Anesth Pain Med.
2021 Jul;16(3):266-272. 10.17085/apm.21025.
Pre-operative fasting times for clear liquids at a tertiary children’s hospital; what can be improved?
- Affiliations
-
- 1Department of Anesthesiology, Perioperative and Pain Medicine, Stanford University School of Medicine, Stanford, CA, USA
- KMID: 2519055
- DOI: http://doi.org/10.17085/apm.21025
Abstract
- Background
The goal of preoperative fasting is to prevent pulmonary aspiration during general anesthesia. Fasting times are often prolonged leading to patient discomfort and risk for adverse events. This retrospective quality improvement survey evaluated effective nil-per-os (NPO) times and causes for prolonged NPO times with the aim to suggest improvement strategies by a newly founded fasting task force.
Methods
Data from all electronic anesthesia records from 2019 at our institution were reviewed for fasting times. Our NPO instructions follow American Society of Anesthesiology guidelines and are calculated based on the patient’s arrival time (90 min before OR time). Primary outcome was the effective NPO time for clear liquids, secondary outcomes were incidence of delays and the parental compliance with the NPO instructions. Data are presented as median (interquartile range).
Results
9,625 cases were included in the analysis. NPO time was documented in 72.1% with a median effective NPO time of 7:13 h (7:36). OR in room times were documented in 72.8%, 2,075 (29.5%; median time 0:10 h [0:21]) were earlier and 4,939 (70.5%; median time 0:29 h [0:54]) were later than scheduled. Parental NPO compliance showed a median deviation for clear liquid intake of 0:55 h (8:30).
Conclusions
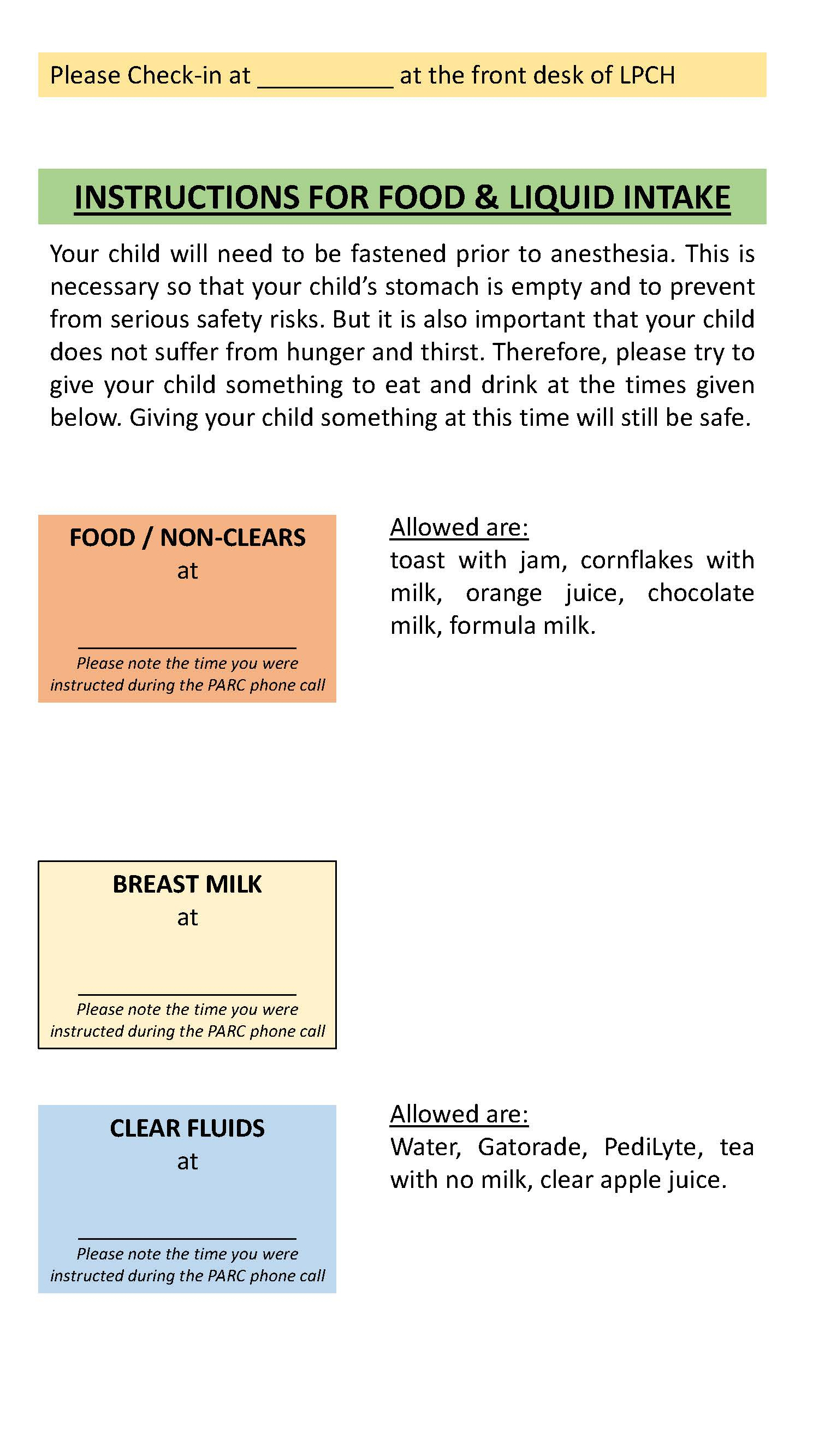
This study revealed that effective NPO times were longer than current ASA guidelines. Contributing causes include case delays and parental non-compliance to NPO instructions. Thus, task force recommendations include change NPO instruction calculations to scheduled OR time versus arrival time, and encourage parents to give their child clear liquids at the instructed time.
Figure
Reference
-
1. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Task Force on preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration. Anesthesiology. 2017; 126:376–93.2. Engelhardt T, Wilson G, Horne L, Weiss M, Schmitz A. Are you hungry? Are you thirsty?--fasting times in elective outpatient pediatric patients. Paediatr Anaesth. 2011; 21:964–8.3. Schmitz A, Kellenberger CJ, Neuhaus D, Schroeter E, Deanovic D, Prüfer F, et al. Fasting times and gastric contents volume in children undergoing deep propofol sedation--an assessment using magnetic resonance imaging. Paediatr Anaesth. 2011; 21:685–90.4. Arun BG, Korula G. Preoperative fasting in children: an audit and its implications in a tertiary care hospital. J Anaesthesiol Clin Pharmacol. 2013; 29:88–91.5. Beck CE, Rudolp D, Becke-Jakob K, Schindler E, Etspüler A, Trapp A, et al. Real fasting times and incidence of pulmonary aspiration in children: results of a German prospective multicenter observational study. Paediatr Anaesth. 2019; 29:1040–5.6. Dennhardt N, Beck C, Huber D, Nickel K, Sander B, Witt LH, et al. Impact of preoperative fasting times on blood glucose concentration, ketone bodies and acid-base balance in children younger than 36 months: a prospective observational study. Eur J Anaesthesiol. 2015; 32:857–61.7. Dennhardt N, Beck C, Huber D, Sander B, Boehne M, Boethig D, et al. Optimized preoperative fasting times decrease ketone body concentration and stabilize mean arterial blood pressure during induction of anesthesia in children younger than 36 months: a prospective observational cohort study. Paediatr Anaesth. 2016; 26:838–43.8. Isserman R, Elliott E, Subramanyam R, Kraus B, Sutherland T, Madu C, et al. Quality improvement project to reduce pediatric clear liquid fasting times prior to anesthesia. Paediatr Anaesth. 2019; 29:698–704.9. Newton RJG, Stuart GM, Willdridge DJ, Thomas M. Using quality improvement methods to reduce clear fluid fasting times in children on a preoperative ward. Paediatr Anaesth. 2017; 27:793–800.10. Schmitz A, Kellenberger CJ, Liamlahi R, Studhalter M, Weiss M. Gastric emptying after overnight fasting and clear fluid intake: a prospective investigation using serial magnetic resonance imaging in healthy children. Br J Anaesth. 2011; 107:425–9.11. Schmitz A, Kellenberger CJ, Lochbuehler N, Fruehauf M, Klaghofer R, Fruehauf H, et al. Effect of different quantities of a sugared clear fluid on gastric emptying and residual volume in children: a crossover study using magnetic resonance imaging. Br J Anaesth. 2012; 108:644–7.12. Andersson H, Zarén B, Frykholm P. Low incidence of pulmonary aspiration in children allowed intake of clear fluids until called to the operating suite. Paediatr Anaesth. 2015; 25:770–7.13. Schmidt AR, Buehler P, Seglias L, Stark T, Brotschi B, Renner T, et al. Gastric pH and residual volume after 1 and 2 h fasting time for clear fluids in children†. Br J Anaesth. 2015; 114:477–82.14. Schmidt AR, Buehler KP, Both C, Wiener R, Klaghofer R, Hersberger M, et al. Liberal fluid fasting: impact on gastric pH and residual volume in healthy children undergoing general anaesthesia for elective surgery. Br J Anaesth. 2018; 121:647–55.15. Thomas M, Morrison C, Newton R, Schindler E. Consensus statement on clear fluids fasting for elective pediatric general anesthesia. Paediatr Anaesth. 2018; 28:411–4.16. Rosen D, Gamble J, Matava C; Canadian Pediatric Anesthesia Society Fasting Guidelines Working Group. Canadian Pediatric Anesthesia Society statement on clear fluid fasting for elective pediatric anesthesia. Can J Anaesth. 2019; 66:991–2.17. Linscott D. SPANZA endorses 1-hour clear fluid fasting consensus statement. Paediatr Anaesth. 2019; 29:292.18. Disma N, Thomas M, Afshari A, Veyckemans F, De Hert S. Clear fluids fasting for elective paediatric anaesthesia: the European Society of Anaesthesiology consensus statement. Eur J Anaesthesiol. 2019; 36:173–4.19. Nye A, Conner E, Wang E, Chadwick W, Marquez J, Caruso TJ. A pilot quality improvement project to reduce preoperative fasting duration in pediatric inpatients. Pediatr Qual Saf. 2019; 4:e246.20. Schreiner MS, Triebwasser A, Keon TP. Ingestion of liquids compared with preoperative fasting in pediatric outpatients. Anesthesiology. 1990; 72:593–7.21. Brady M, Kinn S, Ness V, O'Rourke K, Randhawa N, Stuart P. Preoperative fasting for preventing perioperative complications in children. Cochrane Database Syst Rev. 2009; 4:CD005285.22. Best C, Wolstenholme S, Kimble J, Hitchings H, Gordon HM. How 'nil by mouth' instructions impact on patient behaviour. Nurs Times. 2004; 100:32–4.23. Splinter WM, Stewart JA, Muir JG. The effect of preoperative apple juice on gastric contents, thirst, and hunger in children. Can J Anaesth. 1989; 36:55–8.24. Splinter WM, Stewart JA, Muir JG. Large volumes of apple juice preoperatively do not affect gastric pH and volume in children. Can J Anaesth. 1990; 37:36–9.25. Castillo-Zamora C, Castillo-Peralta LA, Nava-Ocampo AA. Randomized trial comparing overnight preoperative fasting period vs oral administration of apple juice at 06:00-06:30 am in pediatric orthopedic surgical patients. Paediatr Anaesth. 2005; 15:638–42.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Influence of Pre-operative Fasting Time on Blood Glucose in Older Patients
- The Efficacy of 4 Liters of Clear Liquids for Small Bowel Preparation Prior to Video Capsule Endoscopy
- Effects of Preoperative Oral Water Intake on Gastric Content and Emotional State of Patients
- The Irritancy of Hand Dishwashing Liquids on the Skin
- Standard Recipes for the Preparation of Thickened Barium Liquids Used in the Diagnosis of Dysphagia