Brain Tumor Res Treat.
2021 Apr;9(1):35-39. 10.14791/btrt.2021.9.e1.
Neuromyelitis Optica Spectrum Disorders Mimicking Multiple Brain Tumors
- Affiliations
-
- 1Department of Neurosurgery, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, Korea
- KMID: 2515081
- DOI: http://doi.org/10.14791/btrt.2021.9.e1
Abstract
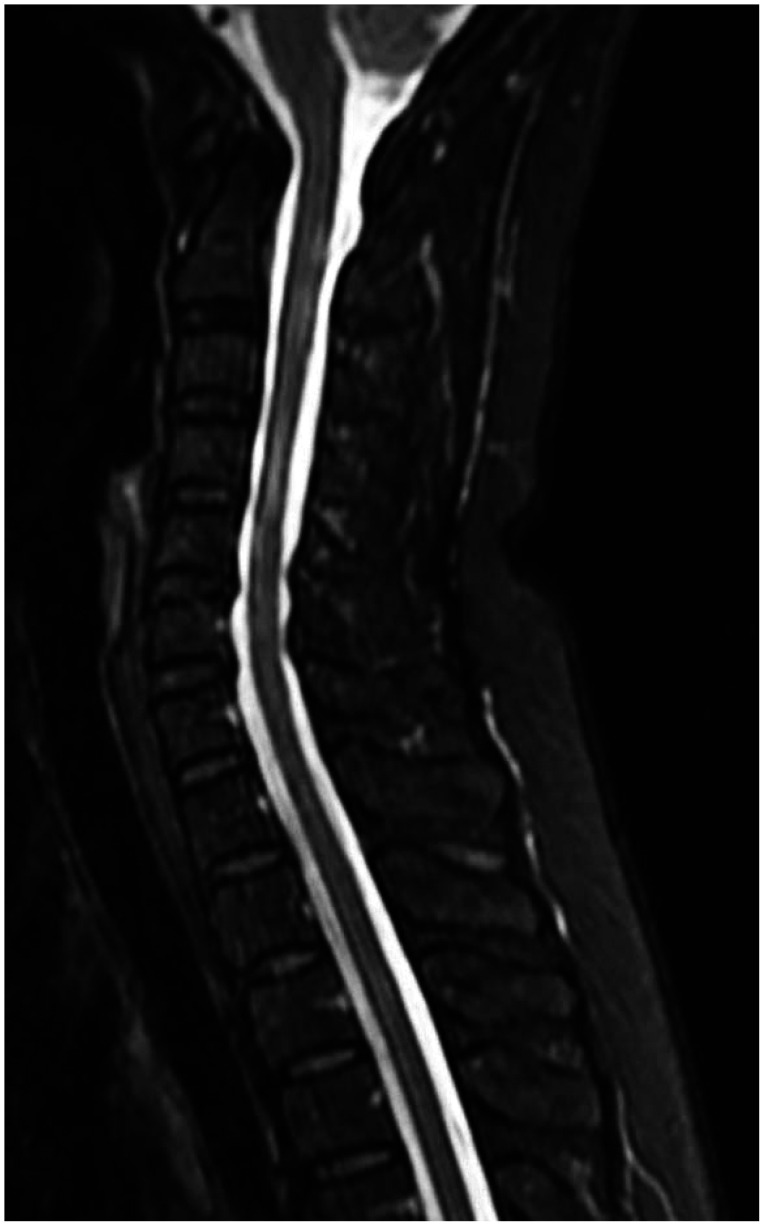
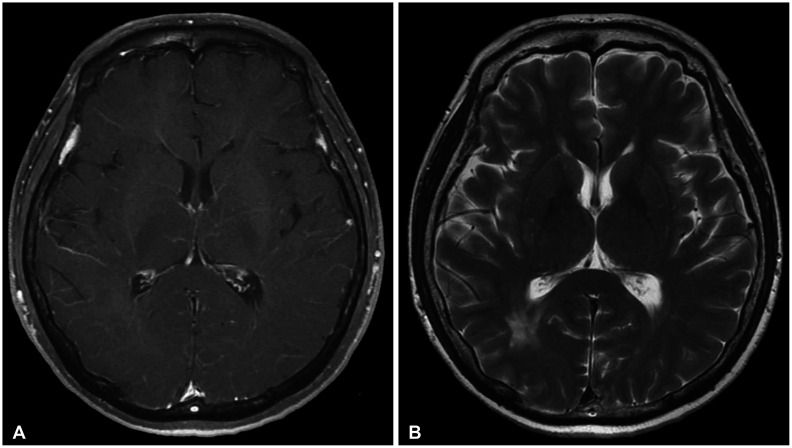
- We report a rare case of neuromyelitis optica spectrum disorders (NMOSD), mimicking multiple brain tumors. A 53-year-old woman presented with weakness and paresthesia in her right arm and leg. Upon admission, brain MRI showed about 10 multiple brain tumors, which had to be differentiated from multiple brain metastases, lymphoma, and high-grade glioma in both hemispheres. No primary cancer was found in the chest-abdomen-pelvis CT. Subsequent spine MRI revealed multifocal cord signal change involving C2-T7, suggesting myelitis. A decrease in visual acuity was noted when taking a medical history, and optic neuritis was diagnosed upon ophthalmologic examination. With clinical and radiological appearances, multiple brain and spinal cord lesions have been diagnosed as NMOSD. Steroid and immunosuppressive drugs were administered. We should consider the possibility of an autoimmune disease, such as NMOSD, involving the optic nerve, spinal cord, and central nervous system when multiple hemispheric tumefactive lesions are observed.
Figure
Reference
-
1. Wingerchuk DM, Lennon VA, Pittock SJ, Lucchinetti CF, Weinshenker BG. Revised diagnostic criteria for neuromyelitis optica. Neurology. 2006; 66:1485–1489. PMID: 16717206.2. Wingerchuk DM, Banwell B, Bennett JL, et al. International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology. 2015; 85:177–189. PMID: 26092914.3. Mandler RN. Neuromyelitis optica - Devic’s syndrome, update. Autoimmun Rev. 2006; 5:537–543. PMID: 17027889.4. Bruscolini A, Sacchetti M, La Cava M, et al. Diagnosis and management of neuromyelitis optica spectrum disorders-an update. Autoimmun Rev. 2018; 17:195–200. PMID: 29339316.5. Juryńczyk M, Craner M, Palace J. Overlapping CNS inflammatory diseases: differentiating features of NMO and MS. J Neurol Neurosurg Psychiatry. 2015; 86:20–25. PMID: 25248365.6. Kim HJ, Paul F, Lana-Peixoto MA, et al. MRI characteristics of neuromyelitis optica spectrum disorder: an international update. Neurology. 2015; 84:1165–1173. PMID: 25695963.7. Kister I, Herbert J, Zhou Y, Ge Y. Ultrahigh-field MR (7 T) imaging of brain lesions in neuromyelitis optica. Mult Scler Int. 2013; 2013:398259. PMID: 23431447.8. Sahraian MA, Radue EW, Minagar A. Neuromyelitis optica: clinical manifestations and neuroimaging features. Neurol Clin. 2013; 31:139–152. PMID: 23186898.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postpartum Relapse of Neuromyelitis Optica Spectrum Disorder after a Long Period of Spontaneous Remission
- Narcolepsy Followed by Intractable Vomiting Caused by Recurrent Brain Involvement in Neuromyelitis Optica Spectrum Disorder
- Differential Diagnosis between Multiple Sclerosis and Neuromyelitis Optica Spectrum Disorder
- Late-onset Seronegative Neuromyelitis Optica Spectrum Disorder Mimicking Wernicke Encephalopathy
- Central Hyperthemia Treated with Bromocriptine in a Patient with Aquaporin 4 Antibody Positive Neuromyelitis Optica Spectrum Disorder