J Korean Med Sci.
2021 Jul;36(27):e186. 10.3346/jkms.2021.36.e186.
Incidence and Risk of Venous Thromboembolism in Bisphosphonates and Selective Estrogen Receptor Modulators Treatment in Korea
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Kyung Hee University Hospital, Seoul, Korea
- 2Department of Internal Medicine, Catholic Kwandong University College of Medicine, International St. Mary's Hospital, Incheon, Korea
- 3Department of Orthopaedic Surgery, School of Medicine, Konkuk University, Seoul, Korea
- 4Department of Orthopaedic Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 5Department of Orthopaedic Surgery, College of Medicine, Chung-Ang University, Seoul, Korea
- 6College of Pharmacy and Gachon Institute of Pharmaceutical Sciences, Gachon University, Incheon, Korea
- 7Division of Endocrinology and Metabolism, Department of Internal Medicine, Inha University Hospital, Inha University School of Medicine, Incheon, Korea
- 8Department of Internal Medicine, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea
- KMID: 2518352
- DOI: http://doi.org/10.3346/jkms.2021.36.e186
Abstract
- Background
Selective estrogen receptor modulators (SERMs) were associated with an increased risk of venous thromboembolism (VTE) due to the estrogen effect. In this study, we investigated the effect of SERMs on VTE compared to bisphosphonates (BPs) using the Korean National Health Insurance claims database.
Methods
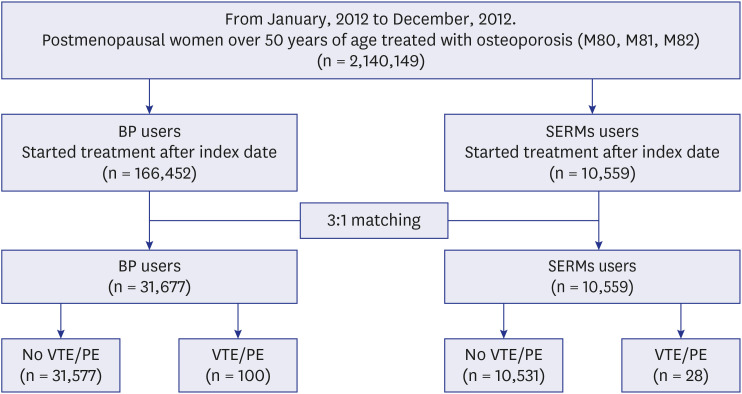
This was a retrospective cohort study. Women over 50 years old who were first prescribed BPs or SERMs for osteoporosis treatment in 2012 were included. The difference in VTE incidence between the SERMs and BP groups was compared. Both groups were followed up for VTE or PE occurrence, death, or until December 2016. The study population was analyzed by 3:1 matching according to age using a multivariate Cox model.
Results
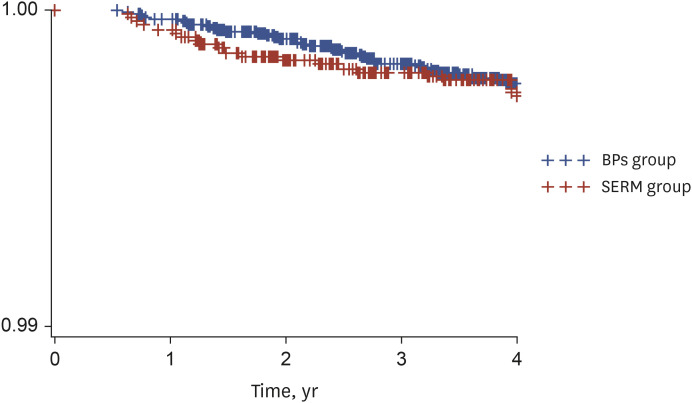
The hazard ratio (HR) for VTE was 0.72 (95% confidence interval [CI], 0.40–1.28) in the SERMs group compared to BP group. Older age (60–69 vs. 50–59 years: HR, 3.77; 95% CI, 2.07–6.86 and 70–79 vs. 50–59 years: HR, 5.88; 95% CI, 3.14–11.02), major osteoporotic fracture (HR, 1.77; 95% CI, 1.16- 2.70), atrial fibrillation (HR, 3.31; 95% CI, 1.35–8.11), and estrogen replacement (HR, 3.40; 95% CI, 2.01–5.73) all increased VTE risk. In subgroup analysis of the SERMs group, past hospitalization (HR, 2.24; 95% CI, 1.02–4.92), estrogen replacement (HR, 5.75; 95% CI, 2.29–14.39), and glucocorticoid replacement (HR, 2.71; 95% CI, 1.05–7.0) increased VTE risk.
Conclusion
SERMs did not increase the risk of VTE compared to BPs in Koreans with osteoporosis. However, old age and estrogen replacement both increased VTE risk.
Keyword
Figure
Reference
-
1. Cauley JA. Estrogen and bone health in men and women. Steroids. 2015; 99(Pt A):11–15. PMID: 25555470.
Article2. Eastell R, Rosen CJ, Black DM, Cheung AM, Murad MH, Shoback D. Pharmacological management of osteoporosis in postmenopausal women: an Endocrine Society* Clinical Practice Guideline. J Clin Endocrinol Metab. 2019; 104(5):1595–1622. PMID: 30907953.
Article3. Mirkin S, Pickar JH. Selective estrogen receptor modulators (SERMs): a review of clinical data. Maturitas. 2015; 80(1):52–57. PMID: 25466304.
Article4. Manson JE, Chlebowski RT, Stefanick ML, Aragaki AK, Rossouw JE, Prentice RL, et al. Menopausal hormone therapy and health outcomes during the intervention and extended poststopping phases of the Women's Health Initiative randomized trials. JAMA. 2013; 310(13):1353–1368. PMID: 24084921.5. Barrett-Connor E, Mosca L, Collins P, Geiger MJ, Grady D, Kornitzer M, et al. Effects of raloxifene on cardiovascular events and breast cancer in postmenopausal women. N Engl J Med. 2006; 355(2):125–137. PMID: 16837676.
Article6. Adomaityte J, Farooq M, Qayyum R. Effect of raloxifene therapy on venous thromboembolism in postmenopausal women. A meta-analysis. Thromb Haemost. 2008; 99(2):338–342. PMID: 18278183.
Article7. Black DM, Delmas PD, Eastell R, Reid IR, Boonen S, Cauley JA, et al. Once-yearly zoledronic acid for treatment of postmenopausal osteoporosis. N Engl J Med. 2007; 356(18):1809–1822. PMID: 17476007.
Article8. Cummings SR, Schwartz AV, Black DM. Alendronate and atrial fibrillation. N Engl J Med. 2007; 356(18):1895–1896. PMID: 17476024.
Article9. Vestergaard P, Schwartz K, Pinholt EM, Rejnmark L, Mosekilde L. Use of bisphosphonates and raloxifene and risk of deep venous thromboembolism and pulmonary embolism. Osteoporos Int. 2010; 21(9):1591–1597. PMID: 19859641.
Article10. Breart G, Cooper C, Meyer O, Speirs C, Deltour N, Reginster JY. Osteoporosis and venous thromboembolism: a retrospective cohort study in the UK General Practice Research Database. Osteoporos Int. 2010; 21(7):1181–1187. PMID: 19806285.
Article11. Lin TC, Lee CH, Yang CY, Yang YH, Lin SJ. Incidence and risk of venous thromboembolism among Taiwan osteoporotic fracture population under osteoporosis pharmacological treatments. J Clin Endocrinol Metab. 2014; 99(5):1599–1607. PMID: 24606074.
Article12. Tans G, Curvers J, Middeldorp S, Thomassen MC, Meijers JC, Prins MH, et al. A randomized cross-over study on the effects of levonorgestrel- and desogestrel-containing oral contraceptives on the anticoagulant pathways. Thromb Haemost. 2000; 84(1):15–21. PMID: 10928463.
Article13. Middeldorp S, Meijers JC, van den Ende AE, van Enk A, Bouma BN, Tans G, et al. Effects on coagulation of levonorgestrel- and desogestrel-containing low dose oral contraceptives: a cross-over study. Thromb Haemost. 2000; 84(1):4–8. PMID: 10928461.
Article14. Meijers JC, Middeldorp S, Tekelenburg W, van den Ende AE, Tans G, Prins MH, et al. Increased fibrinolytic activity during use of oral contraceptives is counteracted by an enhanced factor XI-independent down regulation of fibrinolysis: a randomized cross-over study of two low-dose oral contraceptives. Thromb Haemost. 2000; 84(1):9–14. PMID: 10928462.15. Tchaikovski SN, Rosing J. Mechanisms of estrogen-induced venous thromboembolism. Thromb Res. 2010; 126(1):5–11. PMID: 20163835.
Article16. Heckbert SR, Li G, Cummings SR, Smith NL, Psaty BM. Use of alendronate and risk of incident atrial fibrillation in women. Arch Intern Med. 2008; 168(8):826–831. PMID: 18443257.
Article17. Loke YK, Jeevanantham V, Singh S. Bisphosphonates and atrial fibrillation: systematic review and meta-analysis. Drug Saf. 2009; 32(3):219–228. PMID: 19338379.18. Bunch TJ, Anderson JL, May HT, Muhlestein JB, Horne BD, Crandall BG, et al. Relation of bisphosphonate therapies and risk of developing atrial fibrillation. Am J Cardiol. 2009; 103(6):824–828. PMID: 19268739.
Article19. Sørensen HT, Christensen S, Mehnert F, Pedersen L, Chapurlat RD, Cummings SR, et al. Use of bisphosphonates among women and risk of atrial fibrillation and flutter: population based case-control study. BMJ. 2008; 336(7648):813–816. PMID: 18334527.
Article20. John Camm A. Review of the cardiovascular safety of zoledronic acid and other bisphosphonates for the treatment of osteoporosis. Clin Ther. 2010; 32(3):426–436. PMID: 20399982.
Article21. White RH, Keenan CR. Effects of race and ethnicity on the incidence of venous thromboembolism. Thromb Res. 2009; 123(Suppl 4):S11–S17. PMID: 19303496.
Article22. Tritschler T, Aujesky D. Venous thromboembolism in the elderly: a narrative review. Thromb Res. 2017; 155:140–147. PMID: 28550759.
Article23. Pedersen AB, Ehrenstein V, Szépligeti SK, Sørensen HT. Excess risk of venous thromboembolism in hip fracture patients and the prognostic impact of comorbidity. Osteoporos Int. 2017; 28(12):3421–3430. PMID: 28871320.
Article24. Watson T, Shantsila E, Lip GY. Mechanisms of thrombogenesis in atrial fibrillation: Virchow's triad revisited. Lancet. 2009; 373(9658):155–166. PMID: 19135613.
Article25. Anderson JA, Weitz JI. Hypercoagulable states. Crit Care Clin. 2011; 27(4):933–952. PMID: 22082521.
Article26. Jang MJ, Bang SM, Oh D. Incidence of pregnancy-associated venous thromboembolism in Korea: from the Health Insurance Review and Assessment Service database. J Thromb Haemost. 2011; 9(12):2519–2521. PMID: 21951997.
Article27. Foster SA, Foley KA, Meadows ES, Johnston JA, Wang S, Pohl GM, et al. Characteristics of patients initiating raloxifene compared to those initiating bisphosphonates. BMC Womens Health. 2008; 8(1):24. PMID: 19105828.
Article