J Korean Med Sci.
2021 Jun;36(23):e159. 10.3346/jkms.2021.36.e159.
Descriptive Epidemiology and Survival Analysis of Acromegaly in Korea
- Affiliations
-
- 1Department of Endocrinology and Metabolism, Kyung Hee University College of Medicine, Seoul, Korea
- 2Department of Medicine, Graduate School of Medicine, Kyung Hee University, Seoul, Korea
- 3Department of Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
- KMID: 2516679
- DOI: http://doi.org/10.3346/jkms.2021.36.e159
Abstract
- Background
Acromegaly is a rare, slowly progressive disease. Its mechanism is not fully understood, and epidemiological research on Korean patients with acromegaly is scarce. The purpose of this study was to determine the incidence and prevalence of acromegaly and assess the comorbidities and survival benefits based on treatment options.
Methods
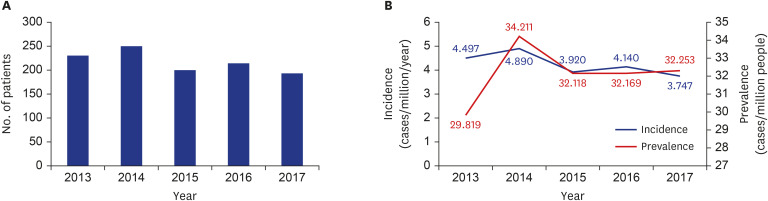
This nationwide population-based cohort study was conducted using data of the Korean Health Insurance Review and Assessment claims database to evaluate the incidence of newly diagnosed acromegaly cases during 2013–2017.
Results
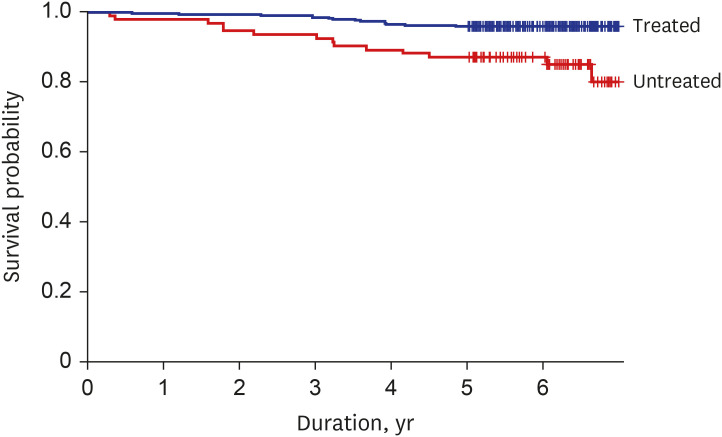
During the 5-year period, 1,093 patients were newly diagnosed with acromegaly. The average annual incidence was 4.2 cases per million per year, and the prevalence was 32.1 cases per million during this period. The incidence of hypertension was low after medical treatment (hazard ratio, 0.257; 95% confidence interval, 0.082–0.808; P = 0.020), but the incidence of diabetes showed no significant difference across treatment modalities. Over a period of 6 years since diagnosis, we found that patients treated for acromegaly had a significantly higher survival rate than those untreated (P < 0.001).
Conclusion
The annual incidence rate of Korean patients with acromegaly was similar to that reported in previous studies. Using nationwide population data, our study emphasized the importance of treatment in acromegaly patients.
Keyword
Figure
Cited by 1 articles
-
Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinol Metab. 2023;38(1):10-24. doi: 10.3803/EnM.2023.102.
Reference
-
1. Melmed S. Acromegaly pathogenesis and treatment. J Clin Invest. 2009; 119(11):3189–3202. PMID: 19884662.
Article2. Melmed S. Acromegaly and cancer: not a problem? J Clin Endocrinol Metab. 2001; 86(7):2929–2934. PMID: 11443145.3. Holdaway IM, Bolland MJ, Gamble GD. A meta-analysis of the effect of lowering serum levels of GH and IGF-I on mortality in acromegaly. Eur J Endocrinol. 2008; 159(2):89–95. PMID: 18524797.
Article4. Dekkers OM, Biermasz NR, Pereira AM, Romijn JA, Vandenbroucke JP. Mortality in acromegaly: a metaanalysis. J Clin Endocrinol Metab. 2008; 93(1):61–67. PMID: 17971431.
Article5. Melmed S, Bronstein MD, Chanson P, Klibanski A, Casanueva FF, Wass JA, et al. A Consensus Statement on acromegaly therapeutic outcomes. Nat Rev Endocrinol. 2018; 14(9):552–561. PMID: 30050156.
Article6. Lavrentaki A, Paluzzi A, Wass JA, Karavitaki N. Epidemiology of acromegaly: review of population studies. Pituitary. 2017; 20(1):4–9. PMID: 27743174.
Article7. Yang IM. Clinical characteristics of acromegalic patients in Korea. J Korean Endocr Soc. 1994; 9(4):290–306.8. Kwon O, Song YD, Kim SY, Lee EJ; Rare Disease Study Group, Science and Research Committee, Korean Endocrine Society. Nationwide survey of acromegaly in South Korea. Clin Endocrinol (Oxf). 2013; 78(4):577–585. PMID: 22909047.
Article9. Park KH, Lee EJ, Seo GH, Ku CR. Risk for acromegaly-related comorbidities by sex in Korean acromegaly. J Clin Endocrinol Metab. 2020; 105(4):e1815–26.
Article10. Holdaway IM, Rajasoorya RC, Gamble GD. Factors influencing mortality in acromegaly. J Clin Endocrinol Metab. 2004; 89(2):667–674. PMID: 14764779.
Article11. Kauppinen-Mäkelin R, Sane T, Reunanen A, Välimäki MJ, Niskanen L, Markkanen H, et al. A nationwide survey of mortality in acromegaly. J Clin Endocrinol Metab. 2005; 90(7):4081–4086. PMID: 15886256.
Article12. Bolfi F, Neves AF, Boguszewski CL, Nunes-Nogueira VS. Mortality in acromegaly decreased in the last decade: a systematic review and meta-analysis. Eur J Endocrinol. 2018; 179(1):59–71. PMID: 29764907.
Article13. Wen-Ko C, Szu-Tah C, Feng-Hsuan L, Chen-Nen C, Ming-Hsu W, Jen-Der L. The impact of diabetes mellitus on the survival of patients with acromegaly. Endokrynol Pol. 2016; 67(5):501–506. PMID: 26884300.14. Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46(3):799–800. PMID: 27794523.15. Bae SO, Kang GW. A comparative study of the disease codes between Korean national health insurance claims and Korean national hospital discharge in-depth injury survey. Health Policy Manag. 2014; 24(4):322–329.
Article16. Bridgman PW. The Logic of Modern Physics. New York, NY, USA: Macmillan;1927.17. National Health Insurance Service. National Health Insurance System of Korea. Wonju, Korea: National Health Insurance Service;2015.18. Gadelha MR, Kasuki L, Lim DS, Fleseriu M. Systemic complications of acromegaly and the impact of the current treatment landscape: an update. Endocr Rev. 2019; 40(1):268–332. PMID: 30184064.
Article19. Vila G, Luger A, van der Lely AJ, Neggers SJ, Webb SM, Biller BM, et al. Hypertension in acromegaly in relationship to biochemical control and mortality: global ACROSTUDY outcomes. Front Endocrinol (Lausanne). 2020; 11:577173. PMID: 33329385.
Article20. Vitale G, Pivonello R, Auriemma RS, Guerra E, Milone F, Savastano S, et al. Hypertension in acromegaly and in the normal population: prevalence and determinants. Clin Endocrinol (Oxf). 2005; 63(4):470–476. PMID: 16181242.
Article21. Ferraù F, Albani A, Ciresi A, Giordano C, Cannavò S. Diabetes secondary to acromegaly: physiopathology, clinical features and effects of treatment. Front Endocrinol (Lausanne). 2018; 9(358):358. PMID: 30034367.
Article22. Kamenicky P, Viengchareun S, Blanchard A, Meduri G, Zizzari P, Imbert-Teboul M, et al. Epithelial sodium channel is a key mediator of growth hormone-induced sodium retention in acromegaly. Endocrinology. 2008; 149(7):3294–3305. PMID: 18388193.
Article23. Bielohuby M, Roemmler J, Manolopoulou J, Johnsen I, Sawitzky M, Schopohl J, et al. Chronic growth hormone excess is associated with increased aldosterone: a study in patients with acromegaly and in growth hormone transgenic mice. Exp Biol Med (Maywood). 2009; 234(8):1002–1009. PMID: 19491373.
Article24. Powlson AS, Gurnell M. Cardiovascular disease and sleep-disordered breathing in acromegaly. Neuroendocrinology. 2016; 103(1):75–85. PMID: 26227953.
Article25. Bondanelli M, Ambrosio MR, degli Uberti EC. Pathogenesis and prevalence of hypertension in acromegaly. Pituitary. 2001; 4(4):239–249. PMID: 12501974.26. Colao A, Auriemma RS, Galdiero M, Lombardi G, Pivonello R. Effects of initial therapy for five years with somatostatin analogs for acromegaly on growth hormone and insulin-like growth factor-I levels, tumor shrinkage, and cardiovascular disease: a prospective study. J Clin Endocrinol Metab. 2009; 94(10):3746–3756. PMID: 19622615.
Article27. Helseth R, Carlsen SM, Bollerslev J, Svartberg J, Øksnes M, Skeie S, et al. Preoperative octreotide therapy and surgery in acromegaly: associations between glucose homeostasis and treatment response. Endocrine. 2016; 51(2):298–307. PMID: 26179177.
Article28. Kinoshita Y, Fujii H, Takeshita A, Taguchi M, Miyakawa M, Oyama K, et al. Impaired glucose metabolism in Japanese patients with acromegaly is restored after successful pituitary surgery if pancreatic {beta}-cell function is preserved. Eur J Endocrinol. 2011; 164(4):467–473. PMID: 21285083.29. Shekhawat VS, Bhansali S, Dutta P, Mukherjee KK, Vaiphei K, Kochhar R, et al. Glucose-dependent Insulinotropic Polypeptide (GIP) Resistance and β-cell Dysfunction Contribute to Hyperglycaemia in Acromegaly. Sci Rep. 2019; 9(1):5646. PMID: 30948746.
Article30. Kim DJ, Lee MS, Kim KW, Lee MK. Insulin secretory dysfunction and insulin resistance in the pathogenesis of Korean type 2 diabetes mellitus. Metabolism. 2001; 50(5):590–593. PMID: 11319722.
Article31. Henry RR, Ciaraldi TP, Armstrong D, Burke P, Ligueros-Saylan M, Mudaliar S. Hyperglycemia associated with pasireotide: results from a mechanistic study in healthy volunteers. J Clin Endocrinol Metab. 2013; 98(8):3446–3453. PMID: 23733372.
Article32. Strowski MZ, Parmar RM, Blake AD, Schaeffer JM. Somatostatin inhibits insulin and glucagon secretion via two receptors subtypes: an in vitro study of pancreatic islets from somatostatin receptor 2 knockout mice. Endocrinology. 2000; 141(1):111–117. PMID: 10614629.33. Gadelha MR, Bronstein MD, Brue T, Coculescu M, Fleseriu M, Guitelman M, et al. Pasireotide versus continued treatment with octreotide or lanreotide in patients with inadequately controlled acromegaly (PAOLA): a randomised, phase 3 trial. Lancet Diabetes Endocrinol. 2014; 2(11):875–884. PMID: 25260838.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Medical Treatment of Acromegaly
- Characteristics of Acromegaly in Korea with a Literature Review
- Multiomics Approach to Acromegaly: Unveiling Translational Insights for Precision Medicine
- A case of acromegaly with empty sella syndrome associated with colonic neoplasm
- A Case of Acromegaly First Diagnosed in Pregnancy