prevalence collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017; Sep. 390(10100):1211–59.7. Shukla A, Harper M, Pedersen E, Goman A, Suen JJ, Price C, et al. Hearing loss, loneliness, and social isolation: a systematic review. Otolaryngol Head Neck Surg. 2020; May. 162(5):622–33.
Article8. Ramsey T, Svider PF, Folbe AJ. Health burden and socioeconomic disparities from hearing loss: a global perspective. Otol Neurotol. 2018; Jan. 39(1):12–6.
Article9. Emmett SD, Francis HW. The socioeconomic impact of hearing loss in U.S. adults. Otol Neurotol. 2015; Mar. 36(3):545–50.
Article10. Lee JS, Choi HG, Jang JH, Sim S, Hong SK, Lee HJ, et al. Analysis of predisposing factors for hearing loss in adults. J Korean Med Sci. 2015; Aug. 30(8):1175–82.
Article11. Jones DD. Relative earnings of deaf and hard-of-hearing individuals. J Deaf Stud Deaf Educ. 2004; Fall. 9(4):459–61.
Article12. Kim SY, Min C, Oh DJ, Choi HG. Tobacco smoking and alcohol consumption are related to benign parotid tumor: a nested case-control study using a national health screening cohort. Clin Exp Otorhinolaryngol. 2019; Nov. 12(4):412–9.
Article13. Kim SY, Lim JS, Kong IG, Choi HG. Hearing impairment and the risk of neurodegenerative dementia: a longitudinal follow-up study using a national sample cohort. Sci Rep. 2018; Oct. 8(1):15266.
Article14. Kim SY, Min C, Kim HJ, Lee CH, Sim S, Park B, et al. Mortality and cause of death in hearing loss participants: a longitudinal follow-up study using a national sample cohort. Otol Neurotol. 2020; Jan. 41(1):25–32.
Article15. National Health Insurance Service. National medical examination sample cohort (NHIS-NMES) user manual [Internet]. Wonju: National Health Insurance Service;2017 [cited 2021 Apr 1]. Available from: https://nhiss.nhis.or.kr/bd/ab/bdaba006cv.do.16. Kim SY, Oh DJ, Park B, Choi HG. Bell’s palsy and obesity, alcohol consumption and smoking: a nested case-control study using a national health screening cohort. Sci Rep. 2020; Mar. 10(1):4248.
Article17. Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011; Mar. 173(6):676–82.
Article18. Jung D, Bhattacharyya N. Association of hearing loss with decreased employment and income among adults in the United States. Ann Otol Rhinol Laryngol. 2012; Dec. 121(12):771–5.
Article19. He P, Luo Y, Hu X, Gong R, Wen X, Zheng X. Association of socioeconomic status with hearing loss in Chinese working-aged adults: a population-based study. PLoS One. 2018; Mar. 13(3):e0195227.
Article20. Shan A, Ting JS, Price C, Goman AM, Willink A, Reed NS, et al. Hearing loss and employment: a systematic review of the association between hearing loss and employment among adults. J Laryngol Otol. 2020; May. 134(5):387–97.
Article21. Wagner-Hartl V, Grossi NR, Kallus KW. Impact of age and hearing impairment on work performance during long working hours. Int J Environ Res Public Health. 2018; Jan. 15(1):98.
Article22. Jennings MB, Shaw L. Impact of hearing loss in the workplace: raising questions about partnerships with professionals. Work. 2008; 30(3):289–95.23. Nachtegaal J, Kuik DJ, Anema JR, Goverts ST, Festen JM, Kramer SE. Hearing status, need for recovery after work, and psychosocial work characteristics: results from an internet-based national survey on hearing. Int J Audiol. 2009; 48(10):684–91.
Article24. Kramer SE, Kapteyn TS, Houtgast T. Occupational performance: comparing normally-hearing and hearing-impaired employees using the Amsterdam Checklist for Hearing and Work. Int J Audiol. 2006; Sep. 45(9):503–12.
Article25. Jennings MB, Shaw L, Hodgins H, Kuchar DA, Bataghva LP. Evaluating auditory perception and communication demands required to carry out work tasks and complimentary hearing resources and skills for older workers with hearing loss. Work. 2010; 35(1):101–13.
Article26. Genther DJ, Frick KD, Chen D, Betz J, Lin FR. Association of hearing loss with hospitalization and burden of disease in older adults. JAMA. 2013; Jun. 309(22):2322–4.
Article27. Besser J, Stropahl M, Urry E, Launer S. Comorbidities of hearing loss and the implications of multimorbidity for audiological care. Hear Res. 2018; Nov. 369:3–14.
Article28. Thomas JP, Loke YK, Alexandre L. Efficacy and safety profile of statins in patients with cancer: a systematic review of randomised controlled trials. Eur J Clin Pharmacol. 2020; Dec. 76(12):1639–51.
Article29. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the national health insurance service-national sample cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; Apr. 46(2):e15.
Article30. Lee HJ, Lee JM, Na G, Moon YM, Lee C, Jung J. Which patients with a unilateral hearing aid for symmetric sensorineural hearing loss have auditory deprivation. Clin Exp Otorhinolaryngol. 2020; Feb. 13(1):23–8.
Article31. Moon IJ, Baek SY, Cho YS. Hearing aid use and associated factors in South Korea. Medicine (Baltimore). 2015; Oct. 94(42):e1580.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictors of Depression in Disability with Hearing Impairment
- Influence of the coexistence of visual impairment, hearing impairment, and masticatory discomfort on the quality of life of middle-aged adults: an analysis based on the 2019 and 2020 Korea National Health and Nutrition Examination Survey
- New Guides to the Evaluation of Korean Hearing Impairment in 2012
- The Effect of Visual and Hearing Impairment on Depression and Cognitive Function in Community-dwelling Elderly: The Korean Longitudinal Study of Aging 2008
- Association between Hearing Difficulty, Masticatory Difficulty, and Risk of Cognitive Impairment: Analysis of the Korean Longitudinal Study of Aging Data (2006-2020)