Intest Res.
2021 Jul;19(3):282-290. 10.5217/ir.2020.00010.
Trends of inflammatory bowel disease at a tertiary care center in northern India
- Affiliations
-
- 1Department of Gastroenterology, Dayanand Medical College and Hospital, Ludhiana, India
- 2Department of Pharmacology, Dayanand Medical College and Hospital, Ludhiana, India
- 3Department of Internal Medicine, Dayanand Medical College and Hospital, Ludhiana, India
- 4Research and Development Centre, Dayanand Medical College and Hospital, Ludhiana, India
- KMID: 2518684
- DOI: http://doi.org/10.5217/ir.2020.00010
Abstract
- Background/Aims
Inflammatory bowel disease (IBD), including ulcerative colitis (UC) and Crohn’s disease (CD), is increasingly being reported from India and other Asian countries. This study looks into the changing trends of IBD at a tertiary care center in north India over last two decades.
Methods
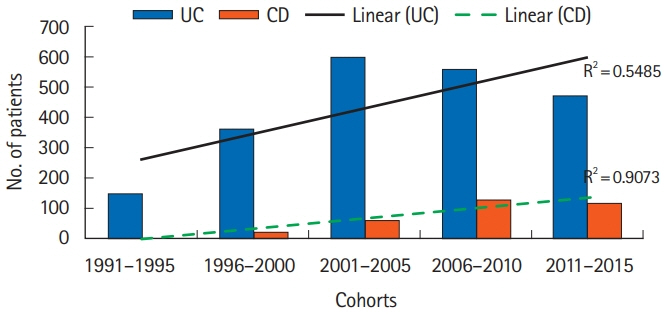
Retrospective analysis of a prospectively maintained database of patients diagnosed with IBD between January 1991 and December 2015 was conducted. The study period was divided into five times cohorts (1991–1995, 1996–2000, 2001–2005, 2006–2010, 2011–2015).
Results
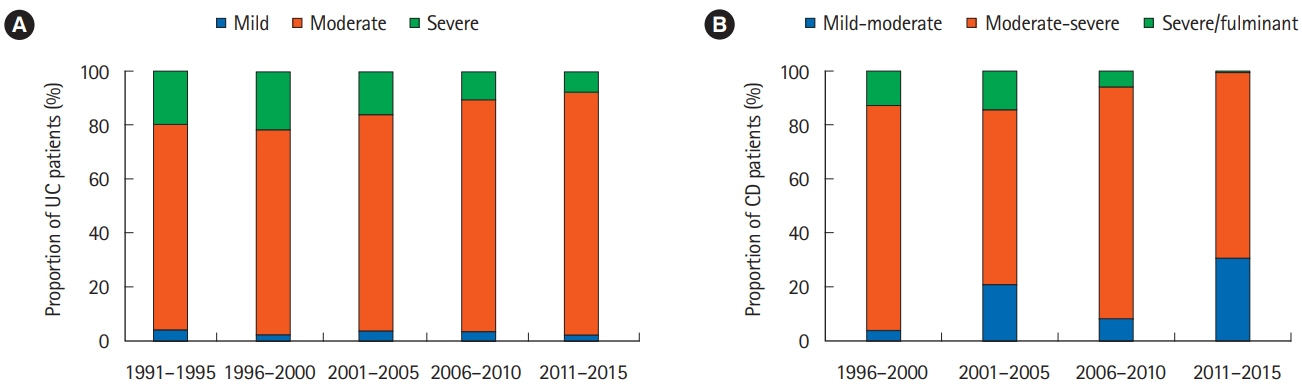
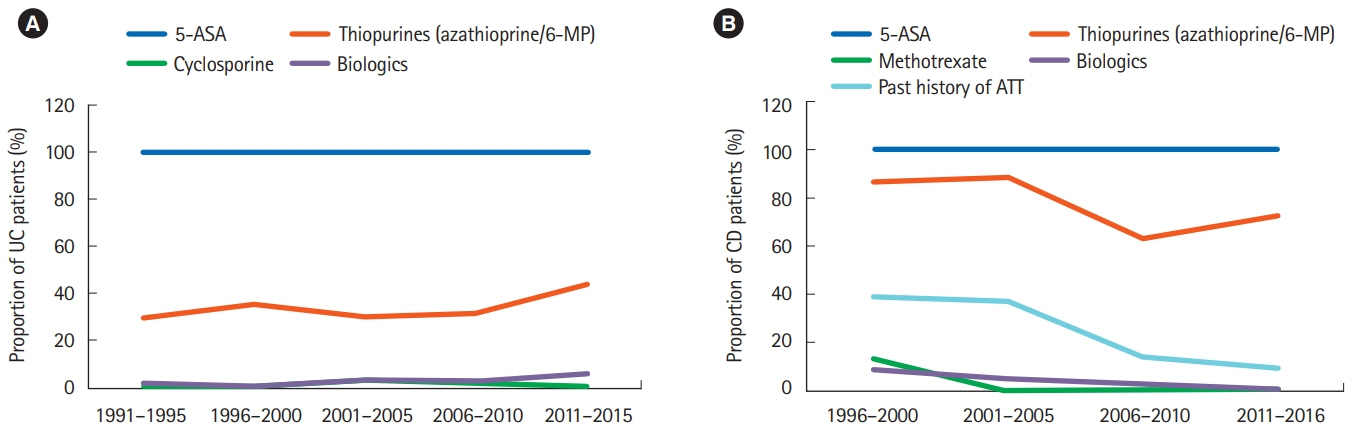
During the study period, 2,467 patients (UC [n = 2,137, 86.6%], CD [n = 330, 13.3%], mean age 38.5 ± 13.3 years; 55.9% males) were registered. The proportion of patients with CD increased (ratio of UC to CD declined from 15.7:1 to 4:1). The mean age at diagnosis decreased for UC (45.7 ± 12.1 years in 1991–1995 vs. 37.6 ± 13.0 years in 2011–2015; P= 0.001) and remained consistent for CD (41.3 ± 13.6 years in 1996–2000 vs. 41.3 ± 16.9 years in 2011–2015, P= 0.86). Patients with proctitis in UC and isolated ileal disease in CD increased over the study period (P= 0.001 and P= 0.007, respectively). Inflammatory CD increased (P= 0.009) whereas stricturing CD decreased (P= 0.01) across all cohorts. There was a trend towards less severe presentation of both UC and CD. The use of thiopurines (P= 0.02) and biologics increased (P= 0.001) with no significant change in trends for requirements of surgery (P= 0.9).
Conclusions
Increasing prevalence of CD, younger age at diagnosis, diagnosis at an earlier and milder stage, greater use of thiopurines and biologics were observed.
Figure
Cited by 2 articles
-
Update on the epidemiology of inflammatory bowel disease in Asia: where are we now?
Sang Hyoung Park
Intest Res. 2022;20(2):159-164. doi: 10.5217/ir.2021.00115.Real-world effectiveness and safety of ustekinumab induction therapy for Korean patients with Crohn’s disease: a KASID prospective multicenter study
Kyunghwan Oh, Hee Seung Hong, Nam Seok Ham, Jungbok Lee, Sang Hyoung Park, Suk-Kyun Yang, Hyuk Yoon, You Sun Kim, Chang Hwan Choi, Byong Duk Ye
Intest Res. 2023;21(1):137-147. doi: 10.5217/ir.2021.00173.
Reference
-
1. Morita N, Toki S, Hirohashi T, et al. Incidence and prevalence of inflammatory bowel disease in Japan: nationwide epidemiological survey during the year 1991. J Gastroenterol. 1995; 30(Suppl 8):1–4.2. Asakura K, Nishiwaki Y, Inoue N, Hibi T, Watanabe M, Takebayashi T. Prevalence of ulcerative colitis and Crohn’s disease in Japan. J Gastroenterol. 2009; 44:659–665.
Article3. Sood A, Midha V, Sood N, Bhatia AS, Avasthi G. Incidence and prevalence of ulcerative colitis in Punjab, North India. Gut. 2003; 52:1587–1590.
Article4. Yang SK, Hong WS, Min YI, et al. Incidence and prevalence of ulcerative colitis in the Songpa-Kangdong district, Seoul, Korea, 1986-1997. J Gastroenterol Hepatol. 2000; 15:1037–1042.
Article5. Lai CL, Wu PC, Wong KL, Lok ASF. Clinical features of ulcerative proctocolitis in Hong Kong Chinese: a review of three decades. Am J Proctol Gastroenterol Colon Rectal Surg. 1985; 36:14–19.6. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986-2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549.
Article7. Makharia GK, Ramakrishna BS, Abraham P, et al. Survey of inflammatory bowel diseases in India. Indian J Gastroenterol. 2012; 31:299–306.
Article8. Munkholm P. Crohn’s disease: occurrence, course and prognosis: an epidemiologic cohort-study. Dan Med Bull. 1997; 44:287–302.9. Langholz E. Ulcerative colitis: an epidemiological study based on a regional inception cohort, with special reference to disease course and prognosis. Dan Med Bull. 1999; 46:400–415.10. Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006; 55:749–753.
Article11. Levine A, Griffiths A, Markowitz J, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis. 2011; 17:1314–1321.
Article12. Best WR, Becktel JM, Singleton JW, Kern F Jr. Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology. 1976; 70:439–444.13. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987; 317:1625–1629.
Article14. Kedia S, Ahuja V. Epidemiology of inflammatory bowel disease in India: the great shift East. Inflamm Intest Dis. 2017; 2:102–115.
Article15. Loftus EV Jr. Clinical epidemiology of inflammatory bowel disease: incidence, prevalence, and environmental influences. Gastroenterology. 2004; 126:1504–1517.
Article16. Moum B, Vatn MH, Ekbom A, et al. Incidence of Crohn’s disease in four counties in southeastern Norway, 1990-93: a prospective population-based study. The Inflammatory Bowel South-Eastern Norway (IBSEN) Study Group of Gastroenterologists. Scand J Gastroenterol. 1996; 31:355–361.
Article17. Moum B, Vatn MH, Ekbom A, et al. Incidence of ulcerative colitis and indeterminate colitis in four counties of southeastern Norway, 1990-93: a prospective population-based study. The Inflammatory Bowel South-Eastern Norway (IBSEN) Study Group of Gastroenterologists. Scand J Gastroenterol. 1996; 31:362–366.
Article18. Loftus EV Jr, Silverstein MD, Sandborn WJ, Tremaine WJ, Harmsen WS, Zinsmeister AR. Crohn’s disease in Olmsted County, Minnesota, 1940-1993: incidence, prevalence, and survival. Gastroenterology. 1998; 114:1161–1168.
Article19. International Institute for Population Sciences. National Family Health Survey (NFHS-4), 2015-16 [Internet]. c2017 [cited 2020 Jan 7]. http://www.rchiips.org/nfhs/nfhs4.shtml.20. Solberg IC, Vatn MH, Høie O, et al. Clinical course in Crohn’s disease: results of a Norwegian population-based ten-year follow-up study. Clin Gastroenterol Hepatol. 2007; 5:1430–1438.
Article21. Das K, Ghoshal UC, Dhali GK, Benjamin J, Ahuja V, Makharia GK. Crohn’s disease in India: a multicenter study from a country where tuberculosis is endemic. Dig Dis Sci. 2009; 54:1099–1107.
Article22. Kalaria R, Desai D, Abraham P, Joshi A, Gupta T, Shah S. Temporal change in phenotypic behaviour in patients with Crohn’s disease: do Indian patients behave differently from Western and other Asian patients? J Crohns Colitis. 2016; 10:255–261.
Article23. Sood A, Midha V, Sood N, Bansal M. Long term results of use of azathioprine in patients with ulcerative colitis in India. World J Gastroenterol. 2006; 12:7332–7336.
Article24. Sood A, Midha V, Sood N, Avasthi G. Azathioprine versus sulfasalazine in maintenance of remission in severe ulcerative colitis. Indian J Gastroenterol. 2003; 22:79–81.25. Sood A, Kaushal V, Midha V, Bhatia KL, Sood N, Malhotra V. The beneficial effect of azathioprine on maintenance of remission in severe ulcerative colitis. J Gastroenterol. 2002; 37:270–274.
Article26. Bopanna S, Ananthakrishnan AN, Kedia S, Yajnik V, Ahuja V. Risk of colorectal cancer in Asian patients with ulcerative colitis: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2017; 2:269–276.
Article27. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010; 127:2893–2917.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Rickettsial Infections among the Undifferentiated Febrile Patients Attending a Tertiary Care Teaching Hospital of Northern India: A Longitudinal Study
- Prevalence of Irritable Bowel Syndrome in Northern India
- Psychiatric Co-morbidity in Patients With Irritable Bowel Syndrome at a Tertiary Care Center in Northern India
- Pivot to Asia: inflammatory bowel disease burden
- Retrospective review of severe acute respiratory syndrome coronavirus-2 infection in children with acute leukemia from a tertiary care hospital in Northern India