Ann Surg Treat Res.
2021 Aug;101(2):93-101. 10.4174/astr.2021.101.2.93.
Oncologic comparison between nonradical management and total mesorectal excision in good responders after chemoradiotherapy in patients with mid-to-low rectal cancer
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 2Center for Colorectal Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea
- 3Department of Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2519002
- DOI: http://doi.org/10.4174/astr.2021.101.2.93
Abstract
- Purpose
This study was performed to compare the oncologic outcomes between nonradical management and total mesorectal excision in good responders after chemoradiotherapy.
Methods
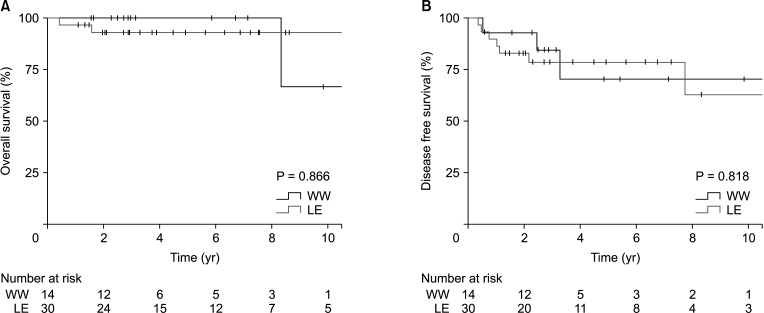
We analyzed 75 patients, who underwent 14 watch-and-wait, 30 local excision, and 31 total mesorectal excision, in ycT0–1N0M0 based on magnetic resonance imaging after chemoradiotherapy for advanced mid-to-low rectal cancer in 3 referral hospitals. The nonradical management group underwent surveillance with additional sigmoidoscopy and rectal magnetic resonance imaging every 3–6 months within the first 2 years.
Results
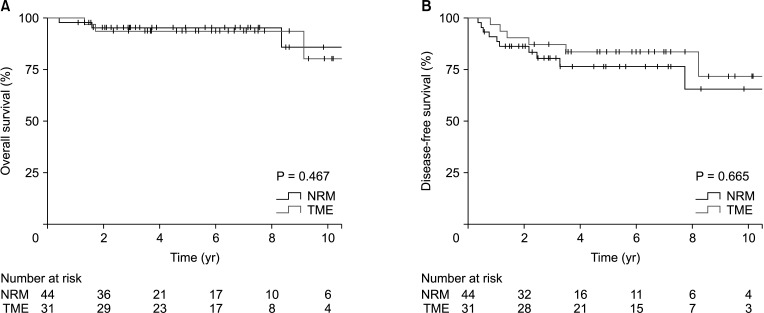
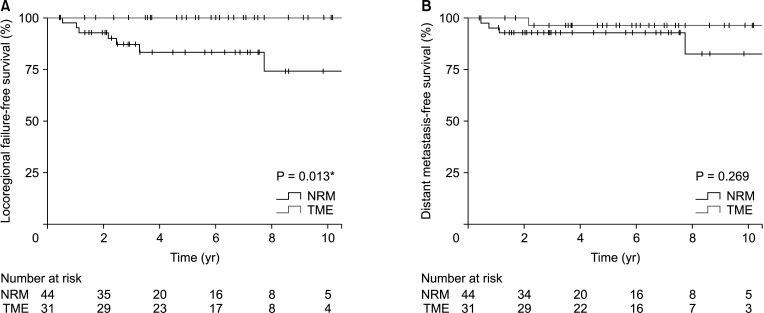
Nonradical management group had more low-lying tumors (P < 0.001) and less lymph node metastasis based on magnetic resonance imaging (P = 0.004). However, cT stage, ycT, and ycN stage were not different between the 2 groups. With a median follow-up period of 64.7 months, the 5-year locoregional failure rate was higher in the nonradical management group than in the total mesorectal excision group (16.7% vs. 0%, P = 0.013). However, the 5-year overall survival and disease-free survival rates of the nonradical management and total mesorectal excision groups were not different (95.2% vs. 93.5%, P = 0.467; 76.4% vs. 83.6%, P = 0.665; respectively).
Conclusion
This study shows that nonradical management for ycT0–1N0 mid-to-low rectal cancer may be an alternative treatment to total mesorectal excision under proper surveillance and management for oncologic events.
Figure
Reference
-
1. Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C, et al. Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol. 2012; 30:1926–1933. PMID: 22529255.
Article2. Uehara K, Nagino M. Neoadjuvant treatment for locally advanced rectal cancer: a systematic review. Surg Today. 2016; 46:161–168. PMID: 26170102.
Article3. Roh MS, Colangelo LH, O'Connell MJ, Yothers G, Deutsch M, Allegra CJ, et al. Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum: NSABP R-03. J Clin Oncol. 2009; 27:5124–5130. PMID: 19770376.
Article4. Yoon WH, Kim HJ, Kim CH, Joo JK, Kim YJ, Kim HR. Oncologic impact of pathologic response on clinical outcome after preoperative chemoradiotherapy in locally advanced rectal cancer. Ann Surg Treat Res. 2015; 88:15–20. PMID: 25553320.
Article5. Pucciarelli S, Giandomenico F, De Paoli A, Gavaruzzi T, Lotto L, Mantello G, et al. Bowel function and quality of life after local excision or total mesorectal excision following chemoradiotherapy for rectal cancer. Br J Surg. 2017; 104:138–147. PMID: 27706805.
Article6. Hallam S, Messenger DE, Thomas MG. A systematic review of local excision after neoadjuvant therapy for rectal cancer: are ypt0 tumors the limit? Dis Colon Rectum. 2016; 59:984–997. PMID: 27602930.
Article7. Dattani M, Heald RJ, Goussous G, Broadhurst J, São Julião GP, Habr-Gama A, et al. Oncological and survival outcomes in watch and wait patients with a clinical complete response after neoadjuvant chemoradiotherapy for rectal cancer: a systematic review and pooled analysis. Ann Surg. 2018; 268:955–967. PMID: 29746338.8. Renehan AG, Malcomson L, Emsley R, Gollins S, Maw A, Myint AS, et al. Watch-and-wait approach versus surgical resection after chemoradiotherapy for patients with rectal cancer (the OnCoRe project): a propensity-score matched cohort analysis. Lancet Oncol. 2016; 17:174–183. PMID: 26705854.
Article9. Maas M, Nelemans PJ, Valentini V, Das P, Rödel C, Kuo LJ, et al. Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data. Lancet Oncol. 2010; 11:835–844. PMID: 20692872.
Article10. Rullier E, Vendrely V, Asselineau J, Rouanet P, Tuech JJ, Valverde A, et al. Organ preservation with chemoradiotherapy plus local excision for rectal cancer: 5-year results of the GRECCAR 2 randomised trial. Lancet Gastroenterol Hepatol. 2020; 5:465–474. PMID: 32043980.
Article11. Shaikh I, Askari A, Ourû S, Warusavitarne J, Athanasiou T, Faiz O. Oncological outcomes of local excision compared with radical surgery after neoadjuvant chemoradiotherapy for rectal cancer: a systematic review and meta-analysis. Int J Colorectal Dis. 2015; 30:19–29. PMID: 25367179.
Article12. Garcia-Aguilar J, Renfro LA, Chow OS, Shi Q, Carrero XW, Lynn PB, et al. Organ preservation for clinical T2N0 distal rectal cancer using neoadjuvant chemoradiotherapy and local excision (ACOSOG Z6041): results of an open-label, single-arm, multi-institutional, phase 2 trial. Lancet Oncol. 2015; 16:1537–1546. PMID: 26474521.
Article13. Kim DW, Kim DY, Kim TH, Jung KH, Chang HJ, Sohn DK, et al. Is T classification still correlated with lymph node status after preoperative chemoradiotherapy for rectal cancer. Cancer. 2006; 106:1694–1700. PMID: 16532432.
Article14. Huang SH, Chi P, Lin HM, Lu XR, Huang YW, Xu ZB, et al. Selecting stage ypT0-1N0 for locally advanced rectal cancer following preoperative chemoradiotherapy: implications for potential candidates of organ-sparing management. Colorectal Dis. 2016; 18:989–996. PMID: 26880193.
Article15. Shin YS, Park JH, Yoon SM, Kim JC, Yu CS, Lim SB, et al. Total mesorectal excision versus local excision after preoperative chemoradiotherapy in rectal cancer with lymph node metastasis: a propensity score-matched analysis. Int J Radiat Oncol Biol Phys. 2018; 101:630–639. PMID: 29678529.16. Balyasnikova S, Brown G. Optimal imaging strategies for rectal cancer staging and ongoing management. Curr Treat Options Oncol. 2016; 17:32. PMID: 27255100.
Article17. Jeong SY, Park JW, Nam BH, Kim S, Kang SB, Lim SB, et al. Open versus laparoscopic surgery for mid-rectal or low- rectal cancer after neoadjuvant chemoradiotherapy (COREAN trial): survival outcomes of an open-label, non-inferiority, randomised controlled trial. Lancet Oncol. 2014; 15:767–774. PMID: 24837215.18. Patel UB, Taylor F, Blomqvist L, George C, Evans H, Tekkis P, et al. Magnetic resonance imaging-detected tumor response for locally advanced rectal cancer predicts survival outcomes: MERCURY experience. J Clin Oncol. 2011; 29:3753–3760. PMID: 21876084.
Article19. Kang SB, Cho JR, Jeong SY, Oh JH, Ahn S, Choi S, et al. Quality of life after sphincter preservation surgery or abdominoperineal resection for low rectal cancer (ASPIRE): a long-term prospective, multicentre, cohort study. Lancet Reg Health West Pac. 2021; 6:100087. PMID: 34327411.
Article20. National Cancer Institute (NCI). Common Terminology Criteria for Adverse Events (CTCAE). v5.0. Bethesda (MD): NCI;2017.21. Song KS, Park SC, Sohn DK, Oh JH, Kim MJ, Park JW, et al. Oncologic risk of rectal preservation against medical advice after chemoradiotherapy for rectal cancer: a multicenter comparative cross-sectional study with rectal preservation as supported by surgeon. World J Surg. 2019; 43:3216–3223. PMID: 31410512.
Article22. Punt CJ, Buyse M, Köhne CH, Hohenberger P, Labianca R, Schmoll HJ, et al. Endpoints in adjuvant treatment trials: a systematic review of the literature in colon cancer and proposed definitions for future trials. J Natl Cancer Inst. 2007; 99:998–1003. PMID: 17596575.
Article23. Smith JD, Ruby JA, Goodman KA, Saltz LB, Guillem JG, Weiser MR, et al. Nonoperative management of rectal cancer with complete clinical response after neoadjuvant therapy. Ann Surg. 2012; 256:965–972. PMID: 23154394.
Article24. Appelt AL, Pløen J, Harling H, Jensen FS, Jensen LH, Jørgensen JC, et al. High-dose chemoradiotherapy and watchful waiting for distal rectal cancer: a prospective observational study. Lancet Oncol. 2015; 16:919–927. PMID: 26156652.
Article25. Lai CL, Lai MJ, Wu CC, Jao SW, Hsiao CW. Rectal cancer with complete clinical response after neoadjuvant chemoradiotherapy, surgery, or “watch and wait”. Int J Colorectal Dis. 2016; 31:413–419. PMID: 26607907.
Article26. Fiorica F, Trovò M, Anania G, Marcello D, Di Benedetto F, Marzola M, et al. Is it possible a conservative approach after radiochemotherapy in locally advanced rectal cancer (LARC)? A systematic review of the literature and meta-analysis. J Gastrointest Cancer. 2019; 50:98–108. PMID: 29273921.
Article27. Liu S, Zhong GX, Zhou WX, Xue HD, Pan WD, Xu L, et al. Can endorectal ultrasound, MRI, and mucosa integrity accurately predic t the complete response for mid-low rectal cancer after preoperative chemoradiation? A prospective observational study from a single medical center. Dis Colon Rectum. 2018; 61:903–910. PMID: 29944579.28. Patel UB, Brown G, Rutten H, West N, Sebag-Montefiore D, Glynne-Jones R, et al. Comparison of magnetic resonance imaging and histopathological response to chemoradiotherapy i n local ly advanced rectal cancer. Ann Surg Oncol. 2012; 19:2842–2852. PMID: 22526897.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical issues in locally advanced rectal cancer treated by preoperative chemoradiotherapy
- Impact of circumferential tumor location of mid to low rectal cancer on oncologic outcomes after preoperative chemoradiotherapy
- Recent Advances in the Diagnosis and Treatment for Rectal Cancer
- Transanal Endoscopic and Transabdominal Robotic Total Mesorectal Excision for Mid-to-Low Rectal Cancer: Comparison of Short-term Postoperative and Oncologic Outcomes by Using a Case-Matched Analysis
- Does a Successful Total Mesorectal ExcisionRequire a Learning Curve?