Clin Endosc.
2021 Jul;54(4):563-569. 10.5946/ce.2020.109.
The Use of Endoscopic Clipping in Preventing Delayed Complications after Endoscopic Resection for Superficial Non-Ampullary Duodenal Tumors
- Affiliations
-
- 1Department of Internal Medicine, Incheon St. Mary’s Hospital, The Catholic University of Korea, Incheon, Korea
- 2Department of Internal Medicine, Seoul St. Mary’s Hospital, The Catholic University of Korea, Seoul, Korea
- 3Department of Internal Medicine, Bucheon St. Mary’s Hospital, The Catholic University of Korea, Bucheon, Korea
- KMID: 2518860
- DOI: http://doi.org/10.5946/ce.2020.109
Abstract
- Background/Aims
Endoscopic resection (ER) has recently been accepted as the standard treatment modality for superficial nonampullary duodenal tumors (SNADTs). However, the procedure can cause adverse events such as perforation and bleeding. This study aimed to investigate the efficacy of prophylactic clipping in the prevention of delayed complications.
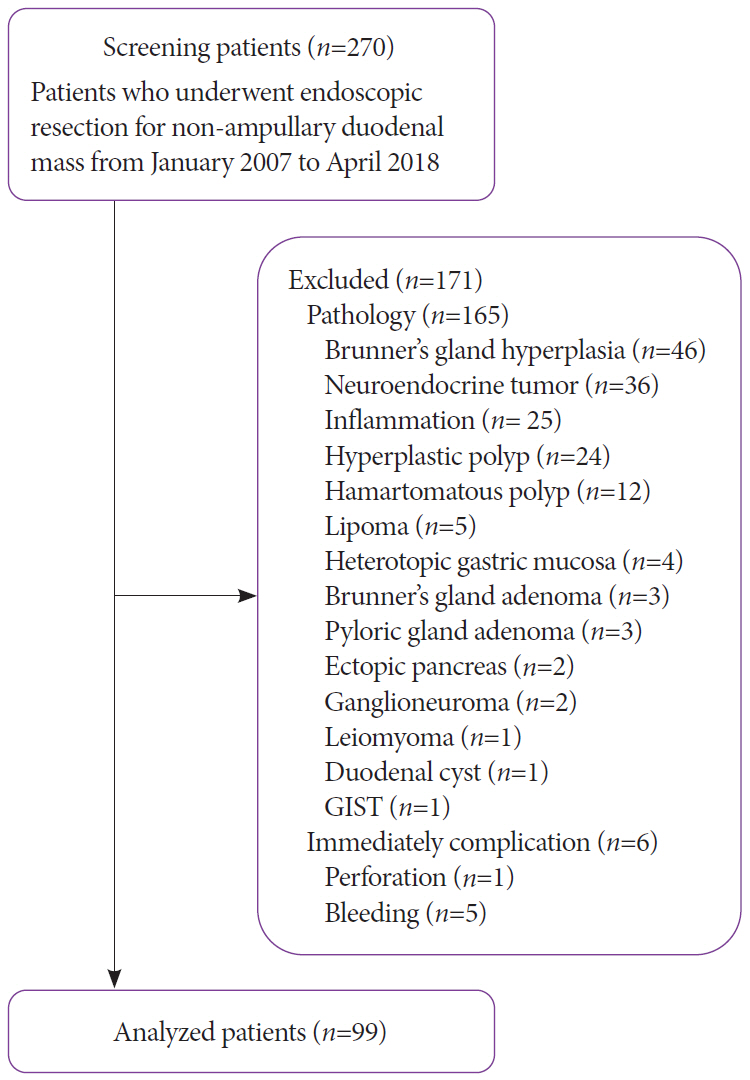
Methods
A retrospective review of the medical records of patients who underwent ER for SNADT from 3 centers was performed. Patients were divided into 2 groups: the immediate clipping group (ICG) and the no clipping group (NCG). Various baseline characteristics and factors associated with the appearance of delayed complications, such as size of the lesion, tumor location, histologic type, and co-morbidities, were compared between the two groups.
Results
A total of 99 lesions from 99 patients were included in this study. Fifty-two patients were allocated into ICG and 47 patients were allocated into NCG. Delayed bleeding occurred in 1 patient from ICG and in 8 patients from NCG. Delayed perforation occurred in 1 patient from ICG and in 3 patients from NCG. There were no procedure-related deaths in both groups.
Conclusions
Although the use of endoscopic clipping seemed to reduce the risk of developing delayed complications, further studies using a prospective design is required.
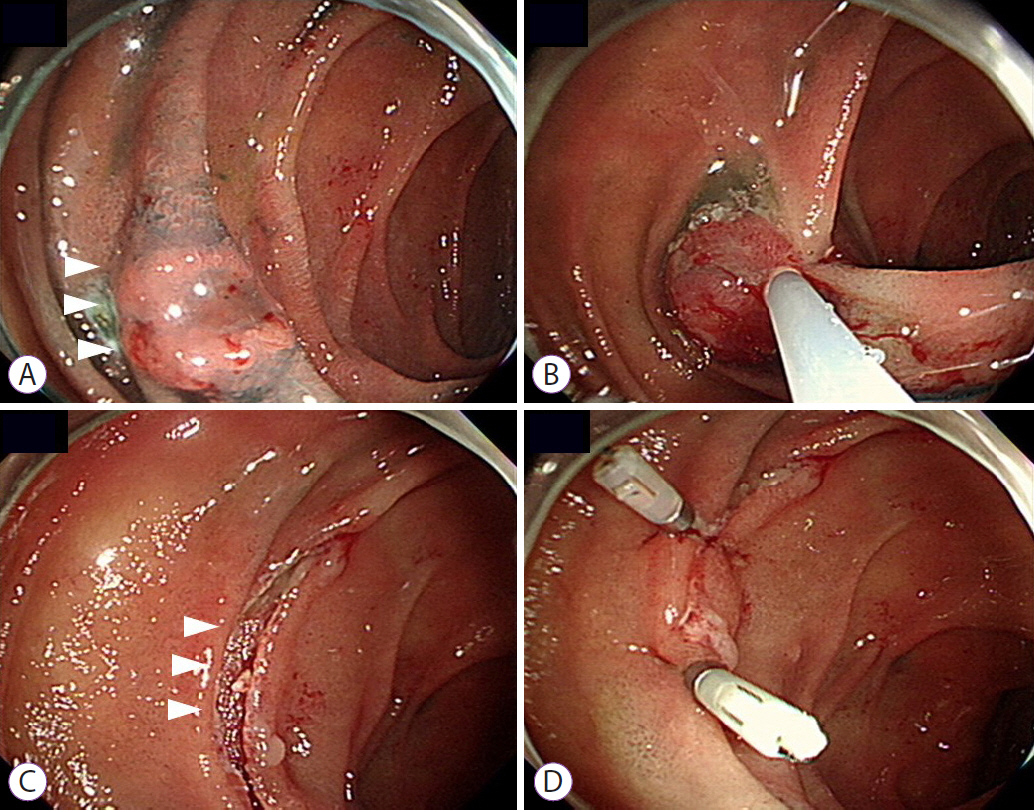
Figure
Cited by 1 articles
-
Endoscopic Closure After Endoscopic Resection for Superficial Non-Ampullary Duodenal Tumors
Satoshi Tanabe, Takuya Wada
Clin Endosc. 2021;54(4):453-454. doi: 10.5946/ce.2021.123.
Reference
-
1. Fu YW, Lin MS, Yang B, Yu H, Jiao X, Huang JX. An early superficial non-ampullary duodenal tumor cured with endoscopic submucosal dissection: a case report. Oncol Lett. 2017; 14:3755–3759.
Article2. Klein A, Nayyar D, Bahin FF, et al. Endoscopic mucosal resection of large and giant lateral spreading lesions of the duodenum: success, adverse events, and long-term outcomes. Gastrointest Endosc. 2016; 84:688–696.
Article3. Shibagaki K, Ishimura N, Kinoshita Y. Endoscopic submucosal dissection for duodenal tumors. Ann Transl Med. 2017; 5:188.
Article4. Cortese AF, Cornell GN. Carcinoma of the duodenum. Cancer. 1972; 29:1010–1015.
Article5. Kakushima N, Kanemoto H, Tanaka M, Takizawa K, Ono H. Treatment for superficial non-ampullary duodenal epithelial tumors. World J Gastroenterol. 2014; 20:12501–12508.
Article6. Valerii G, Tringali A, Landi R, et al. Endoscopic mucosal resection of non-ampullary sporadic duodenal adenomas: a retrospective analysis with long-term follow-up. Scand J Gastroenterol. 2018; 53:490–494.
Article7. Pérez-Cuadrado-Robles E, Quénéhervé L, Margos W, et al. Comparative analysis of ESD versus EMR in a large European series of non-ampullary superficial duodenal tumors. Endosc Int Open. 2018; 6:E1008–E1014.
Article8. Pérez-Cuadrado-Robles E, Quénéhervé L, Margos W, et al. ESD versus EMR in non-ampullary superficial duodenal tumors: a systematic review and meta-analysis. Endosc Int Open. 2018; 6:E998–E1007.
Article9. Inoue T, Uedo N, Yamashina T, et al. Delayed perforation: a hazardous complication of endoscopic resection for non-ampullary duodenal neoplasm. Dig Endosc. 2014; 26:220–227.
Article10. Hoteya S, Kaise M, Iizuka T, et al. Delayed bleeding after endoscopic submucosal dissection for non-ampullary superficial duodenal neoplasias might be prevented by prophylactic endoscopic closure: analysis of risk factors. Dig Endosc. 2015; 27:323–330.
Article11. Fanning SB, Bourke MJ, Williams SJ, Chung A, Kariyawasam VC. Giant laterally spreading tumors of the duodenum: endoscopic resection outcomes, limitations, and caveats. Gastrointest Endosc. 2012; 75:805–812.
Article12. Hoteya S, Furuhata T, Takahito T, et al. Endoscopic submucosal dissection and endoscopic mucosal resection for non-ampullary superficial duodenal tumor. Digestion. 2017; 95:36–42.
Article13. Fujihara S, Mori H, Kobara H, et al. Management of a large mucosal defect after duodenal endoscopic resection. World J Gastroenterol. 2016; 22:6595–6609.
Article14. Tashima T, Ohata K, Sakai E, et al. Efficacy of an over-the-scope clip for preventing adverse events after duodenal endoscopic submucosal dissection: a prospective interventional study. Endoscopy. 2018; 50:487–496.
Article15. Doyama H, Tominaga K, Yoshida N, Takemura K, Yamada S. Endoscopic tissue shielding with polyglycolic acid sheets, fibrin glue and clips to prevent delayed perforation after duodenal endoscopic resection. Dig Endosc. 2014; 26(Suppl 2):41–45.
Article16. Yahagi N, Kato M, Ochiai Y, et al. Outcomes of endoscopic resection for superficial duodenal epithelial neoplasia. Gastrointest Endosc. 2018; 88:676–682.
Article17. Ye LP, Mao XL, Zheng HH, et al. Safety of endoscopic resection for duodenal subepithelial lesions with wound closure using clips and an endoloop: an analysis of 68 cases. Surg Endosc. 2017; 31:1070–1077.
Article18. Kato M, Ochiai Y, Fukuhara S, et al. Clinical impact of closure of the mucosal defect after duodenal endoscopic submucosal dissection. Gastrointest Endosc. 2019; 89:87–93.
Article19. Fujiwara S, Morita Y, Toyonaga T, et al. A randomized controlled trial of rebamipide plus rabeprazole for the healing of artificial ulcers after endoscopic submucosal dissection. J Gastroenterol. 2011; 46:595–602.
Article20. Nishizawa T, Suzuki H, Goto O, Ogata H, Kanai T, Yahagi N. Effect of prophylactic clipping in colorectal endoscopic resection: a meta-analysis of randomized controlled studies. United European Gastroenterol J. 2017; 5:859–867.
Article21. Feagins LA, Nguyen AD, Iqbal R, Spechler SJ. The prophylactic placement of hemoclips to prevent delayed post-polypectomy bleeding: an unnecessary practice? A case control study. Dig Dis Sci. 2014; 59:823–828.
Article22. Shirai Y, Ohki T, Yamamoto M. Application of the clip method, using thread, for duodenal endoscopic mucosal resection. BMJ Case Rep. 2016; 2016:bcr2016215677.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Resection for Superficial Non-Ampullary Duodenal Epithelial Tumors
- Non-Ampullary Duodenal Tumors
- Current Treatment Strategy for Superficial Nonampullary Duodenal Epithelial Tumors
- The Role of Endoscopy in Diagnosis and Treatment of Ampullary Tumor
- Endoscopic Treatment for Superficial Nonampullary Duodenal Tumors