Ann Rehabil Med.
2021 Jun;45(3):215-223. 10.5535/arm.20226.
Outcome Prediction for Patients With Ischemic Stroke in Acute Care: New Three-Level Model by Eating and Bladder Functions
- Affiliations
-
- 1Department of Rehabilitation Medicine, Nishinomiya Kyoritsu Neurosurgical Hospital, Nishinomiya, Japan
- 2Department of Rehabilitation Medicine, Hyogo College of Medicine, Nishinomiya, Japan
- KMID: 2517599
- DOI: http://doi.org/10.5535/arm.20226
Abstract
Objective
To develop a new prediction model by combining independence in eating and bladder management functions, and to assess its utility in an acute care setting.
Methods
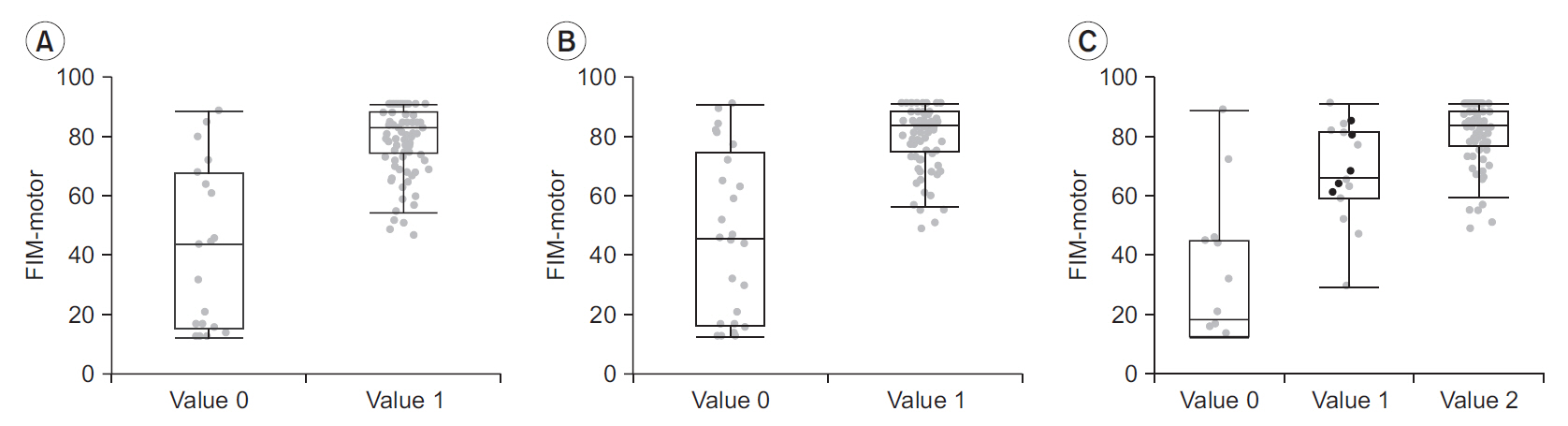
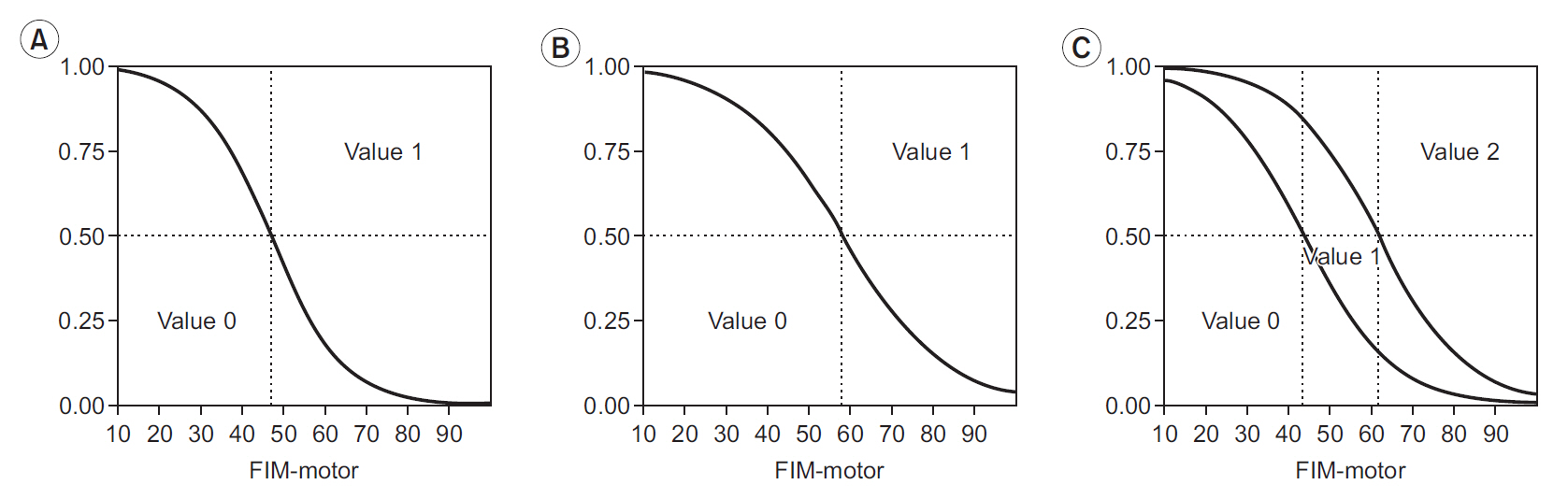
Patients with ischemic stroke who were admitted in our acute stroke care unit (n=250) were enrolled in this study. Functional Independence Measure (FIM) scores for eating and bladder management on the initial day of rehabilitative treatment (median, 3 days) were collected as predictive variables. These scores were divided into low (<5) and high (≥5) and categorized as values 0 and 1, respectively. From the simple summation of these two-level model values, we derived a three-level model that categorized the scores as values 0, 1, and 2. The FIM-motor scores at discharge (median, 14 days) were collected as outcome measurements. The three-level model was assessed by observing the distribution patterns of the outcome FIM-motor scores and logistic regression analyses.
Results
The median outcome FIM-motor score was 19 (interquartile range [IQR],13.8–45.3) for the value 0 category (n=14), 66.5 (IQR, 59.5–81.8) for the value 1 category (n=16), and 84 (IQR, 77–89) for the value 2 category (n=95) in the three-level model. Data fitting by logistic regression for FIM-motor scores of 41.3 and 61.4 reached 50% probability of values 1 and 2, respectively.
Conclusion
Despite the simplicity of the three-level model, it may be useful for predicting outcomes of patients with ischemic stroke in acute care.
Keyword
Figure
Cited by 1 articles
-
Performance of Activities of Daily Living in Typically Developing Children in Korea: Normative Value of K-MBI
Mi-Jeong Yoon, Sungwoo Paek, Jongbin Lee, Youngdeok Hwang, Joon-Sung Kim, Yeun-Jie Yoo, Bo Young Hong
Ann Rehabil Med. 2024;48(4):281-288. doi: 10.5535/arm.230040.
Reference
-
1. Miller EL, Murray L, Richards L, Zorowitz RD, Bakas T, Clark P, et al. Comprehensive overview of nursing and interdisciplinary rehabilitation care of the stroke patient: a scientific statement from the American Heart Association. Stroke. 2010; 41:2402–48.2. Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet. 2011; 377:1693–702.
Article3. Kwakkel G, Kollen BJ. Predicting activities after stroke: what is clinically relevant? Int J Stroke. 2013; 8:25–32.
Article4. Kim B, Winstein C. Can neurological biomarkers of brain impairment be used to predict poststroke motor recovery? A systematic review. Neurorehabil Neural Repair. 2017; 31:3–24.
Article5. Sagnier S, Sibon I. The new insights into human brain imaging after stroke. J Neurosci Res. 2019; Sep. 9. [Epub]. https://doi.org/10.1002/jnr.24525.
Article6. Moura LM, Luccas R, de Paiva JP, Amaro E Jr, Leemans A, Leite CD, et al. Diffusion tensor imaging biomarkers to predict motor outcomes in stroke: a narrative review. Front Neurol. 2019; 10:445.
Article7. Brott T, Adams HP Jr, Olinger CP, Marler JR, Barsan WG, Biller J, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke. 1989; 20:864–70.
Article8. Lai SM, Duncan PW, Keighley J. Prediction of functional outcome after stroke: comparison of the Orpington Prognostic Scale and the NIH Stroke Scale. Stroke. 1998; 29:1838–42.9. Saito J, Koyama T, Domen K. Long-term outcomes of FIM motor items predicted from acute stage NIHSS of patients with middle cerebral artery infarct. Ann Rehabil Med. 2018; 42:670–81.
Article10. Kwakkel G, Veerbeek JM, van Wegen EE, Nijland R, Harmeling-van der Wel BC, Dippel DW. Predictive value of the NIHSS for ADL outcome after ischemic hemispheric stroke: does timing of early assessment matter? J Neurol Sci. 2010; 294:57–61.
Article11. Koyama T, Matsumoto K, Okuno T, Domen K. A new method for predicting functional recovery of stroke patients with hemiplegia: logarithmic modelling. Clin Rehabil. 2005; 19:779–89.
Article12. Sonoda S, Saitoh E, Nagai S, Okuyama Y, Suzuki T, Suzuki M. Stroke outcome prediction using reciprocal number of initial activities of daily living status. J Stroke Cerebrovasc Dis. 2005; 14:8–11.
Article13. De Wit L, Putman K, Devos H, Brinkmann N, Dejaeger E, De Weerdt W, et al. Long-term prediction of functional outcome after stroke using single items of the Barthel Index at discharge from rehabilitation centre. Disabil Rehabil. 2014; 36:353–8.
Article14. Brown AW, Therneau TM, Schultz BA, Niewczyk PM, Granger CV. Measure of functional independence dominates discharge outcome prediction after inpatient rehabilitation for stroke. Stroke. 2015; 46:1038–44.
Article15. Granger CV, Hamilton BB, Linacre JM, Heinemann AW, Wright BD. Performance profiles of the functional independence measure. Am J Phys Med Rehabil. 1993; 72:84–9.
Article16. Stineman MG, Fiedler RC, Granger CV, Maislin G. Functional task benchmarks for stroke rehabilitation. Arch Phys Med Rehabil. 1998; 79:497–504.
Article17. Brittain KR, Peet SM, Castleden CM. Stroke and incontinence. Stroke. 1998; 29:524–8.
Article18. van Almenkerk S, Smalbrugge M, Depla MF, Eefsting JA, Hertogh CM. What predicts a poor outcome in older stroke survivors? A systematic review of the literature. Disabil Rehabil. 2013; 35:1774–82.19. Mizrahi EH, Arad M, Weiss A, Leibovitz A, Adunsky A. Eating management and functional outcome of elderly patients with symptomatic ischemic stroke undergoing inpatient rehabilitation. Geriatr Gerontol Int. 2013; 13:701–5.
Article20. Mizrahi EH, Waitzman A, Arad M, Blumstein T, Adunksy A. Bladder management and the functional outcome of elderly ischemic stroke patients. Arch Gerontol Geriatr. 2011; 53:e125–8.
Article21. Uchida K, Uchiyama Y, Domen K, Koyama T. Item difficulties of the FIM-motor subscale in patients with ischemic stroke during acute care: an ordinal logistic modeling study. Prog Rehabil Med. 2020; 5:20200022.
Article22. Koyama T, Domen K. Diffusion tensor fractional anisotropy in the superior longitudinal fasciculus correlates with Functional Independence Measure cognition scores in patients with cerebral infarction. J Stroke Cerebrovasc Dis. 2017; 26:1704–11.
Article23. Shinohara Y, Yanagihara T, Abe K, Yoshimine T, Fujinaka T, Chuma T, et al. VII. Rehabilitation. J Stroke Cerebrovasc Dis. 2011; 20(4 Suppl):S145–80.
Article24. Shinohara Y, Yanagihara T, Abe K, Yoshimine T, Fujinaka T, Chuma T, et al. II. Cerebral infarction/transient ischemic attack (TIA). J Stroke Cerebrovasc Dis. 2011; 20(4 Suppl):S31–73.
Article25. Miyai I, Sonoda S, Nagai S, Takayama Y, Inoue Y, Kakehi A, et al. Results of new policies for inpatient rehabilitation coverage in Japan. Neurorehabil Neural Repair. 2011; 25:540–7.
Article26. Linacre JM, Heinemann AW, Wright BD, Granger CV, Hamilton BB. The structure and stability of the Functional Independence Measure. Arch Phys Med Rehabil. 1994; 75:127–32.
Article27. Hamilton BB, Laughlin JA, Fiedler RC, Granger CV. Interrater reliability of the 7-level functional independence measure (FIM). Scand J Rehabil Med. 1994; 26:115–9.28. Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996; 77:1226–32.
Article29. Koyama T, Matsumoto K, Okuno T, Domen K. Relationships between independence level of single motor-FIM items and FIM-motor scores in patients with hemiplegia after stroke: an ordinal logistic modelling study. J Rehabil Med. 2006; 38:280–6.
Article30. Kwon S, Hartzema AG, Duncan PW, Min-Lai S. Disability measures in stroke: relationship among the Barthel Index, the Functional Independence Measure, and the Modified Rankin Scale. Stroke. 2004; 35:918–23.31. Organisation for Economic Co-operation and Development. OECD data: length of hospital stay [Internet]. Paris, France: Organisation for Economic Co-operation and Development;c2021. [cited 2021 May 18]. Available from: https://data.oecd.org/healthcare/length-of-hospital-stay.htm.32. Ministry of Health, Labour and Welfare. Annual Health, Labour and Welfare Report 2016: health and medical services [Internet]. Tokyo, Japan: Ministry of Health, Labour and Welfare;c2021. [cited 2021 May 18]. Available from: https://www.mhlw.go.jp/english/wp/wp-hw10/dl/02e.pdf.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Application of Artificial Intelligence in Acute Ischemic Stroke: A Scoping Review
- The Association between Neurological Prognosis and Serum Glucose Level by Stroke Subtype in Acute Ischemic Stroke
- D-dimer Predicts Short-Term Functional Outcome in Acute Ischemic Stroke
- Early In-hospital Management of Acute Ischemic Stroke
- Pneumococcal meningitis complicated by otomastoiditis and pneumocephalus confounding an acute ischemic stroke diagnosis