Korean J Orthod.
2021 Jul;51(4):260-269. 10.4041/kjod.2021.51.4.260.
Quantitative cone-beam computed tomography evaluation of hard and soft tissue thicknesses in the midpalatal suture region to facilitate orthodontic mini-implant placement
- Affiliations
-
- 1Department of Oral and Maxillofacial Radiology, Graduate School, Kyung Hee University, Seoul, Korea
- 2Department of Orthodontics, Graduate School, Kyung Hee University, Seoul, Korea
- KMID: 2518519
- DOI: http://doi.org/10.4041/kjod.2021.51.4.260
Abstract
Objective
To identify the most favorable sites that optimize the initial stability and survival rate of orthodontic mini-implants, this study measured hard and soft tissue thicknesses in the median and paramedian regions of the palate using cone-beam computed tomography (CBCT) and determined possible sexand age-related differences in these thicknesses.
Methods
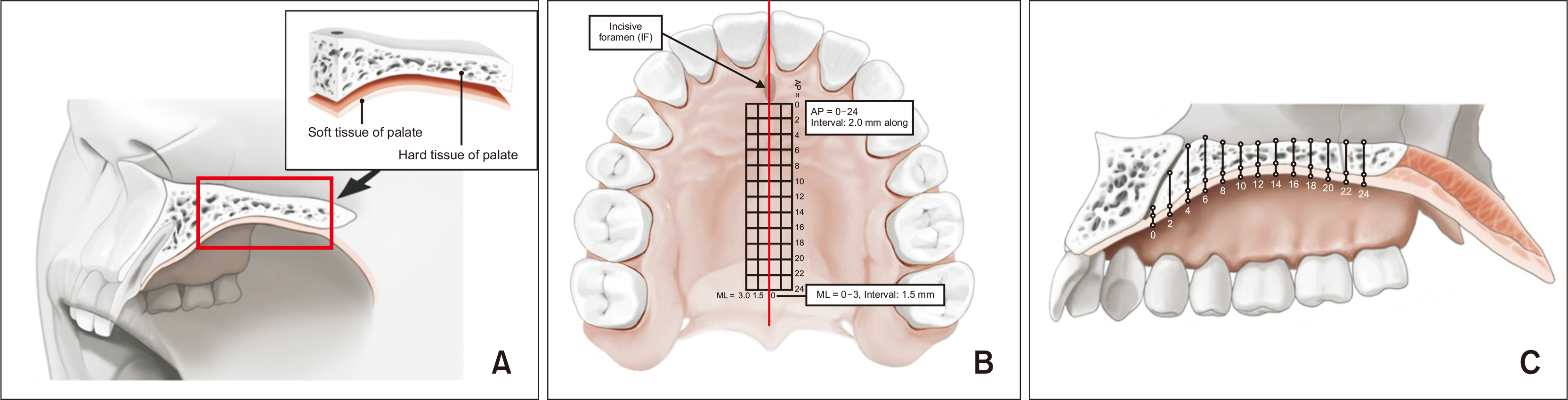
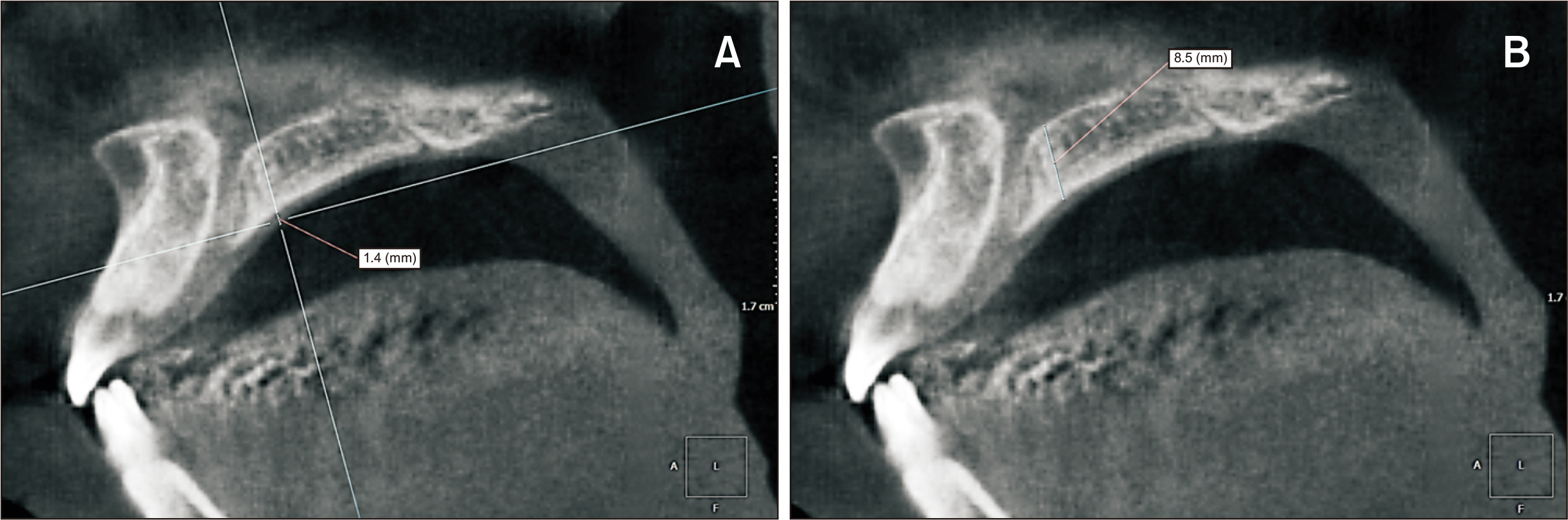
The study sample comprised CBCT images of 189 healthy subjects. The sample was divided into four groups according to age. A grid area was set for the measurement of hard and soft tissue thicknesses in the palate. Vertical lines were marked at intervals of 0, 1.5, and 3.0 mm lateral to the midpalatal suture, while horizontal lines were marked at 2-mm intervals up to 24 mm from the posterior margin of the incisive foramen. Measurements were made at 65 points of intersection between the horizontal and vertical lines.
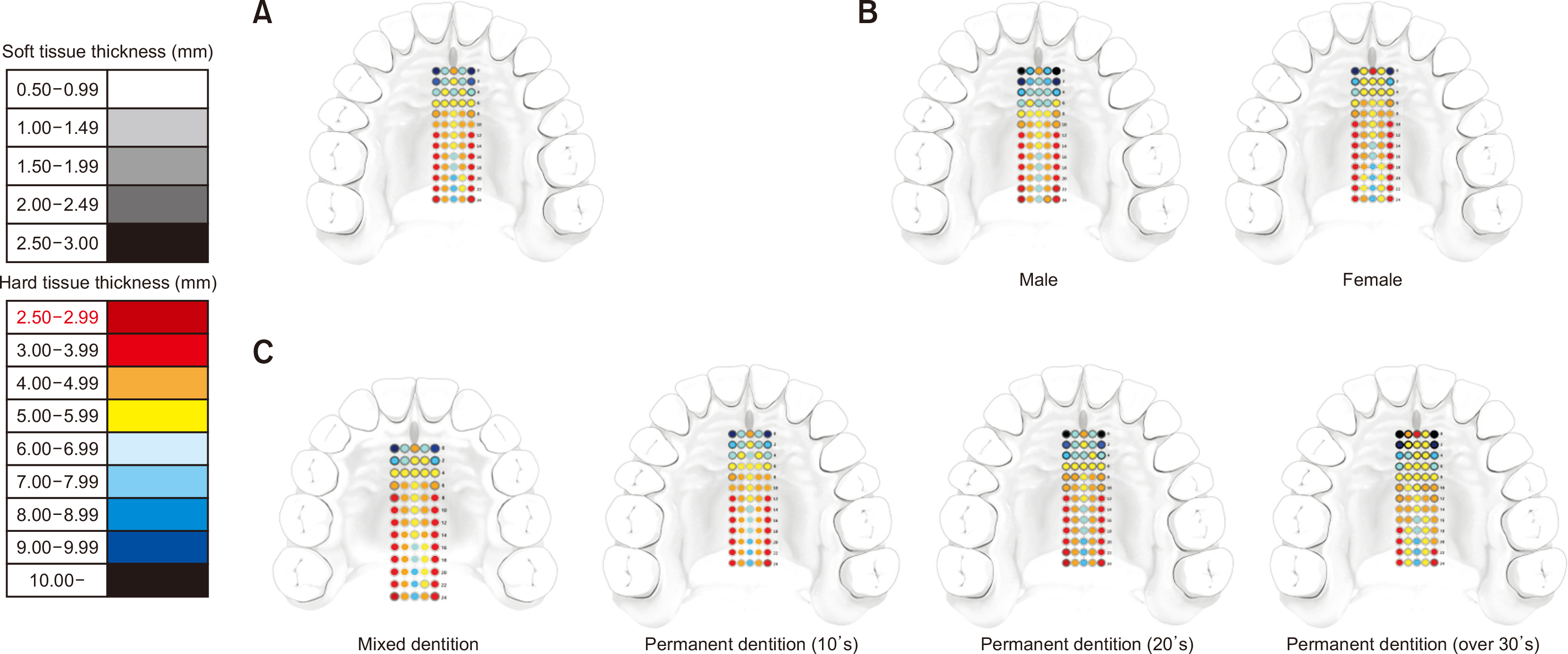
Results
The palatal hard tissue thickness decreased from the anterior to the posterior region, with a decrease in the medial-to-lateral direction in the middle and posterior regions. While the soft tissue was rather thick around the lateral aspects of the palatal arch, it formed a constant layer that was only 1–2-mm thick throughout the palate. Statistically significant differences were observed according to sex and age.
Conclusions
The anterolateral palate as well as the midpalatal suture seem to be the most favorable sites for insertion of orthodontic mini-implants. The thickness of the palate differed by age and sex; these differences should be considered while planning the placement of orthodontic mini-implants.
Figure
Reference
-
1. Janssen KI, Raghoebar GM, Vissink A, Sandham A. 2008; Skeletal anchorage in orthodontics--a review of various systems in animal and human studies. Int J Oral Maxillofac Implants. 23:75–88. PMID: 18416415.2. Seo YJ, Chung KR, Kim SH, Nelson G. 2015; Camouflage treatment of skeletal class III malocclusion with asymmetry using a bone-borne rapid maxillary expander. Angle Orthod. 85:322–34. DOI: 10.2319/031314-189.1. PMID: 25032737.
Article3. Lee KJ, Park YC, Park JY, Hwang WS. 2010; Miniscrew-assisted nonsurgical palatal expansion before orthognathic surgery for a patient with severe mandibular prognathism. Am J Orthod Dentofacial Orthop. 137:830–9. DOI: 10.1016/j.ajodo.2007.10.065. PMID: 20685540.
Article4. Celenk-Koca T, Erdinc AE, Hazar S, Harris L, English JD, Akyalcin S. 2018; Evaluation of miniscrew-supported rapid maxillary expansion in adolescents: a prospective randomized clinical trial. Angle Orthod. 88:702–9. DOI: 10.2319/011518-42.1. PMID: 30102085. PMCID: PMC8174075.
Article5. Kyung SH. 2004; A study on the bone thickness of midpalatal suture area for miniscrew insertion. Korean J Orthod. 34:63–70.6. Kim HJ, Yun HS, Park HD, Kim DH, Park YC. 2006; Soft-tissue and cortical-bone thickness at orthodontic implant sites. Am J Orthod Dentofacial Orthop. 130:177–82. DOI: 10.1016/j.ajodo.2004.12.024. PMID: 16905061.
Article7. Keles A, Erverdi N, Sezen S. 2003; Bodily distalization of molars with absolute anchorage. Angle Orthod. 73:471–82. DOI: 10.1043/0003-3219(2003)073<0471:BDOMWA>2.0.CO;2. PMID: 12940570.8. Poorsattar-Bejeh Mir A, Haghanifar S, Poorsattar-Bejeh Mir M, Rahmati-Kamel M. 2017; Individual scoring and mapping of hard and soft tissues of the anterior hard palate for orthodontic miniscrew insertion. J Investig Clin Dent. 8:e12186. DOI: 10.1111/jicd.12186. PMID: 26446347.
Article9. Lyu X, Guo J, Chen L, Gao Y, Liu L, Pu L, et al. 2020; Assessment of available sites for palatal orthodontic mini-implants through cone-beam computed tomography. Angle Orthod. 90:516–23. DOI: 10.2319/070719-457.1. PMID: 33378492. PMCID: PMC8028458.
Article10. Bjöerk A, Krebs A, Solow B. 1964; A method for epidemiological registration of malocclusion. Acta Odontol Scand. 22:27–41. DOI: 10.3109/00016356408993963. PMID: 14158468.11. Kang S, Lee SJ, Ahn SJ, Heo MS, Kim TW. 2007; Bone thickness of the palate for orthodontic mini-implant anchorage in adults. Am J Orthod Dentofacial Orthop. 131(4 Suppl):S74–81. DOI: 10.1016/j.ajodo.2005.09.029. PMID: 17448390.
Article12. Ryu JH, Park JH, Vu Thi Thu T, Bayome M, Kim Y, Kook YA. 2012; Palatal bone thickness compared with cone-beam computed tomography in adolescents and adults for mini-implant placement. Am J Orthod Dentofacial Orthop. 142:207–12. DOI: 10.1016/j.ajodo.2012.03.027. PMID: 22858330.
Article13. Schoenwolf GC, Bleyl SB, Brauer PR, Francis-West PH. 2015. Larsen's human embryology. 5th ed. Churchill Livingstone;Philadelphia:14. Chhatwani S, Rose-Zierau V, Haddad B, Almuzian M, Kirschneck C, Danesh G. 2019; Three-dimensional quantitative assessment of palatal bone height for insertion of orthodontic implants - a retrospective CBCT study. Head Face Med. 15:9. DOI: 10.1186/s13005-019-0193-9. PMID: 30935392. PMCID: PMC6442434.
Article15. Wehrbein H, Merz BR, Diedrich P, Glatzmaier J. 1996; The use of palatal implants for orthodontic anchorage. Design and clinical application of the orthosystem. Clin Oral Implants Res. 7:410–6. DOI: 10.1034/j.1600-0501.1996.070416.x. PMID: 9151610.
Article16. Wehrbein H, Merz BR, Diedrich P. 1999; Palatal bone support for orthodontic implant anchorage--a clinical and radiological study. Eur J Orthod. 21:65–70. DOI: 10.1093/ejo/21.1.65. PMID: 10191579.17. Bernhart T, Freudenthaler J, Dörtbudak O, Bantleon HP, Watzek G. 2001; Short epithetic implants for orthodontic anchorage in the paramedian region of the palate. A clinical study. Clin Oral Implants Res. 12:624–31. DOI: 10.1034/j.1600-0501.2001.120611.x. PMID: 11737107.18. Choi SH, Shi KK, Cha JY, Park YC, Lee KJ. 2016; Nonsurgical miniscrew-assisted rapid maxillary expansion results in acceptable stability in young adults. Angle Orthod. 86:713–20. DOI: 10.2319/101415-689.1. PMID: 26938955.
Article19. Yadav S, Sachs E, Vishwanath M, Knecht K, Upadhyay M, Nanda R, et al. 2018; Gender and growth variation in palatal bone thickness and density for mini-implant placement. Prog Orthod. 19:43. DOI: 10.1186/s40510-018-0241-1. PMID: 30393829. PMCID: PMC6215790.
Article20. Cassetta M, Sofan AA, Altieri F, Barbato E. 2013; Evaluation of alveolar cortical bone thickness and density for orthodontic mini-implant placement. J Clin Exp Dent. 5:e245–52. DOI: 10.4317/jced.51228. PMID: 24455090. PMCID: PMC3892271.
Article21. Chen YJ, Chang HH, Lin HY, Lai EH, Hung HC, Yao CC. 2008; Stability of miniplates and miniscrews used for orthodontic anchorage: experience with 492 temporary anchorage devices. Clin Oral Implants Res. 19:1188–96. DOI: 10.1111/j.1600-0501.2008.01571.x. PMID: 18983323.
Article22. Yao CC, Chang HH, Chang JZ, Lai HH, Lu SC, Chen YJ. 2015; Revisiting the stability of mini-implants used for orthodontic anchorage. J Formos Med Assoc. 114:1122–8. DOI: 10.1016/j.jfma.2014.08.001. PMID: 25260551.
Article23. Baumgaertel S. 2014; Hard and soft tissue considerations at mini-implant insertion sites. J Orthod. 41 Suppl 1:S3–7. DOI: 10.1179/1465313314Y.0000000104. PMID: 25138363.
Article24. Kim JS, Kim SH, Kook YA, Chung KR, Nelson G. 2011; Analysis of lingual en masse retraction combining a C-lingual retractor and a palatal plate. Angle Orthod. 81:662–9. DOI: 10.2319/100110-574.1. PMID: 21406002.
Article25. Kim YT, Lee JH, Jeong SN. 2020; Three-dimensional observations of the incisive foramen on cone-beam computed tomography image analysis. J Periodontal Implant Sci. 50:48–55. DOI: 10.5051/jpis.2020.50.1.48. PMID: 32128273. PMCID: PMC7040439.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of the Midpalatal Suture Maturation in Young Koreans Using Cone-Beam Computed Tomography
- Maxillary Soft Tissue and Cortical Bone Thickness for Mini-implant Placement
- Quantitative evaluation of midpalatal suture maturation via fractal analysis
- Assessment of Midpalatal Suture Maturation by Skeletal Maturity on Hand Wrist Radiographs
- Buccal cortical bone thickness on CBCT for mini-implant