J Korean Med Sci.
2021 May;36(19):e130. 10.3346/jkms.2021.36.e130.
Current Asthma Prevalence Using Methacholine Challenge Test in Korean Children from 2010 to 2014
- Affiliations
-
- 1Department of Pediatrics, Inha University School of Medicine, Inha University Hospital, Incheon, Korea
- KMID: 2515865
- DOI: http://doi.org/10.3346/jkms.2021.36.e130
Abstract
- Background
Most epidemiological studies depend on the subjects' response to asthma symptom questionnaires. Questionnaire-based study for childhood asthma prevalence may overestimate the true prevalence. The aim of this study was to investigate the prevalence of “Current asthma” using the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire and methacholine challenge test in Korean children.
Methods
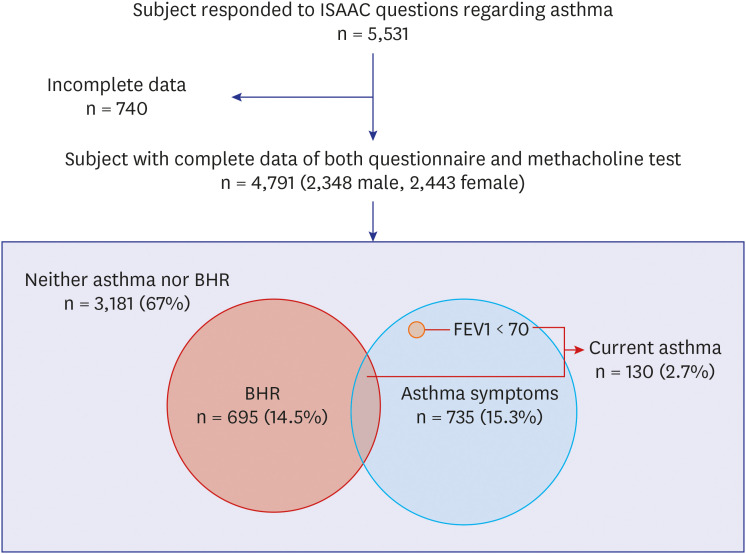
Our survey on allergic disease included 4,791 children (age 7–12 years) from 2010 to 2014 in Korean elementary schools. Bronchial hyperresponsiveness (BHR) was defined as provocative concentration of methacholine causing a 20% fall in forced expiratory volume in one second (FEV1) (PC20) ≤ 16 mg/mL. “Current asthma symptoms” was defined as positive response to “Wheezing, current,” “Treatment, current,” or “Exercise, current.” “Current asthma” was defined when the subjects with “Current asthma symptoms” showed BHR on the methacholine challenge test or had less than 70% of predicted FEV1 value.
Results
The prevalence of “Wheezing, ever,” “Wheezing, current,” “Diagnosis, ever,” “Treatment, current,” “Exercise, current,” and “Current asthma symptoms” was 19.6%, 6.9%, 10.0%, 3.3%, 3.5%, and 9.6%, respectively, in our cross-sectional study of Korean elementary school students. The prevalence of BHR in elementary school students was 14.5%. The prevalence of BHR in children with “Wheezing, ever,” “Wheezing, current,” “Diagnosis, ever,” “Treatment, current,” and “Exercise, current” was 22.3%, 30.5%, 22.4%, 28.8%, and 29.9%, respectively. BHR was 26.1% in those with “Current asthma symptoms.”The prevalence of “Current asthma” was 2.7%.
Conclusions
Our large-scale study provides 2.7% prevalence of current asthma in Korean elementary school children. Since approximately one third of the children who have “Current asthma symptoms” present BHR, both subjective and objective methods are required to accurately predict asthma in subjects with asthma symptoms.
Figure
Reference
-
1. Asher MI, Keil U, Anderson HR, Beasley R, Crane J, Martinez F, et al. International study of asthma and allergies in childhood (ISAAC): rationale and methods. Eur Respir J. 1995; 8(3):483–491. PMID: 7789502.
Article2. Cockcroft DW. Nonallergic airway responsiveness. J Allergy Clin Immunol. 1988; 81(1):111–119. PMID: 3276756.
Article3. Toelle BG, Peat JK, Salome CM, Mellis CM, Woolcock AJ. Toward a definition of asthma for epidemiology. Am Rev Respir Dis. 1992; 146(3):633–637. PMID: 1519839.
Article4. Gruchalla RS, Gan V, Roy L, Bokovoy J, McDermott S, Lawrence G, et al. Results of an inner-city school-based asthma and allergy screening pilot study: a combined approach using written questionnaires and step testing. Ann Allergy Asthma Immunol. 2003; 90(5):491–499. PMID: 12775130.
Article5. Yavuz ST, Civelek E, Tuncer A, Sahiner UM, Sekerel BE. Predictive factors for airway hyperresponsiveness in children with respiratory symptoms. Ann Allergy Asthma Immunol. 2011; 106(5):365–370. PMID: 21530866.
Article6. Kim MH, Kwon JW, Kim HB, Song Y, Yu J, Kim WK, et al. Parent-reported ISAAC written questionnaire may underestimate the prevalence of asthma in children aged 10–12 years. Pediatr Pulmonol. 2012; 47(1):36–43. PMID: 21830311.
Article7. Kim YY, Cho SH, Kim WK, Park JK, Song SH, Kim YK, et al. Prevalence of childhood asthma based on questionnaires and methacholine bronchial provocation test in Korea. Clin Exp Allergy. 1997; 27(7):761–768. PMID: 9249268.
Article8. Kim MS, Kim YH, Suh DI, Koh YY, Kim BJ, Kim HB, et al. The prevalence of bronchial hyperresponsiveness in elementary school children and its associated factors. Allergy Asthma Respir Dis. 2014; 2(3):171–178.
Article9. Crapo RO, Casaburi R, Coates AL, Enright PL, Hankinson JL, Irvin CG, et al. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med. 2000; 161(1):309–329. PMID: 10619836.10. Lee SI, Shin MH, Lee HB, Lee JS, Son BK, Koh YY, et al. Prevalences of symptoms of asthma and other allergic diseases in Korean children: a nationwide questionnaire survey. J Korean Med Sci. 2001; 16(2):155–164. PMID: 11306740.
Article11. Hong SJ, Ahn KM, Lee SY, Kim KE. The prevalences of asthma and allergic diseases in Korean children. Korean J Pediatr. 2008; 51(4):343–350.
Article12. Suh M, Kim HH, Sohn MH, Kim KE, Kim C, Shin DC. Prevalence of allergic diseases among Korean school-age children: a nationwide cross-sectional questionnaire study. J Korean Med Sci. 2011; 26(3):332–338. PMID: 21394299.
Article13. Hong SJ, Kim SW, Oh JW, Rah YH, Ahn YM, Kim KE, et al. The validity of the ISAAC written questionnaire and the ISAAC video questionnaire (AVQ 3.0) for predicting asthma associated with bronchial hyperreactivity in a group of 13–14 year old Korean schoolchildren. J Korean Med Sci. 2003; 18(1):48–52. PMID: 12589086.14. Kwon JW, Kim BJ, Song Y, Seo JH, Kim TH, Yu J, et al. Changes in the prevalence of childhood asthma in Seoul from 1995 to 2008 and its risk factors. Allergy Asthma Immunol Res. 2011; 3(1):27–33. PMID: 21217922.
Article15. Pearce N, Aït-Khaled N, Beasley R, Mallol J, Keil U, Mitchell E, et al. Worldwide trends in the prevalence of asthma symptoms: phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax. 2007; 62(9):758–766. PMID: 17504817.
Article16. Harmsen L, Ulrik CS, Porsbjerg C, Thomsen SF, Holst C, Backer V. Airway hyperresponsiveness and development of lung function in adolescence and adulthood. Respir Med. 2014; 108(5):752–757. PMID: 24512967.
Article17. Leynaert B, Bousquet J, Henry C, Liard R, Neukirch F. Is bronchial hyperresponsiveness more frequent in women than in men? A population-based study. Am J Respir Crit Care Med. 1997; 156(5):1413–1420. PMID: 9372654.18. Joseph-Bowen J, de Klerk NH, Firth MJ, Kendall GE, Holt PG, Sly PD. Lung function, bronchial responsiveness, and asthma in a community cohort of 6-year-old children. Am J Respir Crit Care Med. 2004; 169(7):850–854. PMID: 14742300.
Article19. Jayet PY, Schindler C, Künzli N, Zellweger JP, Brändli O, Perruchoud AP, et al. Reference values for methacholine reactivity (SAPALDIA study). Respir Res. 2005; 6:131. PMID: 16271144.
Article20. Shaw R, Woodman K, Ayson M, Dibdin S, Winkelmann R, Crane J, et al. Measuring the prevalence of bronchial hyper-responsiveness in children. Int J Epidemiol. 1995; 24(3):597–602. PMID: 7672902.
Article21. Lee E, Kim YH, Han S, Yang SI, Jung YH, Seo JH, et al. Different cutoff values of methacholine bronchial provocation test depending on age in children with asthma. World J Pediatr. 2017; 13(5):439–445. PMID: 28276002.
Article22. Frye C, Heinrich J, Wjst M, Wichmann HE. Bitterfeld Study Group. Increasing prevalence of bronchial hyperresponsiveness in three selected areas in East Germany. Eur Respir J. 2001; 18(3):451–458. PMID: 11589341.
Article23. von Mutius E, Weiland SK, Fritzsch C, Duhme H, Keil U. Increasing prevalence of hay fever and atopy among children in Leipzig, East Germany. Lancet. 1998; 351(9106):862–866. PMID: 9525363.
Article24. Zöllner IK, Weiland SK, Piechotowski I, Gabrio T, von Mutius E, Link B, et al. No increase in the prevalence of asthma, allergies, and atopic sensitisation among children in Germany: 1992–2001. Thorax. 2005; 60(7):545–548. PMID: 15994260.
Article25. Huang SJ, Lin LL, Chen LC, Ou LS, Yao TC, Tsao KC, et al. Prevalence of airway hyperresponsiveness and its seasonal variation in children with asthma. Pediatr Neonatol. 2018; 59(6):561–566. PMID: 29398555.
Article26. Ernst P, Ghezzo H, Becklake MR. Risk factors for bronchial hyperresponsiveness in late childhood and early adolescence. Eur Respir J. 2002; 20(3):635–639. PMID: 12358340.
Article27. Xuan W, Peat JK, Toelle BG, Marks GB, Berry G, Woolcock AJ. Lung function growth and its relation to airway hyperresponsiveness and recent wheeze. Results from a longitudinal population study. Am J Respir Crit Care Med. 2000; 161(6):1820–1824. PMID: 10852751.28. Becklake MR, Kauffmann F. Gender differences in airway behaviour over the human life span. Thorax. 1999; 54(12):1119–1138. PMID: 10567633.
Article29. Kim YH, Lee E, Cho HJ, Yang SI, Jung YH, Kim HY, et al. Association between menarche and increased bronchial hyper-responsiveness during puberty in female children and adolescents. Pediatr Pulmonol. 2016; 51(10):1040–1047. PMID: 27105475.
Article30. Fuseini H, Newcomb DC. Mechanisms driving gender differences in asthma. Curr Allergy Asthma Rep. 2017; 17(3):19. PMID: 28332107.
Article31. Peat JK, Salome CM, Woolcock AJ. Factors associated with bronchial hyperresponsiveness in Australian adults and children. Eur Respir J. 1992; 5(8):921–929. PMID: 1426199.32. Le Souëf PN, Sears MR, Sherrill D. The effect of size and age of subject on airway responsiveness in children. Am J Respir Crit Care Med. 1995; 152(2):576–579. PMID: 7633710.
Article33. Siroux V, Curt F, Oryszczyn MP, Maccario J, Kauffmann F. Role of gender and hormone-related events on IgE, atopy, and eosinophils in the Epidemiological Study on the Genetics and Environment of Asthma, Bronchial Hyperresponsiveness and Atopy. J Allergy Clin Immunol. 2004; 114(3):491–498. PMID: 15356546.
Article34. Jee HM, Kim KW, Kim CS, Sohn MH, Shin DC, Kim K. Prevalence of asthma, rhinitis and eczema in Korean children using the International Study of Asthma and Allergies in Childhood (ISAAC) questionnaires. Pediatr Allergy Respir Dis. 2009; 19(2):165–172.35. Ali Z. How to diagnose exercise induced asthma? Asian J Sports Med. 2011; 2(2):63–67. PMID: 22375220.
Article36. Lasmar L, Camargos P, Bousquet J, Goulart E, Sakurai E, Carvalhais M. Factors related to lower adherence rates to inhaled corticosteroids in children and adolescents: a prospective randomized cohort study. J Trop Pediatr. 2009; 55(1):20–25. PMID: 18820317.
Article37. Lasmar LM, Camargos PA, Costa LF, Fonseca MT, Fontes MJ, Ibiapina CC, et al. Compliance with inhaled corticosteroid treatment: rates reported by guardians and measured by the pharmacy. J Pediatr (Rio J). 2007; 83(5):471–476. PMID: 17940683.
Article38. Jónasson G, Carlsen KH, Mowinckel P. Asthma drug adherence in a long term clinical trial. Arch Dis Child. 2000; 83(4):330–333. PMID: 10999870.39. Kim CK, Callaway Z, Choi J, Kim HB, Kwon EM, Chang YS, et al. Multicenter adherence study of asthma medication for children in Korea. Allergy Asthma Immunol Res. 2019; 11(2):222–230. PMID: 30661314.
Article40. Ryhal B. Viral disease, air pollutants, nanoparticles, and asthma. In : Gershwin M, Albertson T, editors. Bronchial Asthma. New York, NY, USA: Springer;2012. p. 267–283. DOI: 10.1007/978-1-4419-6836-4_11. .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bronchial Asthma with Negative Methacholine Challenge Test
- Clinical Characteristics of Asthmatics Having Negative Results to Methacholine Bronchial Challenge Test
- Correlation between Methacholine Bronchial Hyperresponsiveness and Peak Expiratory Flow Variability in Children with Asthma
- Prediction of Airway Hyperresponsiveness by Asthma Questionaire in Compare with Methacholine Challenge Test
- Prevalence of adult asthma based on questionnaires and methacholine bronchial provocation test in Seoul