Anat Cell Biol.
2021 Mar;54(1):132-135. 10.5115/acb.20.241.
Novel bilateral bifurcation of the coronary vasculature
- Affiliations
-
- 1Clinical Anatomy Learning Centre, Lancaster Medical School, Faculty of Health and Medicine, Lancaster University, Lancaster, United Kingdom
- 2Royal Preston Hospital, Fulwood, United Kingdom
- 3Department of Anatomy, School of Medicine, University of Namibia, Windhoek, Namibia
- KMID: 2514594
- DOI: http://doi.org/10.5115/acb.20.241
Abstract
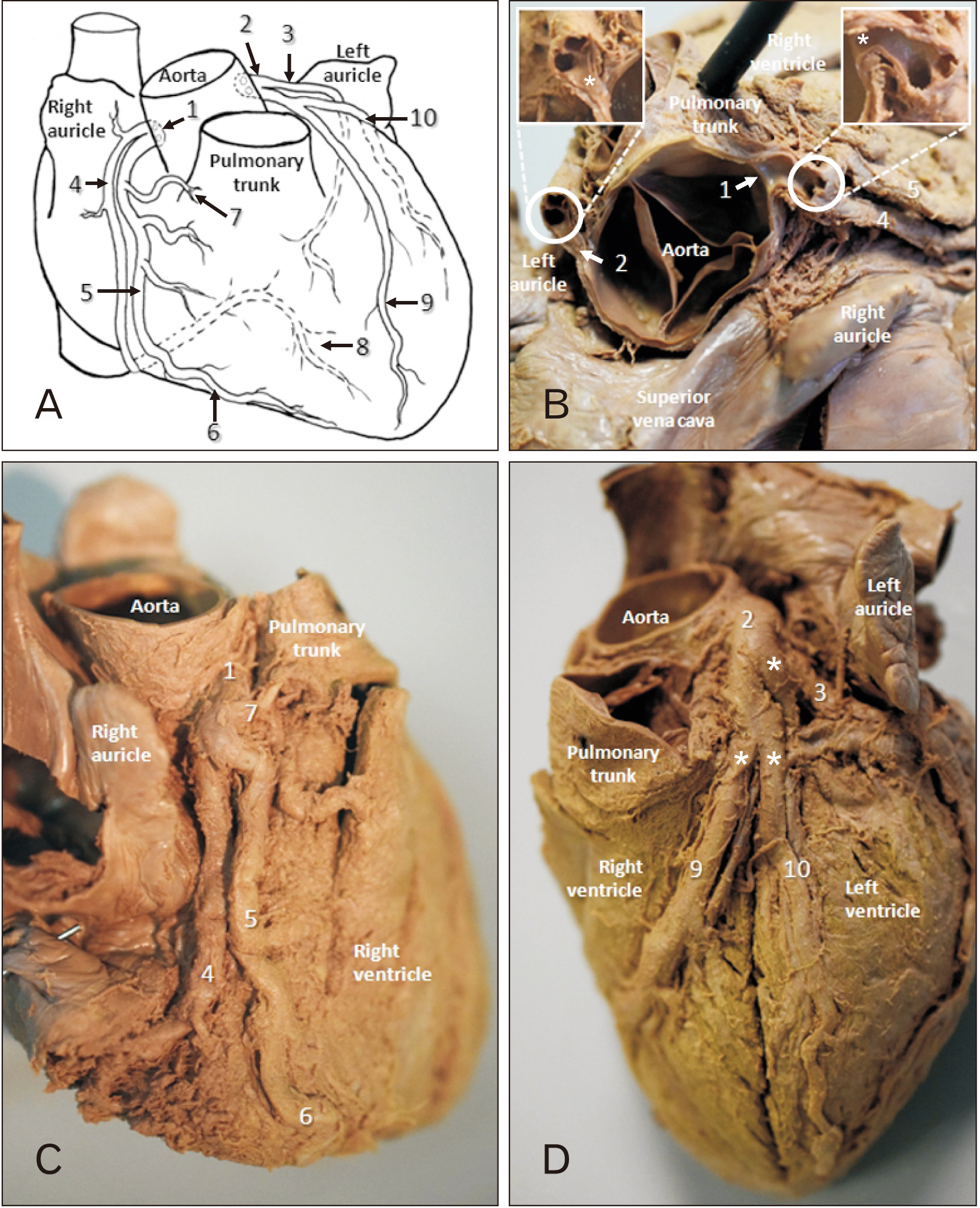
- Multiple variants and anomalies in the coronary vasculature have been reported. Some variants, particularly those with duplication, can be advantageous, many are insignificant and some are ultimately lethal. Many of these variants and anomalies are not identified until imaged or post-mortem. A novel bilateral bifid variation of the coronary arteries was observed in 49-year-old male cadaver. The respective origins were associated with the left and right aortic cusps from single ostia. Immediate bifurcation followed on either side. A right sided accessory branch supplied the pulmonary trunk and right ventricle. A more standard branch continued to form the posterior interventricular artery. The left sided variation demonstrated a solitary circumflex artery (towards the posterior interventricular septum) and, left marginal and anterior interventricular branches shortly after bifurcation. This case may be beneficial in surviving adverse cardiac events, particularly those associated with lifestyle. They also present a ‘double’ challenge for clinicians.
Keyword
Figure
Reference
-
References
1. Quinn T. Barrett D, Gretton M, Quinn T, editors. 2006. The history of cardiac care. Cardiac Care: An Introduction for Healthcare Professionals. John Wiley & Sons;Chichester: p. 10–8.2. Nayak SB. 2018; Trifurcation of right coronary artery and its huge right ventricular branch: can it be hazardous? Anat Cell Biol. 51:139–41. DOI: 10.5115/acb.2018.51.2.139. PMID: 29984060. PMCID: PMC6026817.
Article3. Prakken NH, Cramer MJ, Olimulder MA, Agostoni P, Mali WP, Velthuis BK. 2010; Screening for proximal coronary artery anomalies with 3-dimensional MR coronary angiography. Int J Cardiovasc Imaging. 26:701–10. DOI: 10.1007/s10554-010-9617-0. PMID: 20339919. PMCID: PMC2898111.
Article4. Pejković B, Krajnc I, Anderhuber F. 2008; Anatomical variations of coronary ostia, aortocoronary angles and angles of division of the left coronary artery of the human heart. J Int Med Res. 36:914–22. DOI: 10.1177/147323000803600507. PMID: 18831884.
Article5. Waller BF. 1983; Five coronary ostia: duplicate left anterior descending and right conus coronary arteries. Am J Cardiol. 51:1562. DOI: 10.1016/0002-9149(83)90680-X. PMID: 6846193.
Article6. Villa AD, Sammut E, Nair A, Rajani R, Bonamini R, Chiribiri A. 2016; Coronary artery anomalies overview: the normal and the abnormal. World J Radiol. 8:537–55. DOI: 10.4329/wjr.v8.i6.537. PMID: 27358682. PMCID: PMC4919754.
Article7. Basso C, Thiene G. 2005; Congenital coronary artery anomalies at risk of myocardial ischaemia and sudden death. Eur Cardiol. 1:1–5. DOI: 10.15420/ECR.2005.1i.
Article8. Gräni C, Kaufmann PA, Windecker S, Buechel RR. 2019; Diagnosis and management of anomalous coronary arteries with a malignant course. Interv Cardiol. 14:83–8. DOI: 10.15420/icr.2019.1.1. PMID: 31178934. PMCID: PMC6545977.
Article9. Illes J, Moser MA, McCormick JB, Racine E, Blakeslee S, Caplan A, Hayden EC, Ingram J, Lohwater T, McKnight P, Nicholson C, Phillips A, Sauvé KD, Snell E, Weiss S. 2010; Neurotalk: improving the communication of neuroscience research. Nat Rev Neurosci. 11:61–9. DOI: 10.1038/nrn2773. PMID: 19953102. PMCID: PMC2818800.
Article10. Frescura C, Basso C, Thiene G, Corrado D, Pennelli T, Angelini A, Daliento L. 1998; Anomalous origin of coronary arteries and risk of sudden death: a study based on an autopsy population of congenital heart disease. Hum Pathol. 29:689–95. DOI: 10.1016/S0046-8177(98)90277-5. PMID: 9670825.
Article11. Rahalkar AM, Rahalkar MD. 2009; Pictorial essay: coronary artery variants and anomalies. Indian J Radiol Imaging. 19:49–53. DOI: 10.4103/0971-3026.45345. PMID: 19774140. PMCID: PMC2747404.
Article12. Rama Krishnan RS, Marwah VV, Gupta T, Kalyanpur A. 2008; Images: malignant right coronary artery- 64-slice CTA. Indian J Radiol Imaging. 18:126–7. DOI: 10.4103/0971-3026.40293. PMCID: PMC2768624.13. Risse M, Weiler G. 1985; [Coronary muscle bridge and its relations to local coronary sclerosis, regional myocardial ischemia and coronary spasm. A morphometric study]. Z Kardiol. 74:700–5. German. PMID: 4096063.14. Lee MS, Chen CH. 2015; Myocardial bridging: an up-to-date review. J Invasive Cardiol. 27:521–8. PMID: 25999138. PMCID: PMC4818117.15. Sari I, Kizilkan N, Sucu M, Davutoglu V, Ozer O, Soydinc S, Aksoy M. 2008; Double right coronary artery: report of two cases and review of the literature. Int J Cardiol. 130:e74–7. DOI: 10.1016/j.ijcard.2007.11.073. PMID: 18207256.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Gender Is Not Predictor for Clinical Outcomes in Patients Undergoing Percutaneous Coronary Intervention for Coronary Bifurcation
- Understanding the Coronary Bifurcation Stenting
- A Case of Bilateral Coronary Artery-Pulmonary Artery Fistula
- Angioplasty at Coronary Bifurcation
- Coronary Angiographic Findings of Left Atrial Thrombi in Mitral Stenosis