J Korean Med Sci.
2021 May;36(18):e120. 10.3346/jkms.2021.36.e120.
Male Sex Is a Significant Predictor of All-cause Mortality in Patients with Antineutrophil Cytoplasmic Antibodyassociated Vasculitis
- Affiliations
-
- 1Department of Rheumatology, Dankook University Hospital, Dankook University College of Medicine, Cheonan, Korea
- 2Division of Rheumatology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 3Institute for Immunology and Immunological Diseases, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2515856
- DOI: http://doi.org/10.3346/jkms.2021.36.e120
Abstract
- Background
We investigated and compared the initial clinical features at diagnosis and the poor outcomes during follow-up in Korean patients with antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) based on sex.
Methods
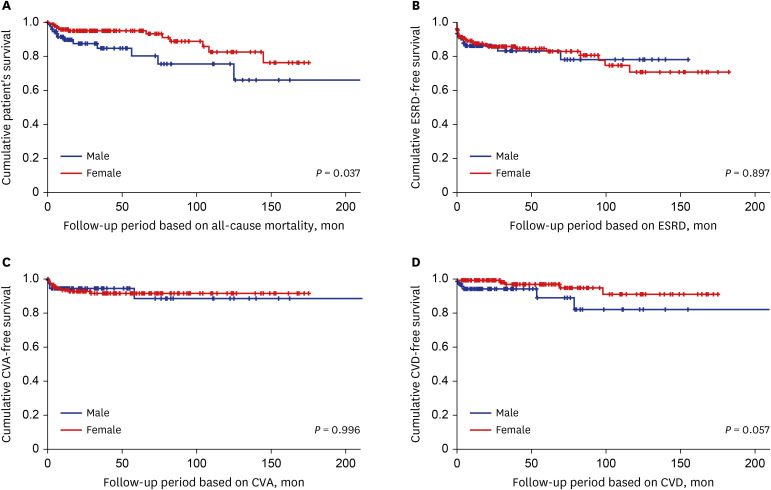
The medical records of 223 immunosuppressive drug-naïve patients with AAV were reviewed. Age, body mass index (BMI), smoking history, AAV subtypes, ANCA positivity, clinical manifestations, Birmingham vasculitis activity score (BVAS), five-factor score (FFS), erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) at diagnosis were collected. All-cause mortality, end-stage renal disease (ESRD), cerebrovascular accident (CVA) and cardiovascular disease (CVD) were assessed as the poor outcomes of AAV during follow-up.
Results
The median age was 59.0 years and 74 of 223 AAV patients (33.2%) were men. Among variables at diagnosis, male patients exhibited higher BMI than female. However, there were no differences in other demographic data, AAV subtypes, ANCA positivity, BVAS, FFS, ESR and CRP between the two groups. Male patients received cyclophosphamide more frequently, but there were no significant differences in the frequencies of the poor outcomes of AAV between the two groups. Male patients exhibited a significantly lower cumulative patients' survival rate than female patients during the follow-up period based on all-cause mortality (P = 0.037). In the multivariable analysis, both male sex (hazard ratio [HR], 2.378) and FFS (HR, 1.693) at diagnosis were significantly and independently associated with allcause mortality during follow-up.
Conclusion
Male sex is a significant and independent predictor of all-cause mortality in AAV patients.
Keyword
Figure
Reference
-
1. Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, et al. 2012 revised International Chapel Hill Consensus Conference Nomenclature of Vasculitides. Arthritis Rheum. 2013; 65(1):1–11. PMID: 23045170.
Article2. Watts R, Lane S, Hanslik T, Hauser T, Hellmich B, Koldingsnes W, et al. Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis. 2007; 66(2):222–227. PMID: 16901958.
Article3. Kermani TA. Takayasu arteritis and giant cell arteritis: are they a spectrum of the same disease? Int J Rheum Dis. 2019; 22(Suppl 1):41–48. PMID: 29624864.
Article4. Ryu HJ, Seo MR, Choi HJ, Baek HJ. Clinical phenotypes of Korean patients with Behcet disease according to gender, age at onset, and HLA-B51. Korean J Intern Med. 2018; 33(5):1025–1031. PMID: 28073242.
Article5. Bjørneklett R, Solbakken V, Bostad L, Fismen AS. Exploring sex-specific differences in the presentation and outcomes of ANCA-associated vasculitis: a nationwide registry-based cohort study. Int Urol Nephrol. 2018; 50(7):1311–1318. PMID: 29790004.
Article6. Mukhtyar C, Lee R, Brown D, Carruthers D, Dasgupta B, Dubey S, et al. Modification and validation of the Birmingham vasculitis activity score (version 3). Ann Rheum Dis. 2009; 68(12):1827–1832. PMID: 19054820.
Article7. Guillevin L, Pagnoux C, Seror R, Mahr A, Mouthon L, Toumelin PL, et al. The five-factor score revisited: assessment of prognoses of systemic necrotizing vasculitides based on the French Vasculitis Study Group (FVSG) cohort. Medicine (Baltimore). 2011; 90(1):19–27. PMID: 21200183.8. McAdoo SP, Medjeral-Thomas N, Gopaluni S, Tanna A, Mansfield N, Galliford J, et al. Long-term follow-up of a combined rituximab and cyclophosphamide regimen in renal anti-neutrophil cytoplasm antibody-associated vasculitis. Nephrol Dial Transplant. 2019; 34(1):63–73. PMID: 29462348.
Article9. Murray CJ, Atkinson C, Bhalla K, Birbeck G, Burstein R, Chou D, et al. The state of US health, 1990-2010: burden of diseases, injuries, and risk factors. JAMA. 2013; 310(6):591–608. PMID: 23842577.10. Crimmins EM, Shim H, Zhang YS, Kim JK. Differences between men and women in mortality and the health dimensions of the morbidity process. Clin Chem. 2019; 65(1):135–145. PMID: 30478135.
Article11. Bhaskaran K, Dos-Santos-Silva I, Leon DA, Douglas IJ, Smeeth L. Association of BMI with overall and cause-specific mortality: a population-based cohort study of 3·6 million adults in the UK. Lancet Diabetes Endocrinol. 2018; 6(12):944–953. PMID: 30389323.
Article12. Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, MacInnis RJ, et al. Body-mass index and mortality among 1.46 million white adults. N Engl J Med. 2010; 363(23):2211–2219. PMID: 21121834.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- ANCA : The Marker Antibody of Vasculitis
- ANCA-Associated Vasculitis Presenting with Hypertrophic Pachymeningitis
- ANCA-Associated Vasculitic Neuropathy with Concurrent Pulmonary Tuberculosis
- Implication of Serious Infections in Patients With Antineutrophil Cytoplasmic Antibody-Associated Vasculitis for the First Cycle of Rituximab: A Pilot Study in a Single Korean Center
- C-Reactive Protein to Serum Albumin Ratio Is an Independent Predictor of All-Cause Mortality in Patients with ANCA-Associated Vasculitis