J Korean Assoc Oral Maxillofac Surg.
2021 Jun;47(3):209-215. 10.5125/jkaoms.2021.47.3.209.
Functional outcomes in children with reduction glossectomy for vascular malformations – “less is more!”
- Affiliations
-
- 1Departments of Paediatric Surgery, Christian Medical College, Vellore, India
- 2Departments of Pathology, Christian Medical College, Vellore, India
- KMID: 2517271
- DOI: http://doi.org/10.5125/jkaoms.2021.47.3.209
Abstract
Objectives
Vascular malformation (VM) of the tongue can cause true macroglossia in children. Reduction glossectomy provides primary relief when sclerotherapy has failed or is not possible. In this study, we evaluated the surgical role in functional outcome of reduction glossectomy performed for VM of the tongue.
Patients and Methods
We evaluated the functional and surgical outcomes of seven children who were treated at a tertiary care centre in Southern India between 2013 and 2018.
Results
Six children underwent median glossectomy, while one child underwent lateral glossectomy. Functional assessment was performed at least 2 years after the date of surgery. At the time of assessment, speech was comprehensible for three children and was occasionally unintelligible in four children. Taste and swallowing were normal in all seven children. Six children exhibited a minimal residual lesion after surgery, of which only one was symptomatic. Residual lesions were managed with sclerotherapy (n=3), observation (n=2), or repeat surgery (n=1).
Conclusion
Reduction glossectomy in children with macroglossia secondary to VMs has acceptable outcomes in terms of cosmesis and speech, with no gastronomic restriction.
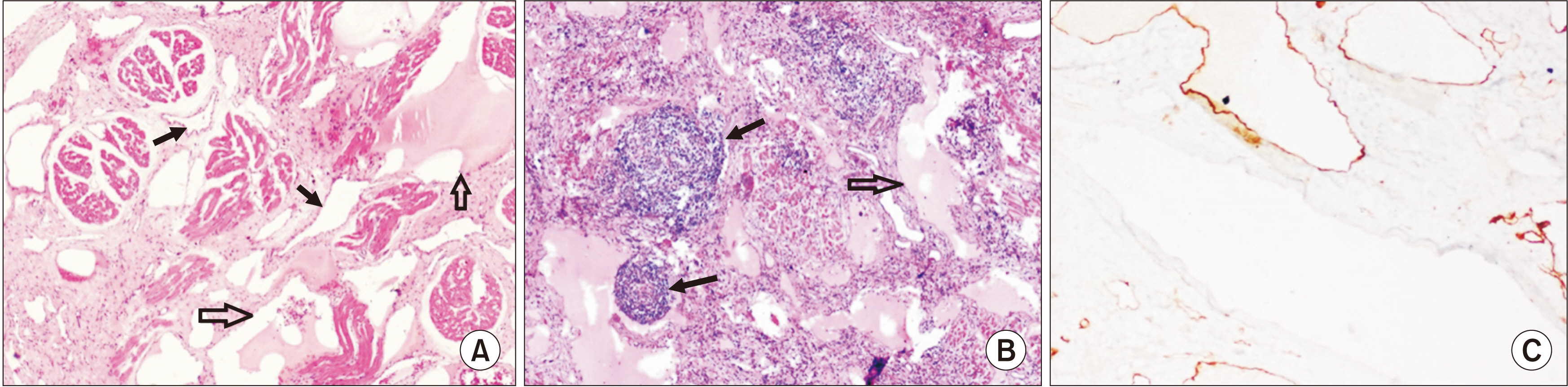
Figure
Reference
-
References
1. Balaji SM. 2013; Reduction glossectomy for large tongues. Ann Maxillofac Surg. 3:167–72. https://doi.org/10.4103/2231-0746.119230. DOI: 10.4103/2231-0746.119230. PMID: 24205477. PMCID: PMC3814666.
Article2. Walker WA, Goulet O, Kleinman RE, Sherman PM, Schneider BL, Sanderson IR. 2004. Pediatric gastrointestinal disease: pathophysiology, diagnosis, management. 4th ed. BC Decker;Hamilton: p. 1158.3. Myer CM 3rd, Hotaling AJ, Reilly JS. 1986; The diagnosis and treatment of macroglossia in children. Ear Nose Throat J. 65:444–8. PMID: 3536424.4. Vogel JE, Mulliken JB, Kaban LB. 1986; Macroglossia: a review of the condition and a new classification. Plast Reconstr Surg. 78:715–23. PMID: 2947254.5. Khadilkar V, Khadilkar AV, Kajale N. 2019; Indian growth references from 0-18-year-old children and adolescents - a comparison of two methods. Indian J Endocrinol Metab. 23:635–44. https://doi.org/10.4103/ijem.IJEM_555_19. DOI: 10.4103/ijem.IJEM_555_19. PMID: 32042700. PMCID: PMC6987783.
Article6. Henningsson G, Kuehn DP, Sell D, Sweeney T, Trost-Cardamone JE. Whitehill TL; Speech Parameters Group. 2008; Universal parameters for reporting speech outcomes in individuals with cleft palate. Cleft Palate Craniofac J. 45:1–17. https://doi.org/10.1597/06-086.1. DOI: 10.1597/06-086.1. PMID: 18215095.
Article7. Crary MA, Mann GD, Groher ME. 2005; Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 86:1516–20. https://doi.org/10.1016/j.apmr.2004.11.049. DOI: 10.1016/j.apmr.2004.11.049. PMID: 16084801.
Article8. Bell DJ, Gaillard F. 2020. ISSVA classification of vascular anomalies [Internet]. Radiopaedia;Kew: Available from: https://radiopaedia.org/articles/issva-classification-of-vascular-anomalies.9. Vlachou E, Dalal M, Monaghan A, Nishikawa H. 2005; Acute exacerbation of macroglossia. Br J Plast Surg. 58:877–80. https://doi.org/10.1016/j.bjps.2004.12.010. DOI: 10.1016/j.bjps.2004.12.010. PMID: 16086997.
Article10. Wiegand S, Eivazi B, Zimmermann AP, Neff A, Barth PJ, Sesterhenn AM, et al. 2009; Microcystic lymphatic malformations of the tongue: diagnosis, classification, and treatment. Arch Otolaryngol Head Neck Surg. 135:976–83. https://doi.org/10.1001/archoto.2009.131. DOI: 10.1001/archoto.2009.131. PMID: 19841334.
Article11. Lahiri A, Kok K, Sharp I, Nishikawa H. 2006; Acute exacerbation of macroglossia leading to necrosis of the anterior third of the tongue. J Plast Reconstr Aesthet Surg. 59:871–3. https://doi.org/10.1016/j.bjps.2005.12.005. DOI: 10.1016/j.bjps.2005.12.005. PMID: 16876088.
Article12. Adams DM, Trenor CC 3rd, Hammill AM, Vinks AA, Patel MN, Chaudry G, et al. 2016; Efficacy and safety of sirolimus in the treatment of complicated vascular anomalies. Pediatrics. 137:e20153257. DOI: 10.1542/peds.2015-3257. PMID: 26783326. PMCID: PMC4732362.
Article13. Curry S, Logeman A, Jones D. 2019; Sirolimus: a successful medical treatment for head and neck lymphatic malformations. Case Rep Otolaryngol. 2019:2076798. https://doi.org/10.1155/2019/2076798. DOI: 10.1155/2019/2076798. PMID: 31019827. PMCID: PMC6451791.
Article14. Hammer J, Seront E, Duez S, Dupont S, Van Damme A, Schmitz S, et al. 2018; Sirolimus is efficacious in treatment for extensive and/or complex slow-flow vascular malformations: a monocentric prospective phase II study. Orphanet J Rare Dis. 13:191. https://doi.org/10.1186/s13023-018-0934-z. DOI: 10.1186/s13023-018-0934-z. PMID: 30373605. PMCID: PMC6206885.
Article15. Lee BB. 2020; Sirolimus in the treatment of vascular anomalies. J Vasc Surg. 71:328. https://doi.org/10.1016/j.jvs.2019.08.246. DOI: 10.1016/j.jvs.2019.06.217. PMID: 31676179.
Article16. Morgan WE, Friedman EM, Duncan NO, Sulek M. 1996; Surgical management of macroglossia in children. Arch Otolaryngol Head Neck Surg. 122:326–9. DOI: 10.1001/archotol.1996.01890150096017. PMID: 8607962.
Article17. Myers EN. 2008. Operative otolaryngology: head and neck surgery. 2nd ed. Elsevier;Philadelphia (PA): p. 161–7.18. Davalbhakta A, Lamberty BG. 2000; Technique for uniform reduction of macroglossia. Br J Plast Surg. 53:294–7. https://doi.org/10.1054/bjps.1999.3311. DOI: 10.1054/bjps.1999.3311. PMID: 10876252.
Article19. Melville JC, Menegotto KD, Woernley TC, Maida BD, Alava I 3rd. 2018; Unusual case of a massive macroglossia secondary to myxedema: a case report and literature review. J Oral Maxillofac Surg. 76:119–27. https://doi.org/10.1016/j.joms.2017.06.033. DOI: 10.1016/j.joms.2017.06.033. PMID: 28742994.
Article20. Chung IH, Song SI, Kim ES. 2003; Central tongue reduction for macroglossia. J Korean Assoc Oral Maxillofac Surg. 29:191–4. DOI: 10.1097/00006534-199305000-00031. PMID: 8479986.21. Köle H. 1965; Results, experience, and problems in the operative treatment of anomalies with reverse overbite (mandibular protrusion). Oral Surg Oral Med Oral Pathol. 19:427–50. https://doi.org/10.1016/0030-4220(65)90002-2. DOI: 10.1016/0030-4220(65)90002-2.
Article22. Dzioba A, Aalto D, Papadopoulos-Nydam G, Seikaly H, Rieger J, Wolfaardt J, et al. 2017; ; Head and Neck Research Network. Functional and quality of life outcomes after partial glossectomy: a multi-institutional longitudinal study of the head and neck research network. J Otolaryngol Head Neck Surg. 46:56. https://doi.org/10.1186/s40463-017-0234-y. DOI: 10.1186/s40463-017-0234-y.
Article23. Halczy-Kowalik L, Wiktor A, Rzewuska A, Kowalczyk R, Wysocki R, Posio V. 2015; Compensatory mechanisms in patients after a partial or total glossectomy due to oral cancer. Dysphagia. 30:738–50. https://doi.org/10.1007/s00455-015-9652-z. DOI: 10.1007/s00455-015-9652-z. PMID: 26487064.
Article24. Hall JE. 2012. Pocket companion to Guyton and Hall textbook of medical physiology. 12th ed. Saunders/Elsevier;Philadelphia (PA): p. 1091.25. Barrett KE, Barman SM, Boitano S, Brooks H. 2012. Ganong's review of medical physiology. 24th ed. McGraw-Hill;New York: p. 764.26. Elhalaby EE, Hassan HS, Almetaher HA. 2015; Reduction glossectomy for macroglossia in children. Ann Pediatr Surg. 11:115–9. https://doi.org/10.1097/01.XPS.0000462929.45595.1a. DOI: 10.1097/01.XPS.0000462929.45595.1a.
Article27. Bjuggren G, Jensen R, Strömbeck JO. 1968; Macroglossia and its surgical treatment. Indications and postoperative experiences from the orthodontic, phoniatric, and surgical points of view. Scand J Plast Reconstr Surg. 2:116–24. https://doi.org/10.3109/02844316809010493. DOI: 10.3109/02844316809010493. PMID: 5733935.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Glossectomy in the severe maxillofacial vascular malformation with jaw deformity: a rare case report
- Central tongue reduction for macroglossia
- A Review of the Current State and Future Directions for Management of Scalp and Facial Vascular Malformations
- Reduction glossectomy of congenital macroglossia due to lymphangioma
- An experimental study on the mandibular growth by the partial glossectomy of the rats