Anesth Pain Med.
2021 Apr;16(2):119-132. 10.17085/apm.21012.
Ultrasound-guided arterial catheterization
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2515537
- DOI: http://doi.org/10.17085/apm.21012
Abstract
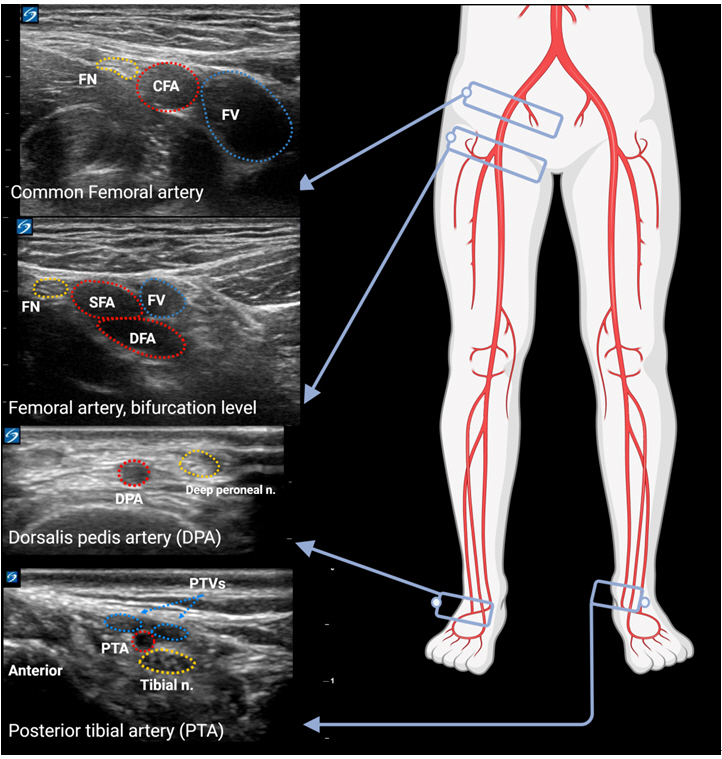
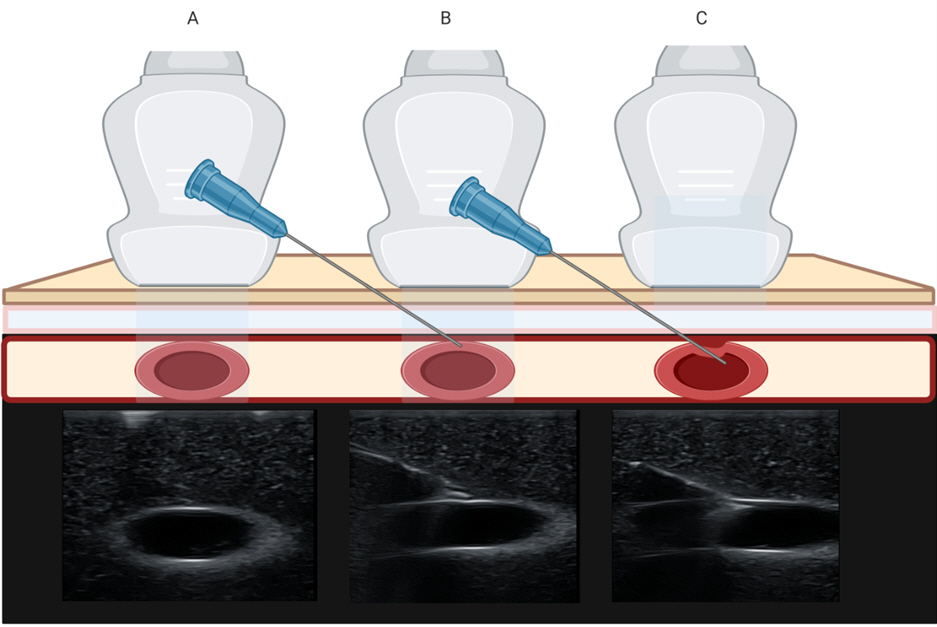
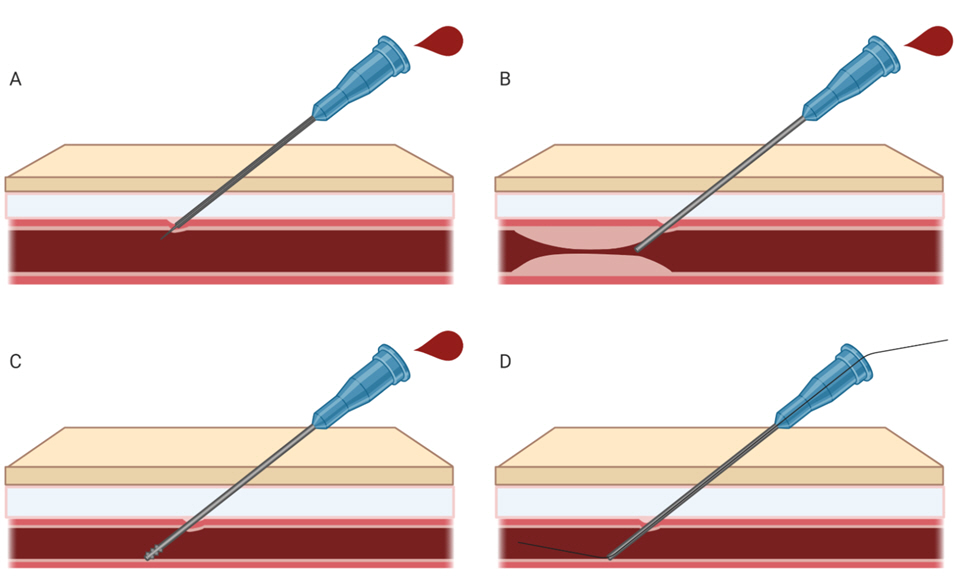
- Ultrasonography facilitates arterial catheterization compared to traditional palpation techniques, especially in small arteries. For successful catheterization without complications, practitioners should be familiar with the anatomic characteristics of the artery and ultrasound-guided techniques. There are two approaches for ultrasound-guided arterial catheterization: the short-axis view out-of-plane approach and the long-axis view in-plane approach. There are several modified techniques and tips to facilitate ultrasound-guided arterial catheterization. This review deals with the anatomy relevant to arterial catheterization, several methods to improve success rates, and decrease complications associated with arterial catheterization.
Keyword
Figure
Reference
-
1. Ishii S, Shime N, Shibasaki M, Sawa T. Ultrasound-guided radial artery catheterization in infants and small children. Pediatr Crit Care Med. 2013; 14:471–3.2. Kim JM, Arakawa K, Bliss J. Arterial cannulation: factors in the development of occlusion. Anesth Analg. 1975; 54:836–41.3. Latham GJ, Bosenberg AT, Low DK. Images in anesthesiology: radial artery spasm in an infant as documented by high-frequency micro-ultrasound. Anesthesiology. 2014; 120:1254.4. Nuttall G, Burckhardt J, Hadley A, Kane S, Kor D, Marienau MS, et al. Surgical and patient risk factors for severe arterial line complications in adults. Anesthesiology. 2016; 124:590–7.5. Gleich SJ, Wong AV, Handlogten KS, Thum DE, Nemergut ME. Major short-term complications of arterial cannulation for monitoring in children. Anesthesiology. 2021; 134:26–34.6. Beniwal S, Bhargava K, Kausik SK. Size of distal radial and distal ulnar arteries in adults of southern Rajasthan and their implications for percutaneous coronary interventions. Indian Heart J. 2014; 66:506–9.7. Ashraf T, Panhwar Z, Habib S, Memon MA, Shamsi F, Arif J. Size of radial and ulnar artery in local population. J Pak Med Assoc. 2010; 60:817–9.8. Kim EH, Lee JH, Song IK, Kim JT, Lee WJ, Kim HS. Posterior tibial artery as an alternative to the radial artery for arterial cannulation site in small children: a randomized controlled study. Anesthesiology. 2017; 127:423–31.9. Jang YE, Ji SH, Kim EH, Lee JH, Kim HS, Mossad EB, et al. Subcutaneous nitroglycerin for radial arterial catheterization in pediatric patients: a randomized controlled trial. Anesthesiology. 2020; 133:53–63.10. Min SW, Cho HR, Jeon YT, Oh AY, Park HP, Yang CW, et al. Effect of bevel direction on the success rate of ultrasound-guided radial arterial catheterization. BMC Anesthesiol. 2016; 16:34.11. Tiru B, Bloomstone JA, McGee WT. Radial artery cannulation: a review article. J Anesth Clin Res. 2012; 3:209.12. Lamperti M, Biasucci DG, Disma N, Pittiruti M, Breschan C, Vailati D, et al. European Society of Anaesthesiology guidelines on peri-operative use of ultrasound-guided for vascular access (PERSEUS vascular access). Eur J Anaesthesiol. 2020; 37:344–76.13. Bertrand OF, Carey PC, Gilchrist IC. Allen or no allen: that is the question! J Am Coll Cardiol. 2014; 63:1842–4.14. Riekkinen HV, Karkola KO, Kankainen A. The radial artery is larger than the ulnar. Ann Thorac Surg. 2003; 75:882–4.15. Schindler E, Kowald B, Suess H, Niehaus-Borquez B, Tausch B, Brecher A. Catheterization of the radial or brachial artery in neonates and infants. Paediatr Anaesth. 2005; 15:677–82.16. Tomiyama Y, Yoshinaga K, Fujii S, Ochi N, Inoue M, Nishida M, et al. Accurate quantitative measurements of brachial artery cross-sectional vascular area and vascular volume elastic modulus using automated oscillometric measurements: comparison with brachial artery ultrasound. Hypertens Res. 2015; 38:478–84.17. Kim EH, Lee HC, Chung J, Ji SH, Jang YE, Lee JH, et al. Flow-mediated dilatation of the brachial artery for assessing endothelial dysfunction in children with Moyamoya disease. Pediatr Neurosurg. 2020; 55:149–54.18. Khan ZA, Khan MA, MohammednourAltaf F, Alkhushi AG, Alasmari WA. Diameter of the dorsalis pedis artery and its clinical relevance. IOSR-JDMS. 2016; 15:129–33.19. Babuccu O, Ozdemir H, Hosnuter M, Kargi E, Söğüt A, Ayoglu FN. Cross-sectional internal diameters of radial, thoracodorsal, and dorsalis pedis arteries in children: relationship to subject sex, age, and body size. J Reconstr Microsurg. 2006; 22:49–52.20. Lorbeer R, Grotz A, Dörr M, Völzke H, Lieb W, Kühn JP, et al. Reference values of vessel diameters, stenosis prevalence, and arterial variations of the lower limb arteries in a male population sample using contrast-enhanced MR angiography. PLoS One. 2018; 13:e0197559.21. Sun J, Ding Z, Qian Y, Peng YG. Central-radial artery pressure gradient after cardiopulmonary bypass is associated with cardiac function and may affect therapeutic direction. PLoS One. 2013; 8:e68890.22. Cho HJ, Lee SH, Jeong IS, Yoon NS, Ma JS, Ahn BH. Differences in perioperative femoral and radial arterial blood pressure in neonates and infants undergoing cardiac surgery requiring cardiopulmonary bypass. J Pediatr (Rio J). 2018; 94:76–81.23. Rudnick MR, Marchi LD, Plotkin JS. Hemodynamic monitoring during liver transplantation: a state of the art review. World J Hepatol. 2015; 7:1302–11.24. Spector KS, Lawson WE. Optimizing safe femoral access during cardiac catheterization. Catheter Cardiovasc Interv. 2001; 53:209–12.25. Bhatia N, Sivaprakasam J, Allford M, Guruswamy V. The relative position of femoral artery and vein in children under general anesthesia--an ultrasound-guided observational study. Paediatr Anaesth. 2014; 24:1164–8.26. Rajebi H, Rajebi MR. Optimizing common femoral artery access. Tech Vasc Interv Radiol. 2015; 18:76–81.27. Troianos CA, Hartman GS, Glas KE, Skubas NJ, Eberhardt RT, Walker JD, et al. Councils on Intraoperative Echocardiography and Vascular Ultrasound of the American Society of Echocardiography. Guidelines for performing ultrasound guided vascular cannulation: recommendations of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2011; 24:1291–318.28. White L, Halpin A, Turner M, Wallace L. Ultrasound-guided radial artery cannulation in adult and paediatric populations: a systematic review and meta-analysis. Br J Anaesth. 2016; 116:610–7.29. Seto AH, Roberts JS, Abu-Fadel MS, Czak SJ, Latif F, Jain SP, et al. Real-time ultrasound guidance facilitates transradial access: RAUST (radial artery access with ultrasound trial). JACC Cardiovasc Interv. 2015; 8:283–91.30. Jang YE, Kim EH, Lee JH, Kim HS, Kim JT. Guidewire-assisted vs. direct radial arterial cannulation in neonates and infants: a randomised controlled trial. Eur J Anaesthesiol. 2019; 36:738–44.31. Abu-Omar Y, Mussa S, Anastasiadis K, Steel S, Hands L, Taggart DP. Duplex ultrasonography predicts safety of radial artery harvest in the presence of an abnormal Allen test. Ann Thorac Surg. 2004; 77:116–9.32. Habib J, Baetz L, Satiani B. Assessment of collateral circulation to the hand prior to radial artery harvest. Vasc Med. 2012; 17:352–61.33. Chittick P, Russo V, Sims M, Robinson-Dunn B, Oleszkowicz S, Sawarynski K, et al. An outbreak of Pseudomonas aeruginosa respiratory tract infections associated with intrinsically contaminated ultrasound transmission gel. Infect Control Hosp Epidemiol. 2013; 34:850–3.34. Berk D, Gurkan Y, Kus A, Ulugol H, Solak M, Toker K. Ultrasound-guided radial arterial cannulation: long axis/in-plane versus short axis/out-of-plane approaches? J Clin Monit Comput. 2013; 27:319–24.35. Quan Z, Tian M, Chi P, Cao Y, Li X, Peng K. Modified short-axis out-of-plane ultrasound versus conventional long-axis in-plane ultrasound to guide radial artery cannulation: a randomized controlled trial. Anesth Analg. 2014; 119:163–9.36. Sethi S, Maitra S, Saini V, Samra T, Malhotra SK. Comparison of short-axis out-of-plane versus long-axis in-plane ultrasound-guided radial arterial cannulation in adult patients: a randomized controlled trial. J Anesth. 2017; 31:89–94.37. Song IK, Choi JY, Lee JH, Kim EH, Kim HJ, Kim HS, et al. Short-axis/out-of-plane or long-axis/in-plane ultrasound-guided arterial cannulation in children: a randomised controlled trial. Eur J Anaesthesiol. 2016; 33:522–7.38. Kiberenge RK, Ueda K, Rosauer B. Ultrasound-guided dynamic needle tip positioning technique versus palpation technique for radial arterial cannulation in adult surgical patients: a randomized controlled trial. Anesth Analg. 2018; 126:120–6.39. Liu L, Tan Y, Li S, Tian J. "Modified dynamic needle tip positioning" short-axis, out-of-plane, ultrasound-guided radial artery cannulation in neonates: a randomized controlled trial. Anesth Analg. 2019; 129:178–83.40. Nam K, Jeon Y, Yoon S, Kwon SM, Kang P, Cho YJ, et al. Ultrasound-guided radial artery cannulation using dynamic needle tip positioning versus conventional long-axis in-plane techniques in cardiac surgery patients: a randomized, controlled trial. Minerva Anestesiol. 2020; 86:30–7.41. Quan Z, Zhang L, Zhou C, Chi P, He H, Li Y. Acoustic shadowing facilitates ultrasound-guided radial artery cannulation in young children. Anesthesiology. 2019; 131:1018–24.42. Evans PJ, Kerr JH. Arterial occlusion after cannulation. Br Med J. 1975; 3:197.43. Buetti N, Ruckly S, Lucet JC, Bouadma L, Schwebel C, Mimoz O, et al. Ultrasound guidance and risk for intravascular catheter-related infections among peripheral arterial catheters: a post-hoc analysis of two large randomized-controlled trials. Ann Intensive Care. 2020; 10:89.44. Pancholy SB, Coppola J, Patel T. Subcutaneous administration of nitroglycerin to facilitate radial artery cannulation. Catheter Cardiovasc Interv. 2006; 68:389–91.45. Candemir B, Kumbasar D, Turhan S, Kilickap M, Ozdol C, Akyurek O, et al. Facilitation of radial artery cannulation by periradial subcutaneous administration of nitroglycerin. J Vasc Interv Radiol. 2009; 20:1151–6.46. Ezhumalai B, Satheesh S, Jayaraman B. Effects of subcutaneously infiltrated nitroglycerin on diameter, palpability, ease-of-puncture and pre-cannulation spasm of radial artery during transradial coronary angiography. Indian Heart J. 2014; 66:593–7.47. Chen Y, Ke Z, Xiao J, Lin M, Huang X, Yan C, et al. Subcutaneous injection of nitroglycerin at the radial artery puncture site reduces the risk of early radial artery occlusion after transradial coronary catheterization: a randomized, placebo-controlled clinical trial. Circ Cardiovasc Interv. 2018; 11:e006571.48. Coppola J, Patel T, Kwan T, Sanghvi K, Srivastava S, Shah S, et al. Nitroglycerin, nitroprusside, or both, in preventing radial artery spasm during transradial artery catheterization. J Invasive Cardiol. 2006; 18:155–8.49. Dharma S, Kedev S, Patel T, Kiemeneij F, Gilchrist IC. A novel approach to reduce radial artery occlusion after transradial catheterization: postprocedural/prehemostasis intra-arterial nitroglycerin. Catheter Cardiovasc Interv. 2015; 85:818–25.50. Majure DT, Hallaux M, Yeghiazarians Y, Boyle AJ. Topical nitroglycerin and lidocaine locally vasodilate the radial artery without affecting systemic blood pressure: a dose-finding phase I study. J Crit Care. 2012; 27:532. e9-13.51. Beyer AT, Ng R, Singh A, Zimmet J, Shunk K, Yeghiazarians Y, et al. Topical nitroglycerin and lidocaine to dilate the radial artery prior to transradial cardiac catheterization: a randomized, placebo-controlled, double-blind clinical trial: the PRE-DILATE Study. Int J Cardiol. 2013; 168:2575–8.52. Reusz G, Langer C, Jakab L, Morvay Z. Ultrasound-guided vascular access: the importance of the needle bevel. Can J Anaesth. 2012; 59:499–500.53. Beards SC, Doedens L, Jackson A, Lipman J. A comparison of arterial lines and insertion techniques in critically ill patients. Anaesthesia. 1994; 49:968–73.54. Yildirim V, Ozal E, Cosar A, Bolcal C, Acikel CH, Kiliç S, et al. Direct versus guidewire-assisted pediatric radial artery cannulation technique. J Cardiothorac Vasc Anesth. 2006; 20:48–50.55. Lavallée C, Ayoub C, Mansour A, Lambert J, Lebon JS, Lalu MM, et al. Subclavian and axillary vessel anatomy: a prospective observational ultrasound study. Can J Anaesth. 2018; 65:350–9.56. Melhuish TM, White LD. Optimal wrist positioning for radial arterial cannulation in adults: a systematic review and meta-analysis. Am J Emerg Med. 2016; 34:2372–8.57. Blanco P. Ultrasound-guided vascular cannulation in critical care patients: a practical review. Med Intensiva. 2016; 40:560–71.58. Werner SL, Jones RA, Emerman CL. Effect of hip abduction and external rotation on femoral vein exposure for possible cannulation. J Emerg Med. 2008; 35:73–5.59. Ahn HJ, Lee JW, Yoo SW, Kim JH, Kim KD, Yoo IS, et al. Novel body positioning maximizes femoral venous size in adults: an ultrasonographic evaluation. Hong Kong J Emerg Med. 2018; 25:338–42.60. Dahl MR, Smead WL, McSweeney TD. Radial artery cannulation: a comparison of 15.2- and 4.45-cm catheters. J Clin Monit. 1992; 8:193–7.61. Belda FJ, Aguilar G, Teboul JL, Pestaña D, Redondo FJ, Malbrain M, et al. PICS Investigators Group. Complications related to less-invasive haemodynamic monitoring. Br J Anaesth. 2011; 106:482–6.62. King MA, Garrison MM, Vavilala MS, Zimmerman JJ, Rivara FP. Complications associated with arterial catheterization in children. Pediatr Crit Care Med. 2008; 9:367–71.63. Lipira AB, Mackinnon SE, Fox IK. Axillary arterial catheter use associated with hand ischemia in a multi-trauma patient: case report and literature review. J Clin Anesth. 2011; 23:325–8.64. Scheer B, Perel A, Pfeiffer UJ. Clinical review: complications and risk factors of peripheral arterial catheters used for haemodynamic monitoring in anaesthesia and intensive care medicine. Crit Care. 2002; 6:199–204.65. Baserga MC, Puri A, Sola A. The use of topical nitroglycerin ointment to treat peripheral tissue ischemia secondary to arterial line complications in neonates. J Perinatol. 2002; 22:416–9.66. Cuper NJ, de Graaff JC, Hartman BJ, Verdaasdonk RM, Kalkman CJ. Difficult arterial cannulation in children: is a near-infrared vascular imaging system the answer? Br J Anaesth. 2012; 109:420–6.67. Ho HH, Jafary FH, Ong PJ. Radial artery spasm during transradial cardiac catheterization and percutaneous coronary intervention: incidence, predisposing factors, prevention, and management. Cardiovasc Revasc Med. 2012; 13:193–5.68. Puri VK, Carlson RW, Bander JJ, Weil MH. Complications of vascular catheterization in the critically ill. A prospective study. Crit Care Med. 1980; 8:495–9.69. Wang A, Hendin A, Millington SJ, Koenig S, Eisen LA, Shiloh AL. Better with ultrasound: arterial line placement. Chest. 2020; 157:574–9.70. O'Horo JC, Maki DG, Krupp AE, Safdar N. Arterial catheters as a source of bloodstream infection: a systematic review and meta-analysis. Crit Care Med. 2014; 42:1334–9.71. Hambsch ZJ, Kerfeld MJ, Kirkpatrick DR, McEntire DM, Reisbig MD, Youngblood CF, et al. Arterial catheterization and infection: toll-like receptors in defense against microorganisms and therapeutic implications. Clin Transl Sci. 2015; 8:857–70.72. Safdar N, O'Horo JC, Maki DG. Arterial catheter-related bloodstream infection: incidence, pathogenesis, risk factors and prevention. J Hosp Infect. 2013; 85:189–95.73. Kuo F, Park J, Chow K, Chen A, Walsworth MK. Avoiding peripheral nerve injury in arterial interventions. Diagn Interv Radiol. 2019; 25:380–91.74. Rubinos C, Ruland S. Neurologic complications in the intensive care unit. Curr Neurol Neurosci Rep. 2016; 16:57.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inadvertent Arterial Catheterization of Central Venous Catheter: A Case Report
- Internal jugular vein thrombosis detection by ultrasound scan after failure of internal jugular vein catheterization: A case report
- Internal Jugular Vein Thrombosis Detected during Ultrasound-guided Cannulation in Children: A case report
- Ultrasound-Guided Subclavian Vein Catheterization
- Real-time ultrasound guided thoracic epidural catheterization: a technical review