Arch Hand Microsurg.
2021 Jun;26(2):100-108. 10.12790/ahm.20.0071.
Novel Recipient Site for Aesthetic Inset of Vascularized Lymph Node Transfer: Preliminary Report
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Pusan National University School of Medicine, Busan, Korea
- 2Biomedical Research Institute, Pusan National University Hospital, Busan, Korea
- 3Department of Rehabilitation Medicine, Pusan National University School of Medicine, Busan, Korea
- KMID: 2516154
- DOI: http://doi.org/10.12790/ahm.20.0071
Abstract
- Purpose
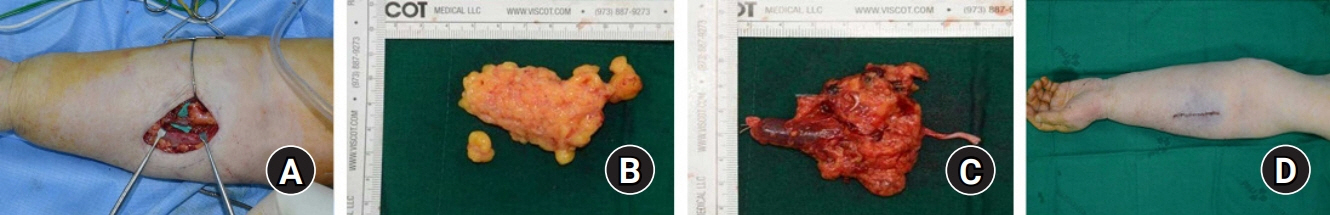
The wrist, elbow, and axillae are recipient sites for vascularized lymph node transfer (VLNT) in upper extremity lymphedema. To the best of our knowledge, the possibility of the forearm as a recipient site for the VLNT has not been extensively investigated. We introduced a novel recipient site and surgical technique for VLNT in the distal upper extremity without a skin paddle.
Methods
Between January 2018 and February 2019, five consecutive patients underwent VLNT for upper extremity lymphedema. A vascularized supraclavicular lymph node was harvested and transferred to the mid-forearm of the lymphedematous limb. Radial artery, venae comitantes, and superficial vein were used as recipient vessels. Outcome was assessed by upper limb circumference and volume.
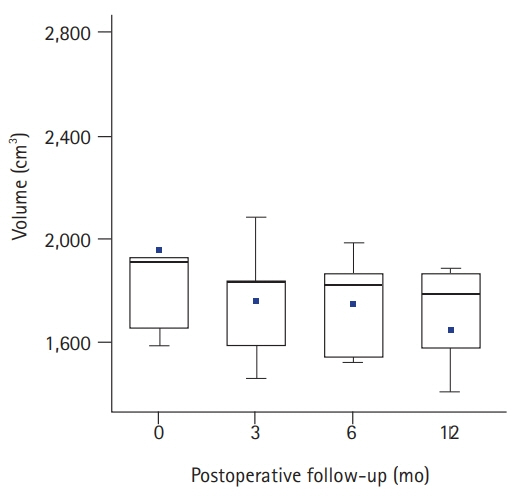
Results
All flaps survived without any donor-site morbidity. All patients reported symptom improvement. Mean circumference and volume at 3, 6, and 12 months after VLNT were reduced statistically significantly (p<0.05). Volume differential reduction was significant (p=0.005), showing an increasing tendency (p=0.050).
Conclusion
The forearm appears to be an excellent recipient site owing to its aesthetic and surgical benefits.
Figure
Reference
-
1. Viitanen TP, Mäki MT, Seppänen MP, Suominen EA, Saaristo AM. Donor-site lymphatic function after microvascular lymph node transfer. Plast Reconstr Surg. 2012; 130:1246–53.
Article2. Najjar M, Lopez MM Jr, Ballestin A, et al. Reestablishment of lymphatic drainage after vascularized lymph node transfer in a rat model. Plast Reconstr Surg. 2018; 142:503e–508e.
Article3. Silva AK, Chang DW. Vascularized lymph node transfer and lymphovenous bypass: novel treatment strategies for symptomatic lymphedema. J Surg Oncol. 2016; 113:932–9.
Article4. Nicoli F, Orfaniotis G, Ciudad P, et al. Alternative vascular constructs of lymph node flap transfer. J Surg Oncol. 2018; 117:1144–7.
Article5. Yamamoto T, Iida T, Yoshimatsu H, Fuse Y, Hayashi A, Yamamoto N. Lymph flow restoration after tissue replantation and transfer: importance of lymph axiality and possibility of lymph flow reconstruction without lymph node transfer or lymphatic anastomosis. Plast Reconstr Surg. 2018; 142:796–804.6. Kim KW, Song JH. Emerging roles of lymphatic vasculature in immunity. Immune Netw. 2017; 17:68–76.
Article7. Bernier-Latmani J, Petrova TV. Intestinal lymphatic vasculature: structure, mechanisms and functions. Nat Rev Gastroenterol Hepatol. 2017; 14:510–26.
Article8. Iwasaki D, Yamamoto Y, Murao N, Oyama A, Funayama E, Furukawa H. Establishment of an acquired lymphedema model in the mouse hindlimb: technical refinement and molecular characteristics. Plast Reconstr Surg. 2017; 139:67e–78e.9. Ogata F, Fujiu K, Koshima I, Nagai R, Manabe I. Phenotypic modulation of smooth muscle cells in lymphoedema. Br J Dermatol. 2015; 172:1286–93.
Article10. Rockson SG. The unique biology of lymphatic edema. Lymphat Res Biol. 2009; 7:97–100.
Article11. Kwak MD, Machens HG. The lateral intercostal artery perforator as an alternative donor vessel for free vascularized lymph node transplantation. Arch Plast Surg. 2018; 45:275–9.
Article12. Koshima I, Inagawa K, Urushibara K, Moriguchi T. Supermicrosurgical lymphaticovenular anastomosis for the treatment of lymphedema in the upper extremities. J Reconstr Microsurg. 2000; 16:437–42.
Article13. Becker C. Autologous lymph node transfers. J Reconstr Microsurg. 2016; 32:28–33.
Article14. Visconti G, Constantinescu T, Chen HC. The venous lymph-node flap. Microsurgery. 2016; 36:527–8.
Article15. Teven CM, Ooi AS, Inbal A, Chang DW. Implantable Doppler monitoring of buried free flaps during vascularized lymph node transfer. J Surg Oncol. 2017; 116:371–7.
Article16. Tourani SS, Taylor GI, Ashton MW. Vascularized lymph node transfer: a review of the current evidence. Plast Reconstr Surg. 2016; 137:985–93.17. Cheng MH, Chen SC, Henry SL, Tan BK, Chia-Yu Lin M, Huang JJ. Vascularized groin lymph node flap transfer for postmastectomy upper limb lymphedema: flap anatomy, recipient sites, and outcomes. Plast Reconstr Surg. 2013; 131:1286–98.18. Gould DJ, Mehrara BJ, Neligan P, Cheng MH, Patel KM. Lymph node transplantation for the treatment of lymphedema. J Surg Oncol. 2018; 118:736–42.
Article19. Chu SY, Wang SC, Chan WH, et al. Volumetric differences in the suprafascial and subfascial compartments of patients with secondary unilateral lower limb lymphedema. Plast Reconstr Surg. 2020; 145:1528–37.
Article20. Cheng MH, Chang DW, Patel KM. Principles and practice of lymphedema surgery. Edinburgh: Elsevier;2016.21. Becker C, Assouad J, Riquet M, Hidden G. Postmastectomy lymphedema: long-term results following microsurgical lymph node transplantation. Ann Surg. 2006; 243:313–5.22. You JM, Wu YS, Wang Y. Comparison of post-operative numbness and patient satisfaction using minimally invasive plate osteosynthesis or open plating for acute displaced clavicular shaft fractures. Int J Surg. 2018; 56:21–5.
Article23. Nathe T, Tseng S, Yoo B. The anatomy of the supraclavicular nerve during surgical approach to the clavicular shaft. Clin Orthop Relat Res. 2011; 469:890–4.
Article24. Vathulya M, Ansari MS. An important superficial vein of the radial aspect of the forearm: an anatomical study. Indian J Plast Surg. 2018; 51:231–4.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- No-fat diet for treatment of donor site chyle leakage in vascularized supraclavicular lymph node transfer
- Vascularized Free Lymph Node Flap Transfer in Advanced Lymphedema Patient after Axillary Lymph Node Dissection
- Free Vascularized Osteocutaneous Fibular Graft To The Tibia
- Surgical treatment of lymphedema
- Surgical Management of Lymphedema: An Overview of Preoperative Evaluation and Surgical Techniques