Ann Surg Treat Res.
2021 Apr;100(4):228-234. 10.4174/astr.2021.100.4.228.
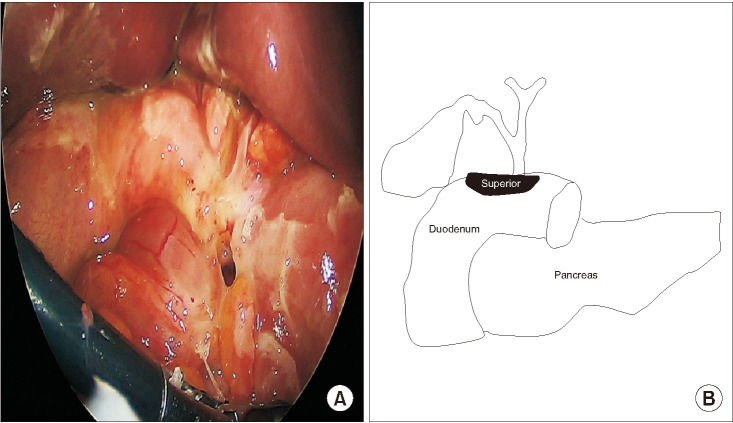
Perforation on the superior side of duodenum is a risk factor of laparoscopic primary repair for duodenal ulcer perforation
- Affiliations
-
- 1Department of Surgery, Hanyang University Guri Hospital, Hanyang University School of Medicine, Guri, Korea
- 2Department of Anesthesiology, Hanyang University Guri Hospital, Hanyang University School of Medicine, Guri, Korea
- KMID: 2514720
- DOI: http://doi.org/10.4174/astr.2021.100.4.228
Abstract
- Purpose
Primary repair is the standard surgical method for treating duodenal ulcer perforations, with very good results usually anticipated because of the simplicity of the associated surgical techniques. Therefore, this study aimed to analyze the risk factors that affect laparoscopic primary repair outcomes for duodenal ulcer perforation.
Methods
Between June 2010 and June 2020, 124 patients who underwent laparoscopic primary repair for duodenal ulcer perforations were reviewed. Early surgical outcomes were evaluated and risk factors for postoperative complications were assessed.
Results
All surgeries were performed laparoscopically without open conversion. Multivariate analysis showed that the elderly (over 70 years), and perforations that needed more than 2 stitches for closure were risk factors for overall postoperative complications. Perforations that needed more than 2 stitches and perforations on the superior side of the duodenum were major risk factors for severe postoperative complications. Severe postoperative complications occurred in 6 of the patients, and 1 of them died of multiorgan failure.
Conclusion
Based on our results, we suggest that laparoscopic primary repair can be safely performed in duodenal ulcer perforation. However, more careful surgery and postoperative care are needed to improve the surgical outcomes of patients who need more than 2 stitches to close their perforation or who have perforations on the superior side of the duodenum.
Figure
Reference
-
1. Bertleff MJ, Lange JF. Perforated peptic ulcer disease: a review of history and treatment. Dig Surg. 2010; 27:161–169. PMID: 20571260.
Article2. Møller MH, Shah K, Bendix J, Jensen AG, Zimmermann-Nielsen E, Adamsen S, et al. Risk factors in patients surgically treated for peptic ulcer perforation. Scand J Gastroenterol. 2009; 44:145–152. PMID: 18785067.
Article3. Boey J, Choi SK, Poon A, Alagaratnam TT. Risk stratification in perforated duodenal ulcers: a prospective validation of predictive factors. Ann Surg. 1987; 205:22–26. PMID: 3800459.4. Townsend CM Jr, Beauchamp RD, Evers BM, Mattox KL. Sabiston textbook of surgery: the biological basis of modern surgical practice. 20th ed. Philadelphia (PA): Elsevier Saunders;2017.5. Siu WT, Leong HT, Law BK, Chau CH, Li AC, Fung KH, et al. Laparoscopic repair for perforated peptic ulcer: a randomized controlled trial. Ann Surg. 2002; 235:313–319. PMID: 11882751.6. Bertleff MJ, Halm JA, Bemelman WA, van der Ham AC, van der Harst E, Oei HI, et al. Randomized clinical trial of laparoscopic versus open repair of the perforated peptic ulcer: the LAMA Trial. World J Surg. 2009; 33:1368–1373. PMID: 19430829.
Article7. Kim MG. Laparoscopic surgery for perforated duodenal ulcer disease: analysis of 70 consecutive cases from a single surgeon. Surg Laparosc Endosc Percutan Tech. 2015; 25:331–336. PMID: 25799260.8. Lee FY, Leung KL, Lai PB, Lau JW. Selection of patients for laparoscopic repair of perforated peptic ulcer. Br J Surg. 2001; 88:133–136. PMID: 11136326.
Article9. Lunevicius R, Morkevicius M. Systematic review comparing laparoscopic and open repair for perforated peptic ulcer. Br J Surg. 2005; 92:1195–1207. PMID: 16175515.
Article10. Lau H. Laparoscopic repair of perforated peptic ulcer: a meta-analysis. Surg Endosc. 2004; 18:1013–1021. PMID: 15136924.
Article11. Lau WY, Leung KL, Kwong KH, Davey IC, Robertson C, Dawson JJ, et al. A randomized study comparing laparoscopic versus open repair of perforated peptic ulcer using suture or sutureless technique. Ann Surg. 1996; 224:131–138. PMID: 8757375.
Article12. Matsuda M, Nishiyama M, Hanai T, Saeki S, Watanabe T. Laparoscopic omental patch repair for perforated peptic ulcer. Ann Surg. 1995; 221:236–240. PMID: 7717776.
Article13. Michelet I, Agresta F. Perforated peptic ulcer: laparoscopic approach. Eur J Surg. 2000; 166:405–408. PMID: 10881954.14. Siu WT, Chau CH, Law BK, Tang CN, Ha PY, Li MK. Routine use of laparoscopic repair for perforated peptic ulcer. Br J Surg. 2004; 91:481–484. PMID: 15048752.
Article15. Kim HS, Lee JH, Kim MG. Outcomes of laparoscopic primary gastrectomy with curative intent for gastric perforation: experience from a single surgeon. Surg Endosc;2020. 8. 28. [Epub]. . DOI: 10.1007/s00464-020-07902-z.16. Lee HH, Son SY, Lee JH, Kim MG, Hur H, Park DJ. Surgeon's experience overrides the effect of hospital volume for postoperative outcomes of laparoscopic surgery in gastric cancer: multi-institutional study. Ann Surg Oncol. 2017; 24:1010–1017. PMID: 27834031.
Article17. Kim MG, Kim KC, Yook JH, Kim BS, Kim TH, Kim BS. A practical way to overcome the learning period of laparoscopic gastrectomy for gastric cancer. Surg Endosc. 2011; 25:3838–3844. PMID: 21656323.
Article18. Ma CH, Kim MG. Laparoscopic primary repair with omentopexy for duodenal ulcer perforation: a single institution experience of 21 cases. J Gastric Cancer. 2012; 12:237–242. PMID: 23346496.
Article19. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.20. Clavien PA, Strasberg SM. Severity grading of surgical complications. Ann Surg. 2009; 250:197–198. PMID: 19638901.
Article21. Sharma SS, Mamtani MR, Sharma MS, Kulkarni H. A prospective cohort study of postoperative complications in the management of perforated peptic ulcer. BMC Surg. 2006; 6:8. PMID: 16780583.
Article22. Hermansson M, Staël von Holstein C, Zilling T. Surgical approach and prognostic factors after peptic ulcer perforation. Eur J Surg. 1999; 165:566–572. PMID: 10433141.23. Blomgren LG. Perforated peptic ulcer: long-term results after simple closure in the elderly. World J Surg. 1997; 21:412–415. PMID: 9143574.
Article24. Kim JH, Chin HM, Bae YJ, Jun KH. Risk factors associated with conversion of laparoscopic simple closure in perforated duodenal ulcer. Int J Surg. 2015; 15:40–44. PMID: 25644542.
Article25. Abd Ellatif ME, Salama AF, Elezaby AF, El-Kaffas HF, Hassan A, Magdy A, et al. Laparoscopic repair of perforated peptic ulcer: patch versus simple closure. Int J Surg. 2013; 11:948–951. PMID: 23806652.
Article26. Sartelli M, Viale P, Catena F, Ansaloni L, Moore E, Malangoni M, et al. 2013 WSES guidelines for management of intraabdominal infections. World J Emerg Surg. 2013; 8:3. PMID: 23294512.27. Sauerland S, Agresta F, Bergamaschi R, Borzellino G, Budzynski A, Champault G, et al. Laparoscopy for abdominal emergencies: evidence-based guidelines of the European Association for Endoscopic Surgery. Surg Endosc. 2006; 20:14–29. PMID: 16247571.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopic Primary Repair with Omentopexy for Duodenal Ulcer Perforation: A Single Institution Experience of 21 Cases
- Conservative Management of a Duodenal Perforation after Trauma
- Two Cases of Successful ERCP during ERCP-Related Iatrogenic Duodenal Perforation
- Endoscopic Treatments of Endoscopic Retrograde Cholangiopancreatography-Related Duodenal Perforations
- A Study of Conservative Management for Peptic Ulcer Perforation