Yeungnam Univ J Med.
2021 Apr;38(2):136-141. 10.12701/yujm.2020.00542.
Analysis of the risk factors of acute kidney injury after total hip or knee replacement surgery
- Affiliations
-
- 1Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2515187
- DOI: http://doi.org/10.12701/yujm.2020.00542
Abstract
- Background
Postoperative acute kidney injury (AKI), which increases the risk of postoperative morbidity and mortality, poses a major concern to surgeons. We conducted this study to analyze the risk factors associated with the occurrence of AKI after orthopedic surgery.
Methods
This was a retrospective study that included 351 patients who underwent total hip or knee replacement surgery at Inje University Haeundae Paik Hospital between January 2012 and December 2016.
Results
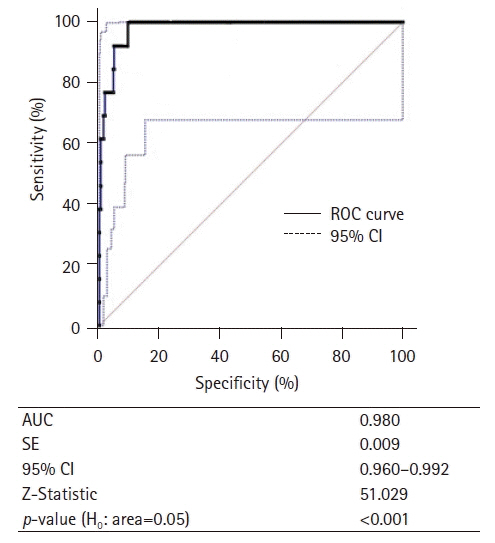
AKI occurred in 13 (3.7%) of the 351 patients. The patients’ preoperative estimated glomerular filtration rate (eGFR) was 66.66±34.02 mL/min/1.73 m2 in the AKI group and 78.07±21.23 mL/min/1.73 m2 in the non-AKI group. The hemoglobin levels were 11.21±1.65 g/dL in the AKI group and 12.39±1.52 g/dL in the non-AKI group. Hemoglobin level was related to increased risk of AKI (odds ratio [OR], 0.13; 95% confidence interval [CI], 0.02–0.68; p=0.016). Administration of crystalloid or colloid fluid alone and the perioperative amount of fluid did not show any significant relationship with AKI. Further analysis of the changes in eGFR was performed using a cutoff value of 7.54. The changes in eGFR were significantly related to decreased risk of AKI (OR, 0.74; 95% CI, 0.61–0.89; p=0.002).
Conclusion
Renal function should be monitored closely after orthopedic surgery if patients have chronic kidney disease and low hemoglobin level. Predicting the likelihood of AKI occurrence, early treatment of high-risk patients, and monitoring perioperative laboratory test results, including eGFR, will help improve patient prognosis.
Figure
Reference
-
References
1. Chertow GM, Levy EM, Hammermeister KE, Grover F, Daley J. Independent association between acute renal failure and mortality following cardiac surgery. Am J Med. 1998; 104:343–8.2. Biteker M, Dayan A, Tekkeşin AI, Can MM, Taycı I, Ilhan E, et al. Incidence, risk factors, and outcomes of perioperative acute kidney injury in noncardiac and nonvascular surgery. Am J Surg. 2014; 207:53–9.
Article3. White SM, Rashid N, Chakladar A. An analysis of renal dysfunction in 1511 patients with fractured neck of femur: the implications for peri-operative analgesia. Anaesthesia. 2009; 64:1061–5.
Article4. Paul A, John B, Pawar B, Sadiq S. Renal profile in patients with orthopaedic trauma: a prospective study. Acta Orthop Belg. 2009; 75:528–32.5. Hobson C, Ozrazgat-Baslanti T, Kuxhausen A, Thottakkara P, Efron PA, Moore FA, et al. Cost and mortality associated with postoperative acute kidney injury. Ann Surg. 2015; 261:1207–14.
Article6. Rosner MH, Okusa MD. Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol. 2006; 1:19–32.
Article7. Yoshihara H, Yoneoka D. Trends in the incidence and in-hospital outcomes of elective major orthopaedic surgery in patients eighty years of age and older in the United States from 2000 to 2009. J Bone Joint Surg Am. 2014; 96:1185–91.
Article8. Statistics Korea. Population projections for Korea: 2017–2067 (based on the 2017 population census) [Internet]. Daejeon: Statistics Korea;2019. [cited 2020 Jul 1]. http://kosis.kr/publication/publicationThema.do?pubcode=PJ.9. Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int Suppl. 2012; 2:1–138.10. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013; 3:1–150.11. Scottish Arthroplasty Project. Biennial report 2014. Edinburgh: NHS National Services Scotland;2014.12. Thakar CV. Perioperative acute kidney injury. Adv Chronic Kidney Dis. 2013; 20:67–75.
Article13. Sun LY, Wijeysundera DN, Tait GA, Beattie WS. Association of intraoperative hypotension with acute kidney injury after elective noncardiac surgery. Anesthesiology. 2015; 123:515–23.
Article14. Lim SY, Lee JY, Yang JH, Na YJ, Kim MG, Jo SK, et al. Predictive factors of acute kidney injury in patients undergoing rectal surgery. Kidney Res Clin Pract. 2016; 35:160–4.
Article15. Bayer O, Reinhart K, Sakr Y, Kabisch B, Kohl M, Riedemann NC, et al. Renal effects of synthetic colloids and crystalloids in patients with severe sepsis: a prospective sequential comparison. Crit Care Med. 2011; 39:1335–42.
Article16. Levey AS, Eckardt KU, Tsukamoto Y, Levin A, Coresh J, Rossert J, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int. 2005; 67:2089–100.
Article17. Odden MC, Shlipak MG, Tager IB. Serum creatinine and functional limitation in elderly persons. J Gerontol A Biol Sci Med Sci. 2009; 64:370–6.
Article18. Slankamenac K, Beck-Schimmer B, Breitenstein S, Puhan MA, Clavien PA. Novel prediction score including pre- and intraoperative parameters best predicts acute kidney injury after liver surgery. World J Surg. 2013; 37:2618–28.
Article19. Bell S, Dekker FW, Vadiveloo T, Marwick C, Deshmukh H, Donnan PT, et al. Risk of postoperative acute kidney injury in patients undergoing orthopaedic surgery: development and validation of a risk score and effect of acute kidney injury on survival: observational cohort study. BMJ. 2015; 351:h5639.