Anesth Pain Med.
2021 Jul;16(3):305-311. 10.17085/apm.21011.
The correlation between the STOP-Bang score and oxygen saturation during spinal anesthesia with dexmedetomidine sedation
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- 2Department of Anesthesiology and Pain Medicine, Busan Central Hospital, Busan, Korea
- KMID: 2519062
- DOI: http://doi.org/10.17085/apm.21011
Abstract
- Background
The STOP-BANG questionnaire is a simple screening tool with high sensitivity for the detection of severe obstructive sleep apnea (OSA). Predicting airway obstruction would allow the safe management of sedative patients to prevent intraoperative hypoxia. This study was designed to check the correlation between the STOP-BANG score and oxygen saturation (SpO2) during sedation and confirm the availability of the STOP-BANG questionnaire as a preoperative exam for predicting the incidence of hypoxia in sedative patient management.
Methods
This study included 56 patients who received spinal anesthesia. The pre-anesthesia evaluation was conducted using the STOP-Bang questionnaire. The patients were under spinal anesthesia with an average block level of T10. Dexmedetomidine was infused with a loading dose of 1 μg/kg over 10 min and a maintenance dose of 0.5 μg/kg/h until the end of the procedure. The SpO2 of the patients was recorded every 5 min.
Results
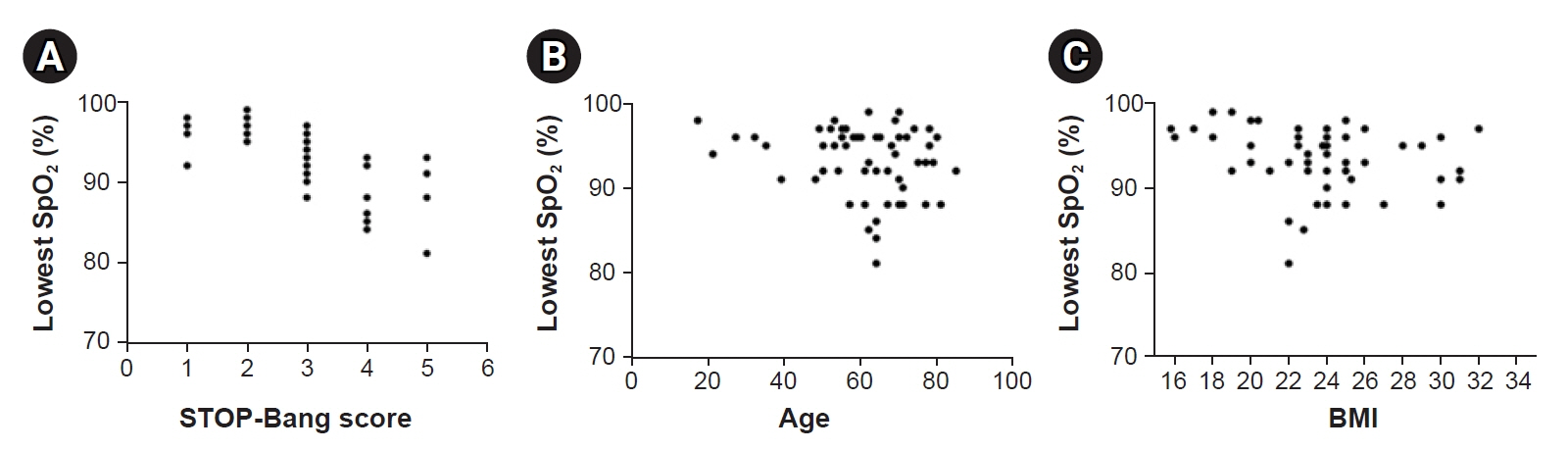
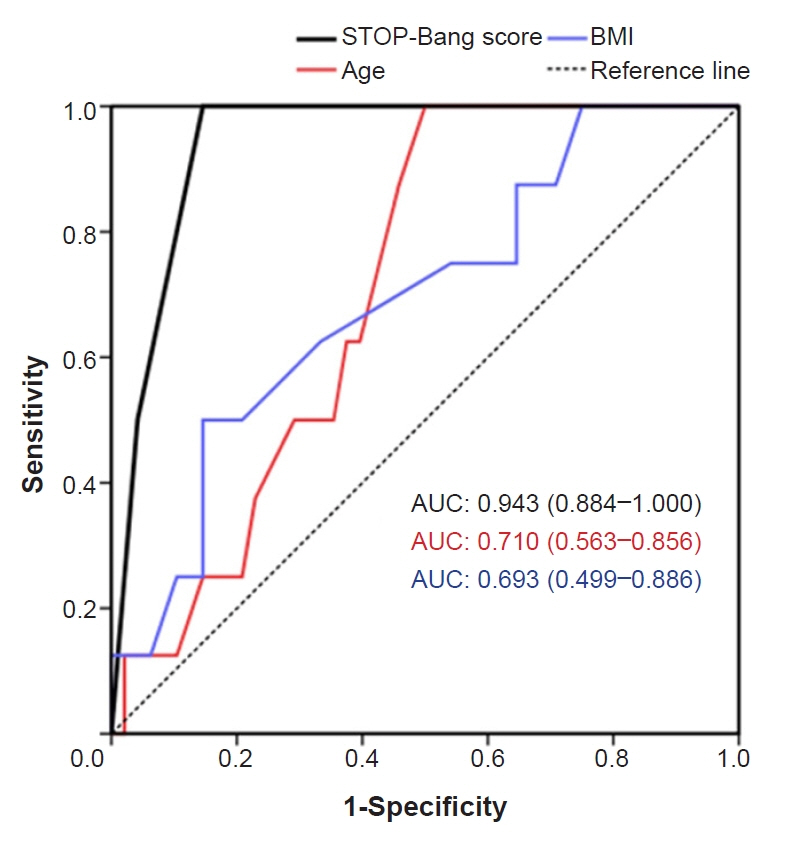
The STOP-Bang score was negatively correlated with the lowest SpO2 (coefficient = –0.774, 95% confidence interval [CI]: –0.855 to –0.649, standard error [SE] = 0.054, P < 0.001). The item of “observed apnea” was the most correlated one with hypoxic events (odds ratio = 6.00, 95% CI: 1.086 to 33.145).
Conclusions
The STOP-BANG score was significantly correlated with the lowest SpO2 during spinal anesthesia, which enabled the prediction of meaningful hypoxia before it occurred in the sedated patients.
Figure
Reference
-
1. Borgeat A, Aguirre J. Sedation and regional anesthesia. Curr Opin Anaesthesiol. 2009; 22:678–82.2. Elkalla RS, El Mourad MB. Respiratory and hemodynamic effects of three different sedative regimens for drug induced sleep endoscopy in sleep apnea patients. A prospective randomized study. Minerva Anestesiol. 2020; 86:132–40.3. Chang ET, Certal V, Song SA, Zaghi S, Carrasco-Llatas M, Torre C, et al. Dexmedetomidine versus propofol during drug-induced sleep endoscopy and sedation: a systematic review. Sleep Breath. 2017; 21:727–35.4. Xu JK, Ye JY, Cao X, Zhang YH, Yuan XM, Zhao CM. [Polysomnographic comparation between dexmedetomidine-induced sleep and natural sleep]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2019; 54:405–9. Chinese.5. Amornyotin S. Sedation-related complications in gastrointestinal endoscopy. World J Gastrointest Endosc. 2013; 5:527–33.6. Geng W, Jia D, Wang Y, Jin S, Ren Y, Liang D, et al. A prediction model for hypoxemia during routine sedation for gastrointestinal endoscopy. Clinics (Sao Paulo). 2018; 73:e513.7. Coté GA, Hovis CE, Hovis RM, Waldbaum L, Early DS, Edmundowicz SA, et al. A screening instrument for sleep apnea predicts airway maneuvers in patients undergoing advanced endoscopic procedures. Clin Gastroenterol Hepatol. 2010; 8:660–5. e1.8. Mathangi K, Mathews J, Mathangi CD. Assessment of perioperative difficult airway among undiagnosed obstructive sleep apnoea patients undergoing elective surgery: a prospective cohort study. Indian J Anaesth. 2018; 62:538–44.9. Larner A, B Z. Screening for obstructive sleep apnoea using the STOPBANG questionnaire. Clin Med (Lond). 2018; 18:108–9.10. Pearson F, Batterham AM, Cope S. The STOP-Bang Questionnaire as a screening tool for obstructive sleep apnea in pregnancy. J Clin Sleep Med. 2019; 15:705–10.11. Nagappa M, Liao P, Wong J, Auckley D, Ramachandran SK, Memtsoudis S, et al. Validation of the STOP-Bang Questionnaire as a screening tool for obstructive sleep apnea among different populations: a systematic review and meta-analysis. PLoS One. 2015; 10:e0143697.12. Kim KT, Cho YW. Real-world STOPBANG: how useful is STOPBANG for sleep clinics? Sleep Breath. 2019; 23:1219–26.13. Chung F, Abdullah HR, Liao P. STOP-Bang Questionnaire: a practical approach to screen for obstructive sleep apnea. Chest. 2016; 149:631–8.14. Oshita H, Ito N, Senoo M, Funaishi K, Mitama Y, Okusaki K. The STOP-Bang test is useful for predicting the severity of obstructive sleep apnea. JMA J. 2020; 3:347–52.15. Kang D, Lim C, Shim DJ, Kim H, Kim JW, Chung HJ, et al. The correlation of heart rate between natural sleep and dexmedetomidine sedation. Korean J Anesthesiol. 2019; 72:164–8.16. Shin HJ, Kim EY, Hwang JW, Do SH, Na HS. Comparison of upper airway patency in patients with mild obstructive sleep apnea during dexmedetomidine or propofol sedation: a prospective, randomized, controlled trial. BMC Anesthesiol. 2018; 18:120.17. Chiu HY, Chen PY, Chuang LP, Chen NH, Tu YK, Hsieh YJ, et al. Diagnostic accuracy of the Berlin questionnaire, STOP-BANG, STOP, and Epworth sleepiness scale in detecting obstructive sleep apnea: a bivariate meta-analysis. Sleep Med Rev. 2017; 36:57–70.18. Neves Junior JAS, Fernandes APA, Tardelli MA, Yamashita AM, Moura SMPGT, Tufik S, et al. Cutoff points in STOP-Bang questionnaire for obstructive sleep apnea. Arq Neuropsiquiatr. 2020; 78:561–9.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effective dose of dexmedetomidine to induce adequate sedation in elderly patients under spinal anesthesia
- Fatal pulmonary aspiration during balanced sedation with dexmedetomidine and midazolam: A case report
- The Effect of Sedation with Diazepam on Arterial Oxygen Saturation During Spinal Anesthesia
- A loading dose of 1 µg/kg and maintenance dose of 0.5 µg/kg/h of dexmedetomidine for sedation under spinal anesthesia may induce excessive sedation and airway obstruction
- Verification of the performance of the Bispectral Index as a hypnotic depth indicator during dexmedetomidine sedation