J Liver Cancer.
2021 Mar;21(1):87-91. 10.17998/jlc.21.1.87.
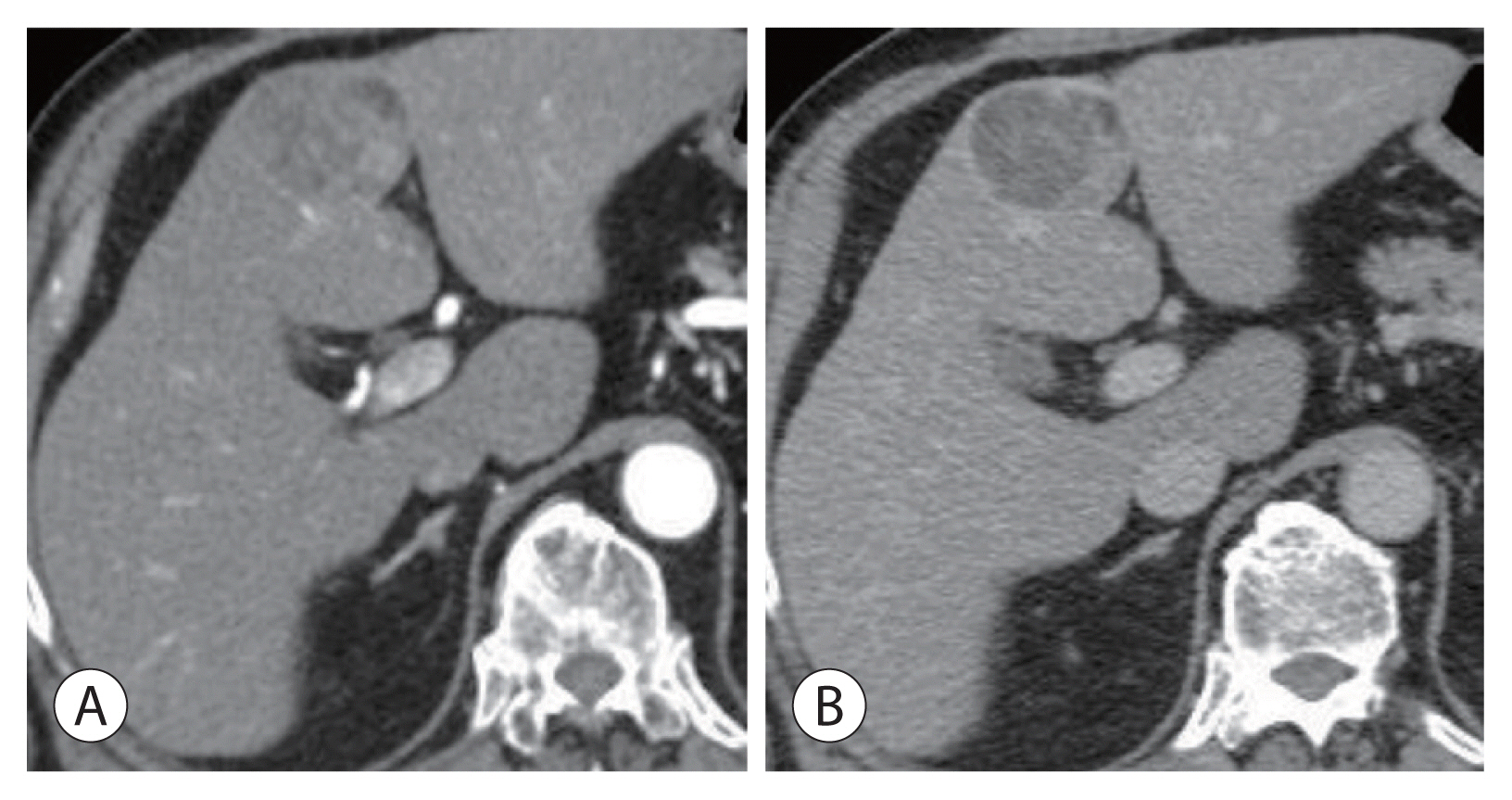
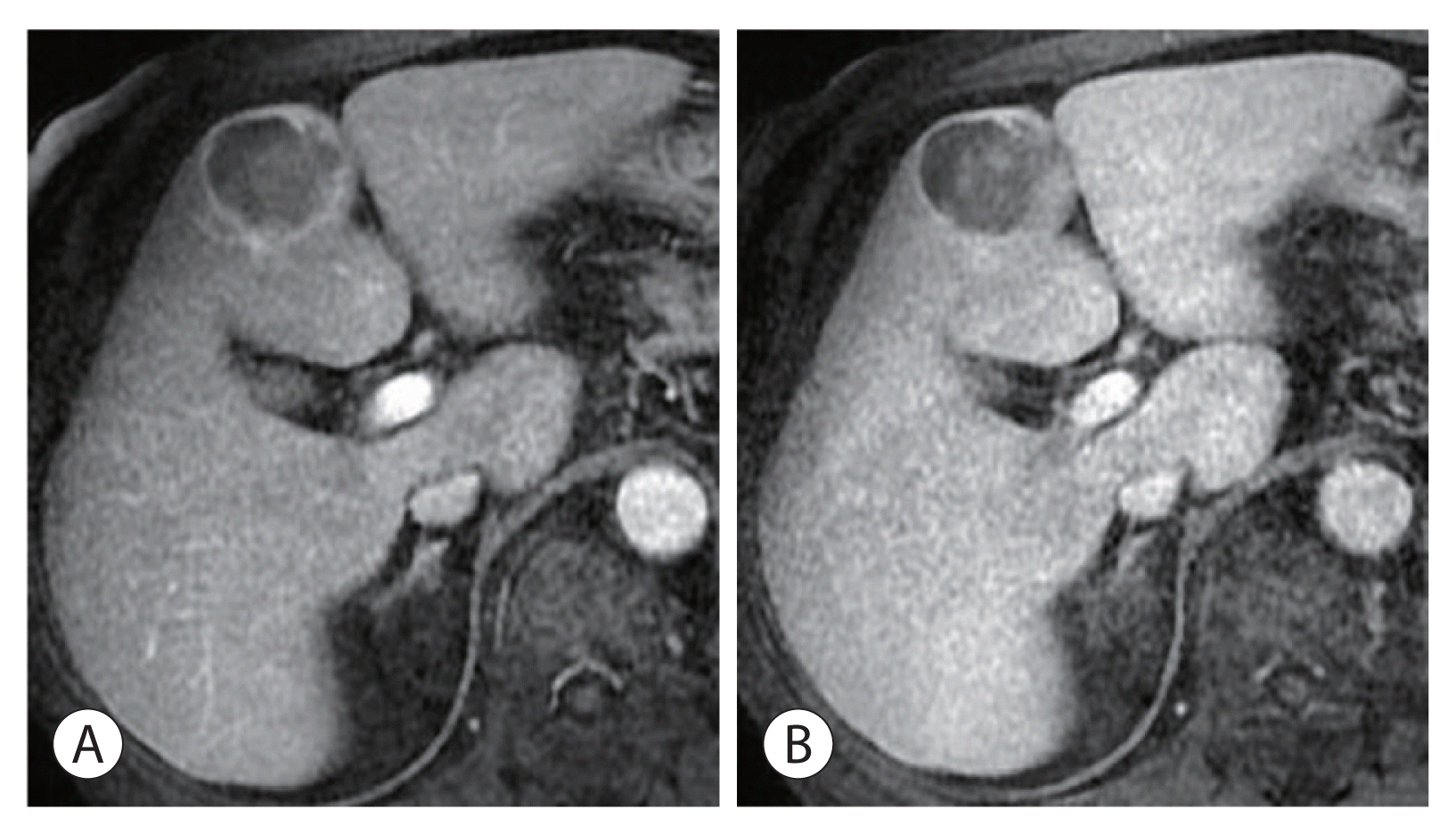
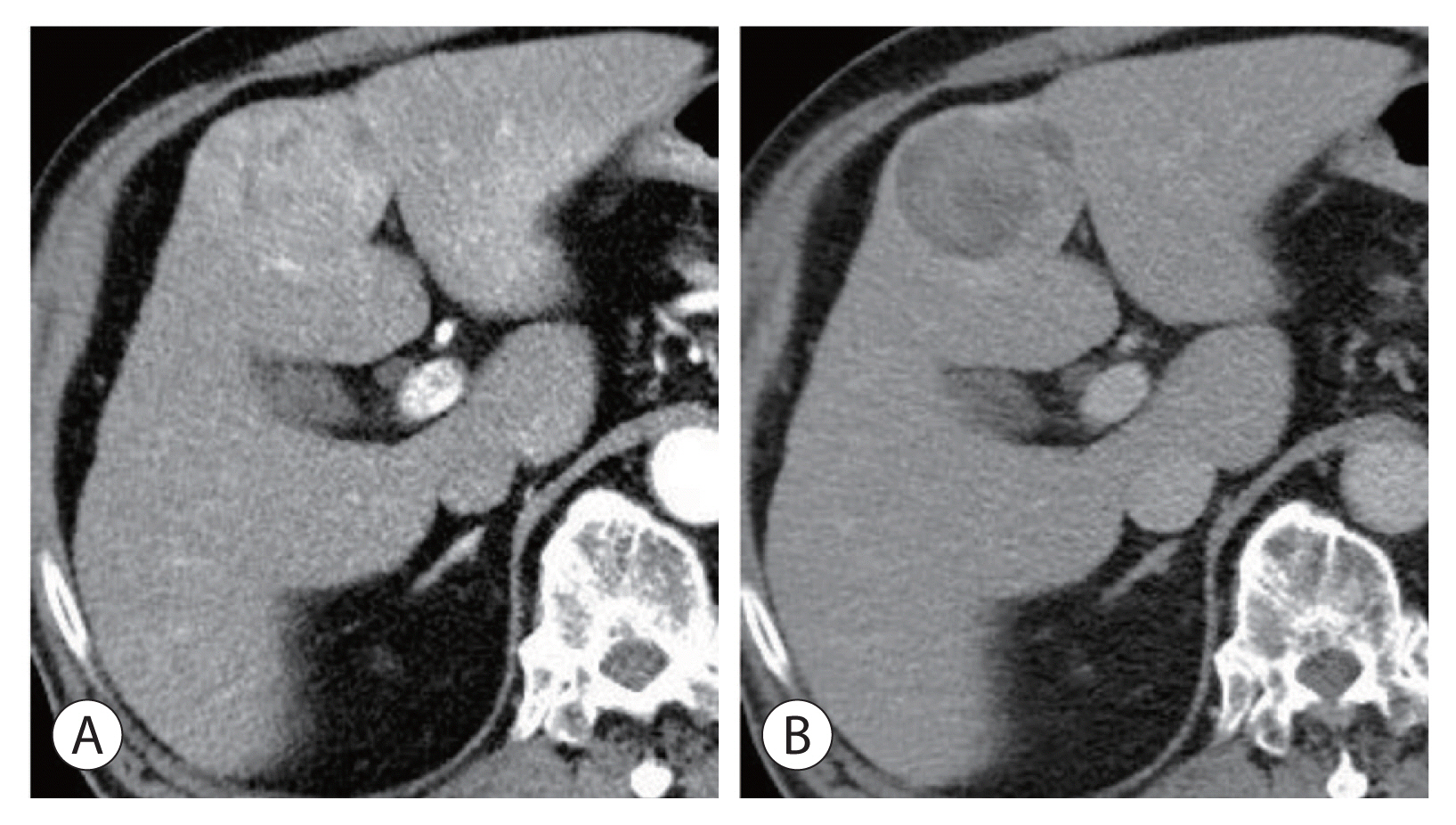
Hepatocellular Carcinoma Arising from Hepatocellular Adenoma in an Elderly Male Patient
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2514239
- DOI: http://doi.org/10.17998/jlc.21.1.87
Abstract
- Hepatocellular adenoma is a benign tumor of the liver occurring predominantly in young women taking oral contraceptives. The malignant transformation of hepatocellular adenoma into hepatocellular carcinoma has rarely been reported. Herein, we report the case of an elderly male patient with hepatocellular carcinoma that developed from hepatocellular adenoma. The patient’s high risk for surgery and conflicting biopsy and imaging results made it difficult to determine the treatment direction. Eventually, the mass was completely removed by laparoscopic left hemi-hepatectomy without complications.
Figure
Reference
-
1. Baum JK, Bookstein JJ, Holtz F, Klein EW. Possible association between benign hepatomas and oral contraceptives. Lancet. 1973; 2:926–929.2. Nault JC, Bioulac-Sage P, Zucman-Rossi J. Hepatocellular benign tumors-from molecular classification to personalized clinical care. Gastroenterology. 2013; 144:888–902.3. Belghiti J, Cauchy F, Paradis V, Vilgrain V. Diagnosis and management of solid benign liver lesions. Nat Rev Gastroenterol Hepatol. 2014; 11:737–749.4. Yacoub H, Kchir H, Cherif D, Hassine H, Haouet S, Ayari A, et al. Hepatocellular carcinoma arising from hepatic adenoma in a young woman. Clin Case Rep. 2020; 8:1659–1662.5. Sempoux C, Balabaud C, Bioulac-Sage P. Malignant transformation of hepatocellular adenoma. Hepat Oncol. 2014; 1:421–431.6. Farges O, Dokmak S. Malignant transformation of liver adenoma: an analysis of the literature. Dig Surg. 2010; 27:32–38.7. Dokmak S, Paradis V, Vilgrain V, Sauvanet A, Farges O, Valla D, et al. A single-center surgical experience of 122 patients with single and multiple hepatocellular adenomas. Gastroenterology. 2009; 137:1698–1705.8. Choe MS, Yu ES. Hepatocellular carcinoma arising in hepatocellular adenoma. Taehan Kan Hakhoe Chi. 2002; 8:107–109.9. Kim DH, Kim SU, Nam DH, Choi YJ, Park SM, Lee CK, et al. A case of hepatocellular carcinoma within hepatocellular adenoma in a non-cirrhotic male. Korean J Intern Med. 2009; 24:147–152.10. Burri E, Steuerwald M, Cathomas G, Mentha G, Majno P, Rubbia-Brandt L, et al. Hepatocellular carcinoma in a liver-cell adenoma within a non-cirrhotic liver. Eur J Gastroenterol Hepatol. 2006; 18:437–441.11. Grazioli L, Federle MP, Brancatelli G, Ichikawa T, Olivetti L, Blachar A. Hepatic adenomas: imaging and pathologic findings. Radiographics. 2001; 21:877–892.12. Nault JC, Paradis V, Cherqui D, Vilgrain V, Zucman-Rossi J. Molecular classification of hepatocellular adenoma in clinical practice. J Hepatol. 2017; 67:1074–1083.13. Monga SP. Beta-catenin signaling and roles in liver homeostasis, injury, and tumorigenesis. Gastroenterology. 2015; 148:1294–1310.14. Zucman-Rossi J, Jeannot E, Nhieu JT, Scoazec JY, Guettier C, Rebouissou S, et al. Genotype-phenotype correlation in hepatocellular adenoma: new classification and relationship with HCC. Hepatology. 2006; 43:515–524.15. Dhingra S, Fiel MI. Update on the new classification of hepatic adenomas: clinical, molecular, and pathologic characteristics. Arch Pathol Lab Med. 2014; 138:1090–1097.16. Bioulac-Sage P, Rebouissou S, Thomas C, Blanc JF, Saric J, Sa Cunha A, et al. Hepatocellular adenoma subtype classification using molecular markers and immunohistochemistry. Hepatology. 2007; 46:740–748.17. Stoot JH, Coelen RJ, De Jong MC, Dejong CH. Malignant transformation of hepatocellular adenomas into hepatocellular carcinomas: a systematic review including more than 1600 adenoma cases. HPB (Oxford). 2010; 12:509–522.18. Kim Y, Amini N, He J, Margonis GA, Weiss M, Wolfgang CL, et al. National trends in the use of surgery for benign hepatic tumors in the United States. Surgery. 2015; 157:1055–1064.19. Cho W, Kwon CHD, Choi JY, Lee SH, Kim JM, Choi GS, et al. Impact of technical innovation on surgical outcome of laparoscopic major liver resection: 10 years’ experience at a large-volume center. Ann Surg Treat Res. 2019; 96:14–18.20. Landi F, De’ Angelis N, Scatton O, Vidal X, Ayav A, Muscari F, et al. Short-term outcomes of laparoscopic vs. open liver resection for hepatocellular adenoma: a multicenter propensity score adjustment analysis by the AFC-HCA-2013 study group. Surg Endosc. 2017; 31:4136–4144.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hepatocellular Carcinoma Arising in Hepatocellular Adenoma
- Atypical Nodule Arising in a Hepatocellular Adenoma
- Malignant Transformation of Inflammatory Hepatocellular Adenoma into Hepatocellular Carcinoma
- A Case of Hepatocellular Carcinoma Within Hepatocellular Adenoma in a Non-Cirrhotic Male
- Hepatocellular Adenoma and Focal Nodular Hyperplasia