J Rheum Dis.
2021 Jul;28(3):165-170. 10.4078/jrd.2021.28.3.165.
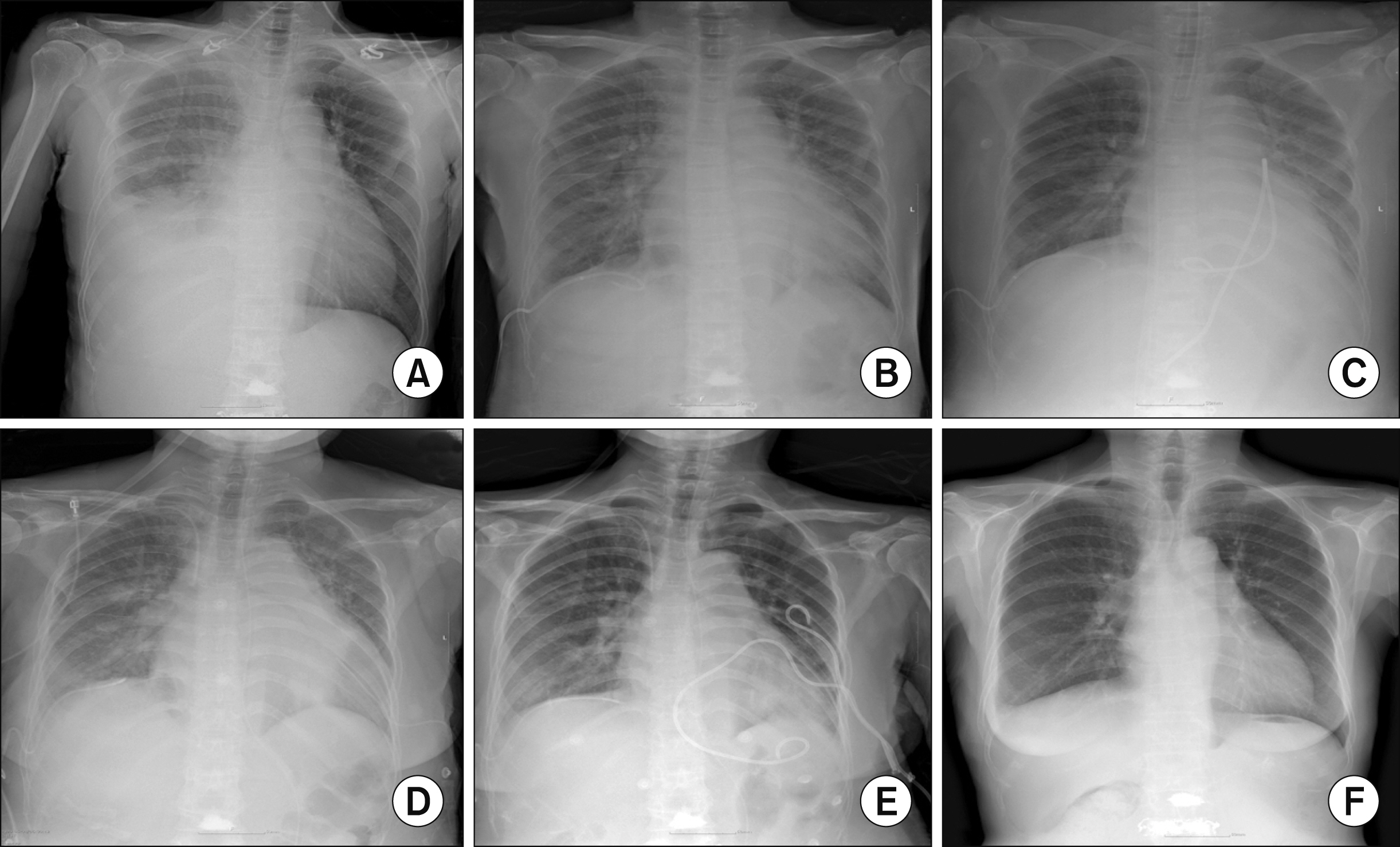
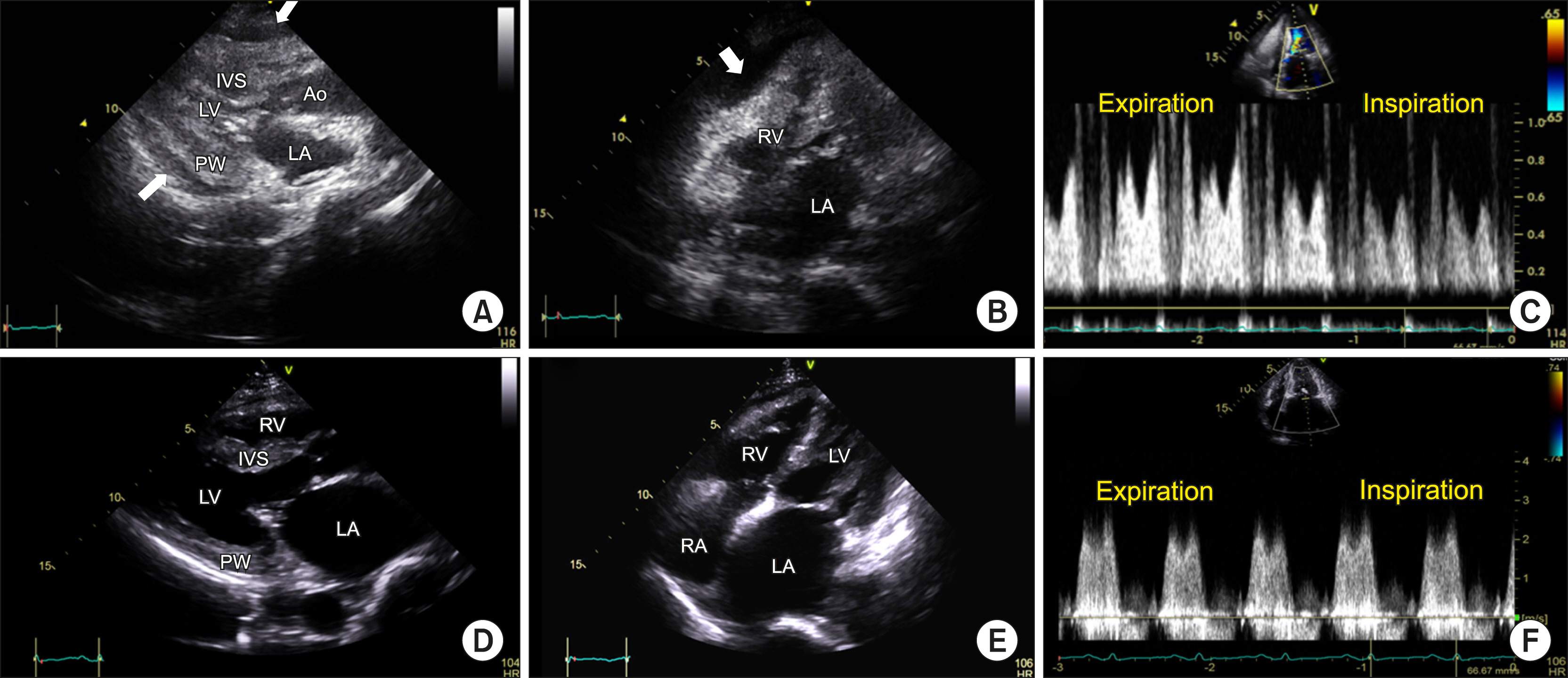
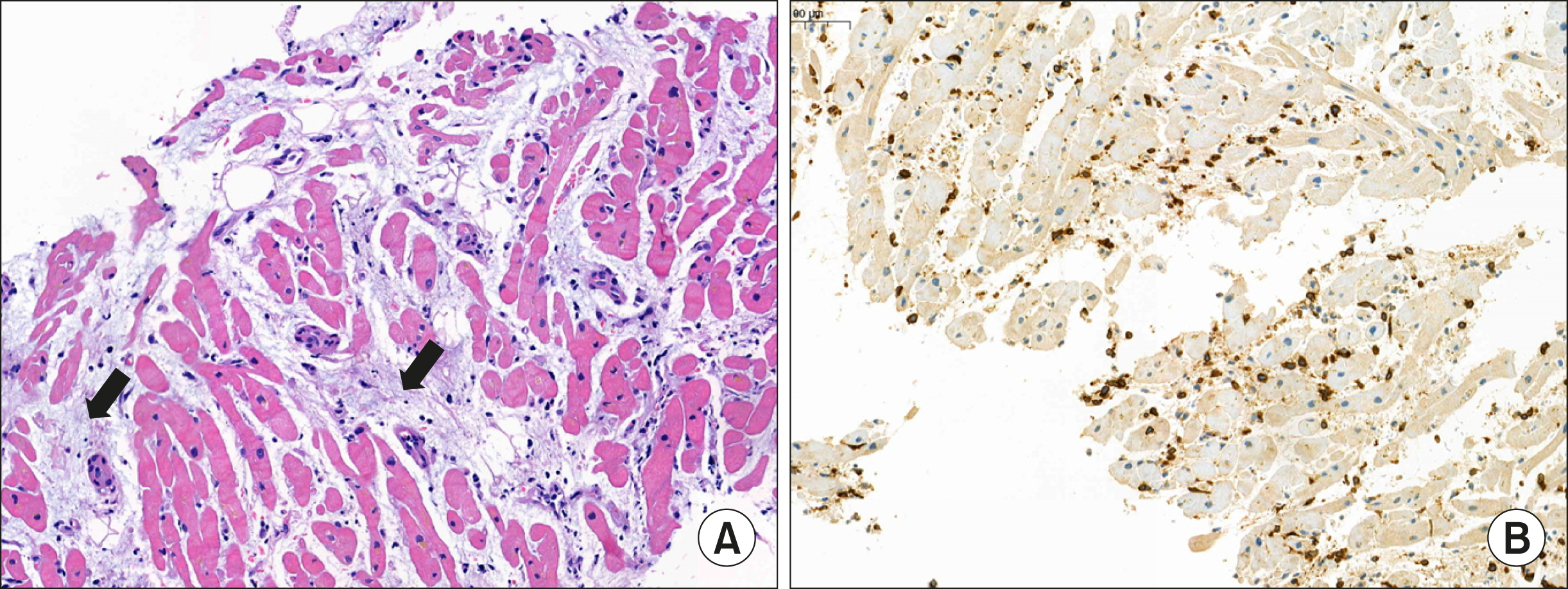
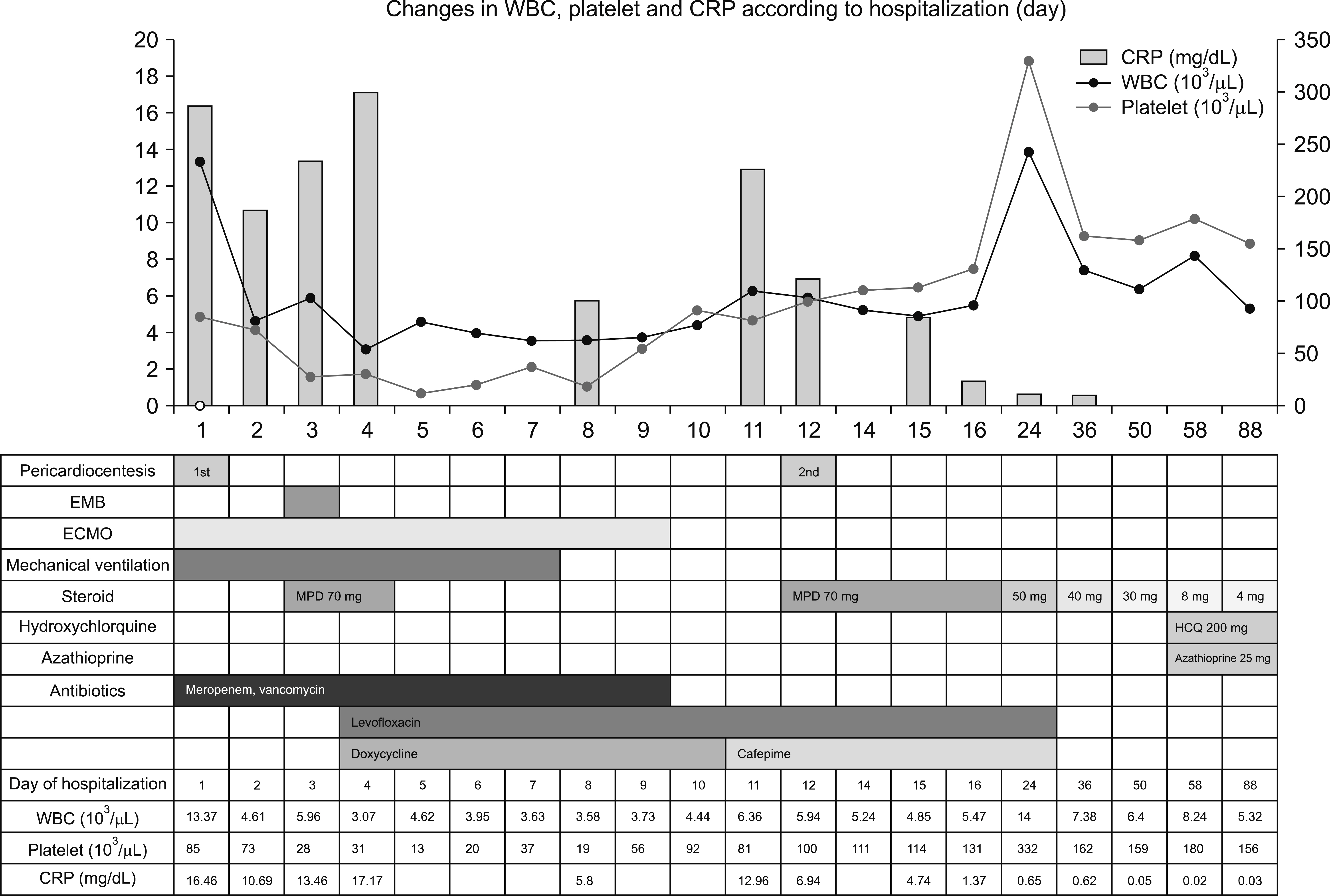
Fatal Myopericarditis in a Patient With Lupus Erythematosus Supported by Extracorporeal Membrane Oxygenation: A Case Report
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine and Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- 2Division of Rheumatology, Department of Internal Medicine, Daedong Hosipital, Busan, Korea
- 3Department of Pathology, Pusan National University Yangsan Hospital, Yangsan, Korea
- 4Division of Pulmonology, Allergy and Critical Care Medicine, Department of Internal Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea
- 5Division of Infectious Disease, Department of Internal Medicine, Pusan National University Yangsan Hospital, Yangsan, Korea
- KMID: 2516953
- DOI: http://doi.org/10.4078/jrd.2021.28.3.165
Abstract
- Systemic lupus erythematosus (SLE) may occur in any organ. In patients with SLE, myocarditis is extremely rare and potentially life-threatening. Herein, we report on a patient with lupus myocarditis, diagnosed by myocardial biopsy, immunologic tests, and clinical manifestations. Our findings suggest that securing time for diagnosis via extracorporeal membrane oxygenation and other intensive care is helpful for obtaining a good prognosis.
Figure
Reference
-
1. Chung JW, Joe DY, Park HJ, Kim HA, Park HS, Suh CH. 2008; Clinical characteristics of lupus myocarditis in Korea. Rheumatol Int. 28:275–80. DOI: 10.1007/s00296-007-0414-6. PMID: 17634899.
Article2. Chaudhari D, Madani MA, Balbissi Md KA, Paul TK. 2015; Lupus myocarditis presenting as life-threatening overt heart failure: a case report with review of cardiovascular manifestations of systemic lupus erythematosus. J La State Med Soc. 167:220–2. PMID: 27159597.3. Mohanty B, Sunder A. 2020; Lupus myocarditis-a rare case. J Family Med Prim Care. 9:4441–3. DOI: 10.4103/jfmpc.jfmpc_716_20. PMID: 33110880. PMCID: PMC7586557.
Article4. Wijetunga M, Rockson S. 2002; Myocarditis in systemic lupus erythematosus. Am J Med. 113:419–23. DOI: 10.1016/S0002-9343(02)01223-8. PMID: 12401537.
Article5. Doria A, Iaccarino L, Sarzi-Puttini P, Atzeni F, Turriel M, Petri M. 2005; Cardiac involvement in systemic lupus erythematosus. Lupus. 14:683–6. DOI: 10.1191/0961203305lu2200oa. PMID: 16218467.
Article6. Thomas G, Cohen Aubart F, Chiche L, Haroche J, Hié M, Hervier B, et al. 2017; Lupus myocarditis: initial presentation and longterm outcomes in a multicentric series of 29 patients. J Rheumatol. 44:24–32. DOI: 10.3899/jrheum.160493. PMID: 28042125.
Article7. Miner JJ, Kim AH. 2014; Cardiac manifestations of systemic lupus erythematosus. Rheum Dis Clin North Am. 40:51–60. DOI: 10.1016/j.rdc.2013.10.003. PMID: 24268009.
Article8. Gartshteyn Y, Tamargo M, Fleischer S, Kapoor T, Li J, Askanase A, et al. 2020; Endomyocardial biopsies in the diagnosis of myocardial involvement in systemic lupus erythematosus. Lupus. 29:199–204. DOI: 10.1177/0961203319897116. PMID: 31924147. PMCID: PMC7261237.
Article9. Kociol RD, Cooper LT, Fang JC, Moslehi JJ, Pang PS, Sabe MA, et al. 2020; Recognition and initial management of fulminant myocarditis: a scientific statement from the American Heart Association. Circulation. 141:e69–92. DOI: 10.1161/CIR.0000000000000745. PMID: 31902242.
Article10. Barrie M, McKnight L, Solanki P. 2012; Rapid resolution of acute fulminant myocarditis after IVIG and steroid treatment. Case Rep Crit Care. 2012:262815. DOI: 10.1155/2012/262815. PMID: 24826334. PMCID: PMC4010038.
Article11. Saito T, Katayama H, Kodani E. 2019; Is steroid therapy really banned for lymphocytic myocarditis before excluding viral infection? Eur Heart J. 40:1014–5. DOI: 10.1093/eurheartj/ehy738. PMID: 30403793.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Successful Use of Extracorporeal Membrane Oxygenation in Diffuse Alveolar Hemorrhage Secondary to Systemic Lupus Erythematosus
- Anesthetic management of cesarean delivery of parturient with systemic lupus erythematosus associated with pulmonary arterial hypertension - A case report -
- Myopericarditis in a Korean Young Male With Systemic Lupus Erythematosus
- Blood Transfusion Strategies in Patients Supported by Extracorporeal Membrane Oxygenation
- A case of rescuing a patient with acute cardiovascular instability from sudden and massive intraoperative pulmonary thromboembolism by extracorporeal membrane oxygenation