J Rheum Dis.
2021 Jul;28(3):150-158. 10.4078/jrd.2021.28.3.150.
Clinical and Genetic Risk Factors Associated With the Presence of Lupus Nephritis
- Affiliations
-
- 1Department of Rheumatology, Hanyang University Hospital for Rheumatic Diseases, Seoul, Korea
- 2Department of Rheumatology, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 3Hanyang University Institute for Rheumatology Research, Seoul, Korea
- 4Division of Rheumatology, Department of Internal Medicine, Korea University Guro Hospital, Seoul, Korea
- 5Department of Big Data Application, College of Social Economic & Interdisciplinary Studies, Hannam University, Daejeon, Korea
- 6Departments of Life and Nanopharmaceutical Sciences, Kyung Hee University, Seoul, Korea
- 7Departments of Biology, Kyung Hee University, Seoul, Korea
- KMID: 2516951
- DOI: http://doi.org/10.4078/jrd.2021.28.3.150
Abstract
Objective
To elucidate whether clinical features and the weighted genetic risk score (wGRS) were associated with the presence of lupus nephritis (LN).
Methods
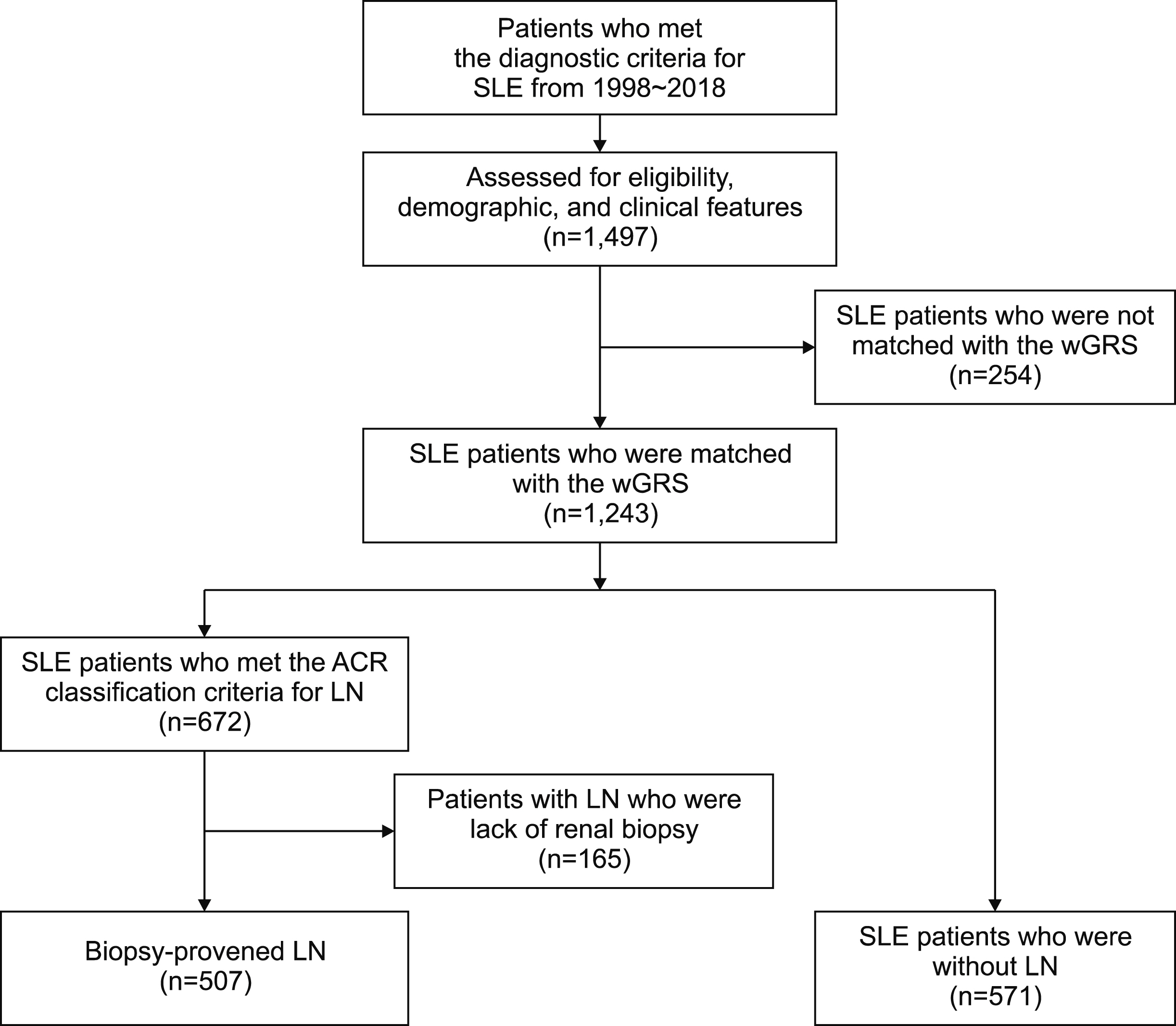
We retrospectively divided patients with systemic lupus erythematosus (SLE, n=1,078) into biopsy-proven LN (n=507) and non-LN groups (non-LN, n=571). Baseline clinical features, serologic markers, and the wGRS were collected. The wGRS was calculated from 112 non-human leukocyte antigen (non-HLA) loci and HLA-DRβ1 amino acid haplotypes for SLE. Associations among clinical features, wGRS, and the presence of LN were identified.
Results
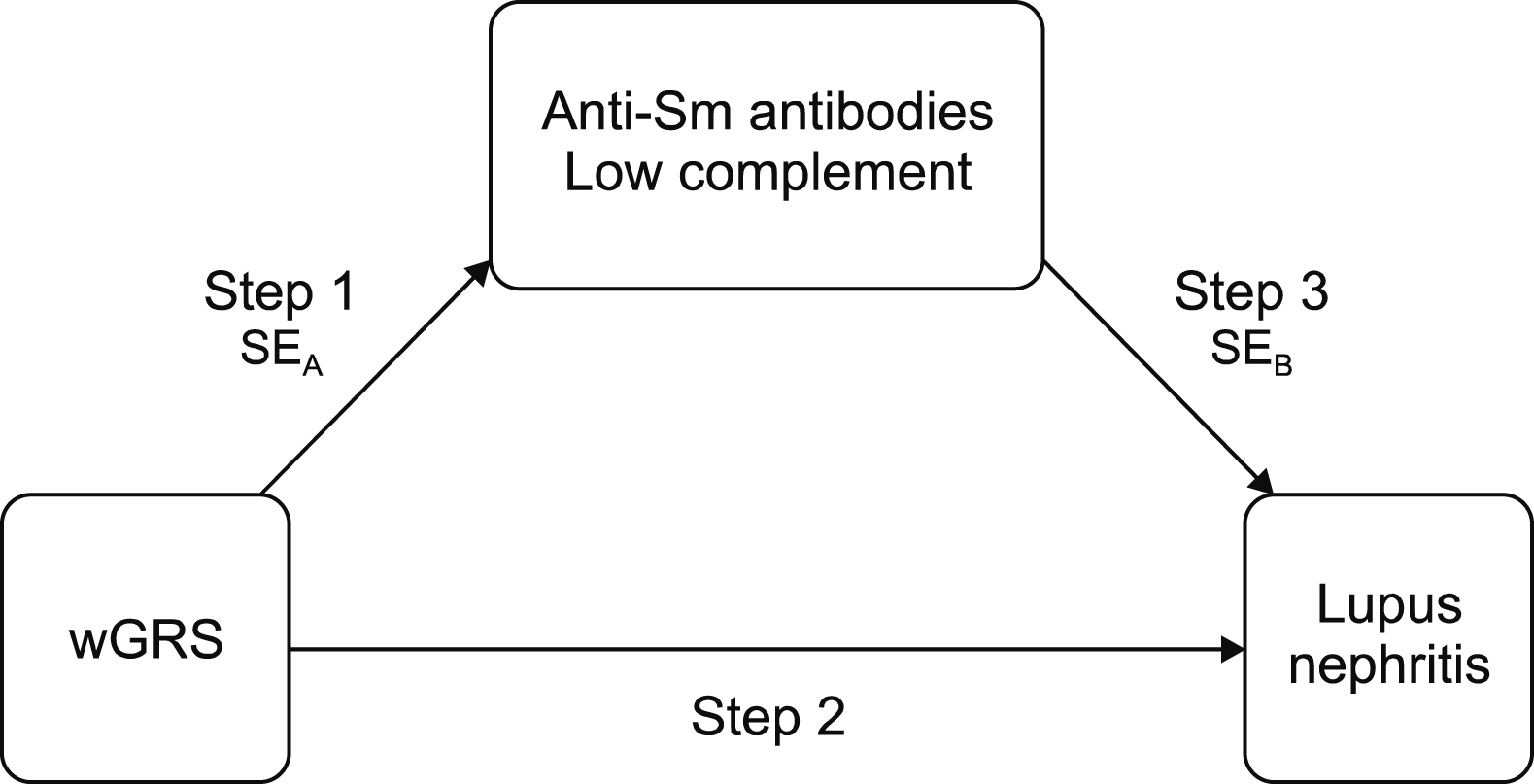
In the multivariate analysis, patients with LN were younger at diagnosis (odds ratio [OR]=0.97, p<0.001), had more pleuritis (OR=2.44, p<0.001) and pericarditis (OR=1.62, p=0.029), had a higher detection rate of anti-double stranded deoxyribonucleic acid (anti-dsDNA antibodies, OR=2.22, p<0.001), anti-Smith antibodies (anti-Sm antibodies, OR=1.70, p=0.002), low level of complement (OR=1.37, p=0.043) and absence of antiphospholipid antibodies (aPL antibodies, OR=1.60, p=0.002), and had higher wGRS (OR=1.16, p=0.012). Mediation analysis suggested that anti-Sm antibodies and low complement could be mediators in the relationship between high wGRS and the presence of LN.
Conclusion
Onset age, pleuritis, pericarditis, several serologic markers, and wGRS were associated with the presence of LN. Anti-Sm antibodies and low complement appeared to mediate the indirect relationship between wGRS and the presence of LN.
Figure
Cited by 1 articles
-
Delineating the Risk of Lupus Nephritis: How Far Have We Come?
Jisoo Lee
J Rheum Dis. 2021;28(4):173-175. doi: 10.4078/jrd.2021.28.4.173.
Reference
-
1. Tsokos GC. 2011; Systemic lupus erythematosus. N Engl J Med. 365:2110–21. DOI: 10.1056/NEJMra1100359. PMID: 22129255.
Article2. Formiga F, Moga I, Pac M, Mitjavila F, Rivera A, Pujol R. 1999; Mild presentation of systemic lupus erythematosus in elderly patients assessed by SLEDAI. SLE Disease Activity Index. Lupus. 8:462–5. DOI: 10.1177/096120339900800609. PMID: 10483015.3. Hanly JG, O'Keeffe AG, Su L, Urowitz MB, Romero-Diaz J, Gordon C, et al. 2016; The frequency and outcome of lupus nephritis: results from an international inception cohort study. Rheumatology (Oxford). 55:252–62. DOI: 10.1093/rheumatology/kev311. PMID: 26342222. PMCID: PMC4939728.4. Fiehn C, Hajjar Y, Mueller K, Waldherr R, Ho AD, Andrassy K. 2003; Improved clinical outcome of lupus nephritis during the past decade: importance of early diagnosis and treatment. Ann Rheum Dis. 62:435–9. DOI: 10.1136/ard.62.5.435. PMID: 12695156. PMCID: PMC1754523.
Article5. Ntatsaki E, Isenberg D. 2015; Risk factors for renal disease in systemic lupus erythematosus and their clinical implications. Expert Rev Clin Immunol. 11:837–48. DOI: 10.1586/1744666X.2015.1045418. PMID: 25973642.
Article6. Mavragani CP, Fragoulis GE, Somarakis G, Drosos A, Tzioufas AG, Moutsopoulos HM. 2015; Clinical and laboratory predictors of distinct histopathogical features of lupus nephritis. Medicine (Baltimore). 94:e829. DOI: 10.1097/MD.0000000000000829. PMID: 26020385. PMCID: PMC4616414.
Article7. Alba P, Bento L, Cuadrado MJ, Karim Y, Tungekar MF, Abbs I, et al. 2003; Anti-dsDNA, anti-Sm antibodies, and the lupus anticoagulant: significant factors associated with lupus nephritis. Ann Rheum Dis. 62:556–60. DOI: 10.1136/ard.62.6.556. PMID: 12759294. PMCID: PMC1754557.
Article8. Reid S, Alexsson A, Frodlund M, Morris D, Sandling JK, Bolin K, et al. 2020; High genetic risk score is associated with early disease onset, damage accrual and decreased survival in systemic lupus erythematosus. Ann Rheum Dis. 79:363–9. DOI: 10.1136/annrheumdis-2019-216227. PMID: 31826855. PMCID: PMC7034364.
Article9. Chen LY, Shi ZR, Tan GZ, Han YF, Tang ZQ, Wang L. 2018; Systemic lupus erythematosus with and without a family history: a meta-analysis. Lupus. 27:716–21. DOI: 10.1177/0961203317739133. PMID: 29087262.
Article10. Kwon YC, Chun S, Kim K, Mak A. 2019; Update on the genetics of systemic lupus erythematosus: genome-wide association studies and beyond. Cells. 8:1180. DOI: 10.3390/cells8101180. PMID: 31575058. PMCID: PMC6829439.
Article11. Yin X, Kim K, Suetsugu H, Bang SY, Wen L, Koido M, et al. 2020; Meta-analysis of 208370 East Asians identifies 113 susceptibility loci for systemic lupus erythematosus. Ann Rheum Dis. 80:632–40. DOI: 10.1136/annrheumdis-2020-219209. PMID: 33272962. PMCID: PMC8053352.12. Igo RP Jr, Kinzy TG, Cooke Bailey JN. 2019; Genetic risk scores. Curr Protoc Hum Genet. 104:e95. DOI: 10.1002/cphg.95. PMID: 31765077. PMCID: PMC6941594.
Article13. Dudbridge F. 2013; Power and predictive accuracy of polygenic risk scores. PLoS Genet. 9:e1003348. DOI: 10.1371/journal.pgen.1003348. PMID: 23555274. PMCID: PMC3605113.
Article14. Tan EM, Cohen AS, Fries JF, Masi AT, McShane DJ, Rothfield NF, et al. 1982; The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 25:1271–7. DOI: 10.1002/art.1780251101. PMID: 7138600.
Article15. Joo YB, Park SY, Won S, Bae SC. 2016; Differences in clinical features and mortality between childhood-onset and adult-onset systemic lupus erythematosus: a prospective single-center study. J Rheumatol. 43:1490–7. DOI: 10.3899/jrheum.151129. PMID: 27252431.
Article16. Hochberg MC. 1997; Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 40:1725. DOI: 10.1002/art.1780400928. PMID: 9324032.
Article17. Gladman DD, Ibañez D, Urowitz MB. 2002; Systemic lupus erythematosus disease activity index 2000. J Rheumatol. 29:288–91. PMID: 11838846.18. Gladman D, Ginzler E, Goldsmith C, Fortin P, Liang M, Urowitz M, et al. 1996; The development and initial validation of the Systemic Lupus International Collaborating Clinics/American College of Rheumatology damage index for systemic lupus erythematosus. Arthritis Rheum. 39:363–9. DOI: 10.1002/art.1780390303. PMID: 8607884.
Article19. Hill GS, Delahousse M, Nochy D, Rémy P, Mignon F, Méry JP, et al. 2001; Predictive power of the second renal biopsy in lupus nephritis: significance of macrophages. Kidney Int. 59:304–16. DOI: 10.1046/j.1523-1755.2001.00492.x. PMID: 11135084.
Article20. Weening JJ, D'Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, et al. 2004; The classification of glomerulonephritis in systemic lupus erythematosus revisited. Kidney Int. 65:521–30. DOI: 10.1111/j.1523-1755.2004.00443.x. PMID: 14717922.
Article21. Austin HA 3rd, Muenz LR, Joyce KM, Antonovych TA, Kullick ME, Klippel JH, et al. 1983; Prognostic factors in lupus nephritis. Contribution of renal histologic data. Am J Med. 75:382–91. DOI: 10.1016/0002-9343(83)90338-8. PMID: 6351607.22. Hill GS, Delahousse M, Nochy D, Tomkiewicz E, Rémy P, Mignon F, et al. 2000; A new morphologic index for the evaluation of renal biopsies in lupus nephritis. Kidney Int. 58:1160–73. DOI: 10.1046/j.1523-1755.2000.00272.x. PMID: 10972679.
Article23. Kim K, Bang SY, Lee HS, Okada Y, Han B, Saw WY, et al. 2014; The HLA-DRβ1 amino acid positions 11-13-26 explain the majority of SLE-MHC associations. Nat Commun. 5:5902. DOI: 10.1038/ncomms6902. PMID: 25533202.
Article24. MacKinnon DP, Fairchild AJ, Fritz MS. 2007; Mediation analysis. Annu Rev Psychol. 58:593–614. DOI: 10.1146/annurev.psych.58.110405.085542. PMID: 16968208. PMCID: PMC2819368.
Article25. Kroon FPB, Veenbrink AI, de Mutsert R, Visser AW, van Dijk KW, le Cessie S, et al. 2019; The role of leptin and adiponectin as mediators in the relationship between adiposity and hand and knee osteoarthritis. Osteoarthritis Cartilage. 27:1761–7. DOI: 10.1016/j.joca.2019.08.003. PMID: 31450004.
Article26. He P, Fan SY, Guan JQ, Song WJ, Obore N, Chen WQ, et al. 2020; Mediation analysis for the relationship between dyslipidemia and coronary artery disease via hypersensitive C-reactive protein in a case-control study. Coron Artery Dis. 31:613–9. DOI: 10.1097/MCA.0000000000000911. PMID: 32452886.
Article27. Sobel ME. 1982; Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol. 13:290–312. DOI: 10.2307/270723.
Article28. Mok CC, Kwok RC, Yip PS. 2013; Effect of renal disease on the standardized mortality ratio and life expectancy of patients with systemic lupus erythematosus. Arthritis Rheum. 65:2154–60. DOI: 10.1002/art.38006. PMID: 23754671.
Article29. Reppe Moe SE, Molberg Ø, Strøm EH, Lerang K. 2019; Assessing the relative impact of lupus nephritis on mortality in a population-based systemic lupus erythematosus cohort. Lupus. 28:818–25. DOI: 10.1177/0961203319847275. PMID: 31072277.
Article30. Parodis I, Arnaud L, Gerhardsson J, Zickert A, Sundelin B, Malmström V, et al. 2016; Antiphospholipid antibodies in lupus nephritis. PLoS One. 11:e0158076. DOI: 10.1371/journal.pone.0158076. PMID: 27336701. PMCID: PMC4919007.
Article31. Varela DC, Quintana G, Somers EC, Rojas-Villarraga A, Espinosa G, Hincapie ME, et al. 2008; Delayed lupus nephritis. Ann Rheum Dis. 67:1044–6. DOI: 10.1136/ard.2008.088740. PMID: 18413438.
Article32. Mehrani T, Petri M. 2011; IgM anti-β2 glycoprotein I is protective against lupus nephritis and renal damage in systemic lupus erythematosus. J Rheumatol. 38:450–3. DOI: 10.3899/jrheum.100650. PMID: 21123325.33. Iwamoto T, Niewold TB. 2017; Genetics of human lupus nephritis. Clin Immunol. 185:32–9. DOI: 10.1016/j.clim.2016.09.012. PMID: 27693588. PMCID: PMC5373939.
Article34. Chen L, Wang YF, Liu L, Bielowka A, Ahmed R, Zhang H, et al. 2020; Genome-wide assessment of genetic risk for systemic lupus erythematosus and disease severity. Hum Mol Genet. 29:1745–56. DOI: 10.1093/hmg/ddaa030. PMID: 32077931. PMCID: PMC7322569.
Article35. Chowdhary VR, Dai C, Tilahun AY, Hanson JA, Smart MK, Grande JP, et al. 2015; A central role for HLA-DR3 in anti-Smith antibody responses and glomerulonephritis in a transgenic mouse model of spontaneous lupus. J Immunol. 195:4660–7. DOI: 10.4049/jimmunol.1501073. PMID: 26475924. PMCID: PMC5292932.
Article36. Kamitaki N, Sekar A, Handsaker RE, de Rivera H, Tooley K, Morris DL, et al. 2020; Complement genes contribute sex-biased vulnerability in diverse disorders. Nature. 582:577–81. DOI: 10.1038/s41586-020-2277-x. PMID: 32499649. PMCID: PMC7319891.
Article37. Reátegui-Sokolova C, Ugarte-Gil MF, Harvey GB, Wojdyla D, Pons-Estel GJ, Quintana R, et al. 2020; Predictors of renal damage in systemic lupus erythematous patients: data from a multiethnic, multinational Latin American lupus cohort (GLADEL). RMD Open. 6:e001299. DOI: 10.1136/rmdopen-2020-001299. PMID: 33310863. PMCID: PMC7859505.
Article38. Ahn SS, Yoo BW, Song JJ, Park YB, Lee SK, Lee SW. 2016; Anti-Sm is associated with the early poor outcome of lupus nephritis. Int J Rheum Dis. 19:897–902. DOI: 10.1111/1756-185X.12880. PMID: 27126359.
Article39. Mok CC, Ying KY, Tang S, Leung CY, Lee KW, Ng WL, et al. 2004; Predictors and outcome of renal flares after successful cyclophosphamide treatment for diffuse proliferative lupus glomerulonephritis. Arthritis Rheum. 50:2559–68. DOI: 10.1002/art.20364. PMID: 15334470.
Article40. Yung S, Chan TM. 2012; Autoantibodies and resident renal cells in the pathogenesis of lupus nephritis: getting to know the unknown. Clin Dev Immunol. 2012:139365. DOI: 10.1155/2012/139365. PMID: 22761629. PMCID: PMC3386553.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of Lupus Nephritis
- Clinical Outcome and Predictive Factors for Remission and Relapse of Proliferative Lupus Nephritis after Intravenous Cyclophosphamide Pulse Therapy
- Clinical study on lupus nephritis
- Survey Results on Diagnosis and Treatment of Lupus Nephritis
- A Clinical Study on Childhood Systemic Lupus Erythematosus