J Korean Med Sci.
2021 Jun;36(25):e172. 10.3346/jkms.2021.36.e172.
The Prevalence and Emergency Department Utilization of Patients Who Underwent Single and Double Inter-hospital Transfers in the Emergency Department: a Nationwide Population-based Study in Korea, 2016–2018
- Affiliations
-
- 1Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Emergency Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 3Department of Emergency Medicine, Dong-A University College of Medicine, Busan, Korea
- 4Department of Emergency Medicine, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 5National Emergency Medical Center, National Medical Center, Seoul, Korea
- 6Department of Emergency Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- KMID: 2516988
- DOI: http://doi.org/10.3346/jkms.2021.36.e172
Abstract
- Background
Inter-hospital transfer (IHT) for emergency department (ED) admission is a burden to high-level EDs. This study aimed to evaluate the prevalence and ED utilization patterns of patients who underwent single and double IHTs at high-level EDs in South Korea.
Methods
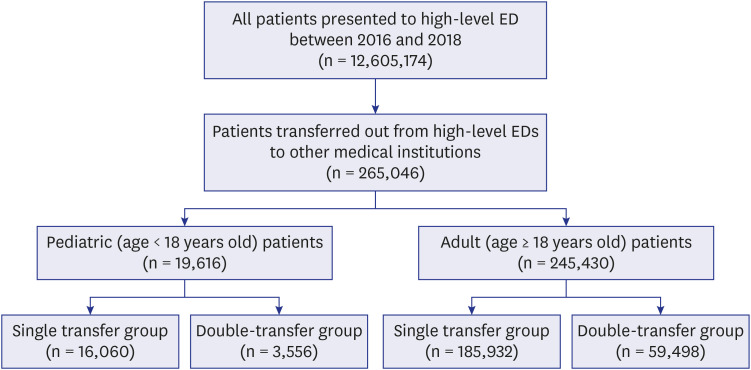
This nationwide cross-sectional study analyzed data from the National Emergency Department Information System for the period of 2016–2018. All the patients who underwent IHT at Level I and II emergency centers during this time period were included. The patients were categorized into the single-transfer and double-transfer groups. The clinical characteristics and ED utilization patterns were compared between the two groups.
Results
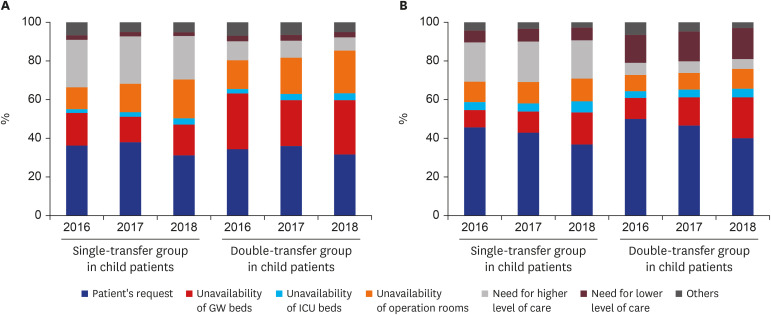
We found that 2.1% of the patients in the ED (n = 265,046) underwent IHTs; 18.1% of the pediatric patients (n = 3,556), and 24.2% of the adult patients (n = 59,498) underwent double transfers. Both pediatric (median, 141.0 vs. 208.0 minutes, P < 0.001) and adult (median, 189.0 vs. 308.0 minutes, P < 0.001) patients in the double-transfer group had longer duration of stay in the EDs. Patient's request was the reason for transfer in 41.9% of all IHTs (111,076 of 265,046). Unavailability of medical resources was the reason for transfer in 30.0% of the double transfers (18,920 of 64,054).
Conclusion
The incidence of double-transfer of patients is increasing. The main reasons for double transfers were patient's request and unavailability of medical resources at the firsttransfer hospitals. Emergency physicians and policymakers should focus on lowering the number of preventable double transfers.
Figure
Reference
-
1. Siegel B. The emergency department: rethinking the safety net for the safety net. Health Aff (Millwood). 2004; 23(Suppl Web Exclusives):W4-146–8.
Article2. Mueller SK, Zheng J, Orav EJ, Schnipper JL. Rates, predictors and variability of interhospital transfers: a national evaluation. J Hosp Med. 2017; 12(6):435–442. PMID: 28574533.
Article3. Mohr NM, Wessman BT, Bassin B, Elie-Turenne MC, Ellender T, Emlet LL, et al. Boarding of critically ill patients in the emergency department. Crit Care Med. 2020; 48(8):1180–1187. PMID: 32697489.
Article4. Kindermann DR, Mutter RL, Cartwright-Smith L, Rosenbaum S, Pines JM. Admit or transfer? The role of insurance in high-transfer-rate medical conditions in the emergency department. Ann Emerg Med. 2014; 63(5):561–571.e8. PMID: 24342815.
Article5. Cassan S, Rata M, Vallenet C, Fromage P, Champly F, Broin P, et al. Early inter-hospital transfer of patients with myocardial infarction without a doctor, paramedic or nurse on board: results from a French regional emergency care network. BMC Emerg Med. 2019; 19(1):60. PMID: 31660873.
Article6. Iwashyna TJ, Kahn JM, Hayward RA, Nallamothu BK. Interhospital transfers among Medicare beneficiaries admitted for acute myocardial infarction at nonrevascularization hospitals. Circ Cardiovasc Qual Outcomes. 2010; 3(5):468–475. PMID: 20682917.
Article7. Hernandez-Boussard T, Davies S, McDonald K, Wang NE. Interhospital facility transfers in the United States: a nationwide outcomes study. J Patient Saf. 2017; 13(4):187–191. PMID: 25397857.
Article8. Mueller S, Zheng J, Orav EJ, Schnipper JL. Inter-hospital transfer and patient outcomes: a retrospective cohort study. BMJ Qual Saf. 2019; 28(11):e1.
Article9. Fan R, Zhao M, Peng X. Differentiating inter-hospital transfer types: varied impacts on LOS and destination choices. Acad Manag Proc. 2019; 2019.
Article10. Bosk EA, Veinot T, Iwashyna TJ. Which patients and where: a qualitative study of patient transfers from community hospitals. Med Care. 2011; 49(6):592–598. PMID: 21430581.11. Mohr NM, Harland KK, Shane DM, Ahmed A, Fuller BM, Torner JC. Inter-hospital transfer is associated with increased mortality and costs in severe sepsis and septic shock: an instrumental variables approach. J Crit Care. 2016; 36:187–194. PMID: 27546770.
Article12. Golestanian E, Scruggs JE, Gangnon RE, Mak RP, Wood KE. Effect of interhospital transfer on resource utilization and outcomes at a tertiary care referral center. Crit Care Med. 2007; 35(6):1470–1476. PMID: 17440423.
Article13. Sokol-Hessner L, White AA, Davis KF, Herzig SJ, Hohmann SF. Interhospital transfer patients discharged by academic hospitalists and general internists: Characteristics and outcomes. J Hosp Med. 2016; 11(4):245–250. PMID: 26588825.
Article14. National Emergency Medical Center (KR). Statistical yearbook of emergency medical service, 2019. Updated 2019. Accessed December 10, 2020. https://www.e-gen.or.kr/nemc/statistics_annual_report.do.15. Khang YH, Lee SI. Health inequalities policy in Korea: current status and future challenges. J Korean Med Sci. 2012; 27(Suppl):S33–40. PMID: 22661869.
Article16. Statistics Korea. Korean Standard Classification of Diseases, 7th Revision (KCD-7). Updated 2020. Accessed December 10, 2020. http://kssc.kostat.go.kr/ksscNew_web/kssc/common/selectIntroduce.do?gubun=2&bbsId=kcd_ug#.17. Kim YJ, Seo DW, Kim WY. Types of cancer and outcomes in patients with cancer requiring admission from the emergency department: a nationwide, population-based study, 2016-2017. Cancer. Forthcoming. 2021; DOI: 10.1002/cncr.33534.
Article18. Park J, Choi H, Kang B, Kim C, Kang H, Lim T. A nationwide survey of Korean emergency department triage systems and scales; A first step towards reform of the emergency medical service system. J Korean Soc Emerg Med. 2014; 25(5):499–508.19. Nacht J, Macht M, Ginde AA. Interhospital transfers from U.S. emergency departments: implications for resource utilization, patient safety, and regionalization. Acad Emerg Med. 2013; 20(9):888–893. PMID: 24033705.
Article20. Arulraja MD, Swanson MB, Mohr NM. Double inter-hospital transfer in Sepsis patients presenting to the ED does not worsen mortality compared to single inter-hospital transfer. J Crit Care. 2020; 56:49–57. PMID: 31837601.
Article21. Mohr NM, Harland KK, Shane DM, Miller SL, Torner JC. Potentially avoidable pediatric interfacility transfer is a costly burden for rural families: a cohort study. Acad Emerg Med. 2016; 23(8):885–894. PMID: 27018337.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The pattern of emergency department utilization in pediatric patients who underwent interfacility transfers from the emergency department: a nationwide population-based study in South Korea, 2016-2018
- Survey of Emergency-Related Physicians on Inter-hospital Transfers via 1339 in Busan
- An analysis of HIV patients visiting hospitals in Korea by complete enumeration: based on the Health Insurance Review and Assessment Service database
- The impacts of the COVID-19 pandemic on emergency care utilization in patients with major emergency diseases in Chungnam Province
- Requests for Interhospital Transfer Received by An 1339 Emergency Medical Information Center