J Korean Med Sci.
2021 May;36(21):e141. 10.3346/jkms.2021.36.e141.
The Use of Point-of-care Ultrasound in Emergency Medical Centers in Korea: a National Cross-sectional Survey
- Affiliations
-
- 1Department of Emergency Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2516250
- DOI: http://doi.org/10.3346/jkms.2021.36.e141
Abstract
- Background
Point-of-care ultrasound (POCUS) is an essential tool in emergency medicine (EM). We aimed to investigate the current status and perception of POCUS use in emergency medical centers in Korea.
Methods
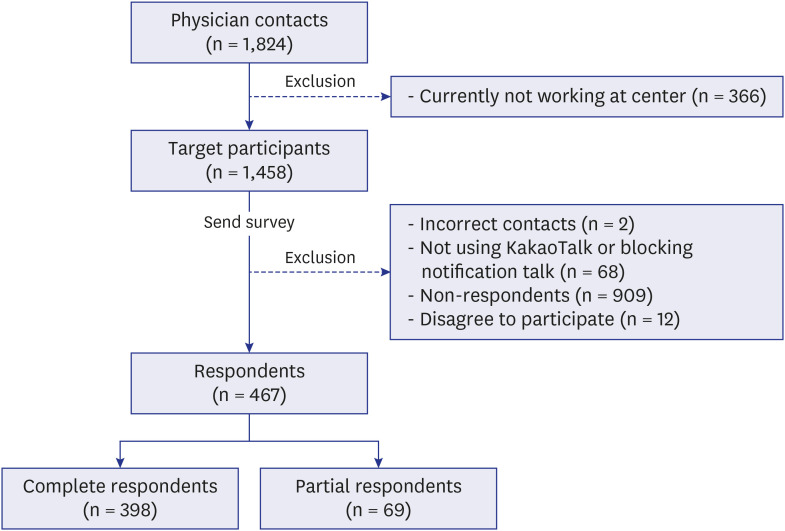
A cross-sectional, nationwide survey was conducted using a mobile survey of physicians at emergency medical centers in Korea. The first message was sent on November 27, 2020, and the second message was sent on December 3, 2020 to the non-responders. The questionnaire comprised 6 categories and 24 questionnaires on demographics, current practice, education, perception, and barriers to the use of POCUS.
Results
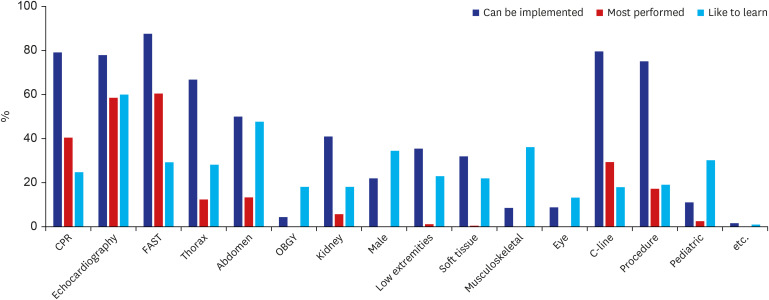
A total of 467 physicians participated in the survey (a response rate of 32% among 1,458 target physicians), of which 43% were residents and 57% were EM specialists. Most of the respondents (96%) answered that they use POCUS, of which 89% reported using it at least once a week. The most frequently used types of POCUS were focused assessment with sonography for trauma (68%) and echocardiography (66%). Musculoskeletal, male genital, and pediatric scans were rarely performed tests but ranked as of the scans physicians most wanted to learn. About 73% of the respondents received ultrasound education, and 41% received ultrasound education at their own institutions. Nevertheless, educationrelated barriers are still the biggest deterrent to POCUS use (60%). In addition, multivariate multinomial logistic regression analysis revealed that the greater the number of ultrasound devices and the total number of physicians in the emergency center, the more likely they were to use POCUS every day.
Conclusion
This study found that most physicians currently working in emergency medical centers in Korea more frequently perform various types of ultrasound scans compared to those 10 years prior. To further promote the use of POCUS, it is important to have an appropriate number of ultrasound devices and physicians in the emergency center along with systematic POCUS education.
Figure
Reference
-
1. Jehle D, Davis E, Evans T, Harchelroad F, Martin M, Zaiser K, et al. Emergency department sonography by emergency physicians. Am J Emerg Med. 1989; 7(6):605–611. PMID: 2679578.
Article2. Plummer D. Whose turf is it, anyway? Diagnostic ultrasonography in the emergency department. Acad Emerg Med. 2000; 7(2):186–187. PMID: 10691079.
Article3. Schlager D, Lazzareschi G, Whitten D, Sanders AB. A prospective study of ultrasonography in the ED by emergency physicians. Am J Emerg Med. 1994; 12(2):185–189. PMID: 8161394.
Article4. Durston W, Carl ML, Guerra W. Patient satisfaction and diagnostic accuracy with ultrasound by emergency physicians. Am J Emerg Med. 1999; 17(7):642–646. PMID: 10597080.
Article5. Boniface KS, Drake A, Pyle M, Moideen F, Mehta S, Poovathumparambil V, et al. Learner-centered survey of point-of-care ultrasound training, competence, and implementation barriers in emergency medicine training programs in India. AEM Educ Train. 2019; 4(4):387–394. PMID: 33150281.
Article6. Beeson MS, Ankel F, Bhat R, Broder JS, Dimeo SP, Gorgas DL, et al. The 2019 Model of the Clinical Practice of Emergency Medicine. J Emerg Med. 2020; 59(1):96–120. PMID: 32475725.
Article7. American College of Emergency Physicians. Ultrasound guidelines: emergency, point-of -care, and clinical ultrasound guidelines in medicine. Updated 2016. Accessed November 30, 2020. https://www.acep.org/patient-care/policy-statements/ultrasound-guidelines-emergency-point-of--care-and-clinical-ultrasound-guidelines-in-medicine/.8. Labovitz AJ, Noble VE, Bierig M, Goldstein SA, Jones R, Kort S, et al. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr. 2010; 23(12):1225–1230. PMID: 21111923.
Article9. Counselman FL, Sanders A, Slovis CM, Danzl D, Binder LS, Perina DG. The status of bedside ultrasonography training in emergency medicine residency programs. Acad Emerg Med. 2003; 10(1):37–42. PMID: 12511313.
Article10. Park IY. History and future of medical ultrasound. J Surg Ultrasound. 2014; 1(1):1–4.11. Korea Ministry of Government Legislation. Annual training curriculum for resident. Updated 2002. Accessed February 6, 2021. https://www.law.go.kr/.12. Lee JJ, Kang BS, Cho YS, Lee YJ, Lee JH, Park YS, et al. The current status and activities of emergency physician-performed ultrasonography in Seoul and Gyeonggi do. J Korean Soc Emerg Med. 2010; 21(2):166–174.13. Lee JH, Kang B, Kwon H, Kim S, Kim JY, Lee JH, et al. The experience of emergency pediatric ultrasound education course. Ped Emerg Med J. 2014; 1(1):34–41.
Article14. Kim JS, Cho YS, Kim YS, Ha YR, Kang BS, Chung HS, et al. Development of an emergency abdominal ultrasound course in Korea: 1-year experience. J Korean Soc Emerg Med. 2010; 21(3):382–387.15. Health Insurance Review & Assessment Service. Medical information: Easy-to-understand salary benefits - Ultrasonography. Updated 2019. Accessed February 6, 2021. http://www.hira.or.kr/rd/insuadtcrtr/bbsView.do?pgmid=HIRAA030069000400&brdScnBltNo=4&brdBltNo=51292.16. Keenan SP. Use of ultrasound to place central lines. J Crit Care. 2002; 17(2):126–137. PMID: 12096376.
Article17. Sofia S, Angelini F, Cianci V, Copetti R, Farina R, Scuderi M. Diffusion and practice of ultrasound in emergency medicine departments in Italy. J Ultrasound. 2009; 12(3):112–117. PMID: 23396902.
Article18. Dinh VA, Fu JY, Lu S, Chiem A, Fox JC, Blaivas M. Integration of ultrasound in medical education at United States medical schools: a national survey of directors' experiences. J Ultrasound Med. 2016; 35(2):413–419. PMID: 26782166.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Point-of-care ultrasound for airway management in the emergency and critical care setting
- Operational status of Korean emergency medical institutions in preparation for infectious disease outbreak after COVID-19 pandemic: 1 year later
- Cat got your artery? Point of care ultrasound in the evaluation of penetrating trauma by a feline: a case report
- Parental satisfaction with pediatric emergency care: a nationwide, cross-sectional survey in Korea
- Spontaneous elbow hemarthrosis identified by point-of-care ultrasound