Effect of Sarcopenia and Body Shape on Cardiovascular Disease According to Obesity Phenotypes
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Hallym University College of Medicine, Chuncheon, Korea.
- 2Department of Public Health Science, Graduate School of Public Health, Seoul National University, Seoul, Korea.
- 3Institute of Health and Environment, Seoul National University, Seoul, Korea.
- KMID: 2514197
- DOI: http://doi.org/10.4093/dmj.2019.0223
Abstract
Background This study aimed to assess the effects of sarcopenia and A Body Shape Index (ABSI) on cardiovascular disease (CVD) risk according to obesity phenotypes.
Methods We used data from the National Health and Nutrition Examination Survey 1999 to 2012. A total of 25,270 adults were included and classified into the following groups: metabolically healthy normal weight (MHNW), metabolically healthy overweight/obese (MHO), metabolically unhealthy normal weight (MUNW), and metabolically unhealthy overweight/obese (MUO). Sarcopenia was defined as the appendicular skeletal mass index <7 kg/m2 in men and <5.5kg/m2 in women. A multivariate logistic regression analysis was performed to evaluate the odds ratio (OR) of sarcopenia and ABSI for CVD events according to the obesity phenotype.
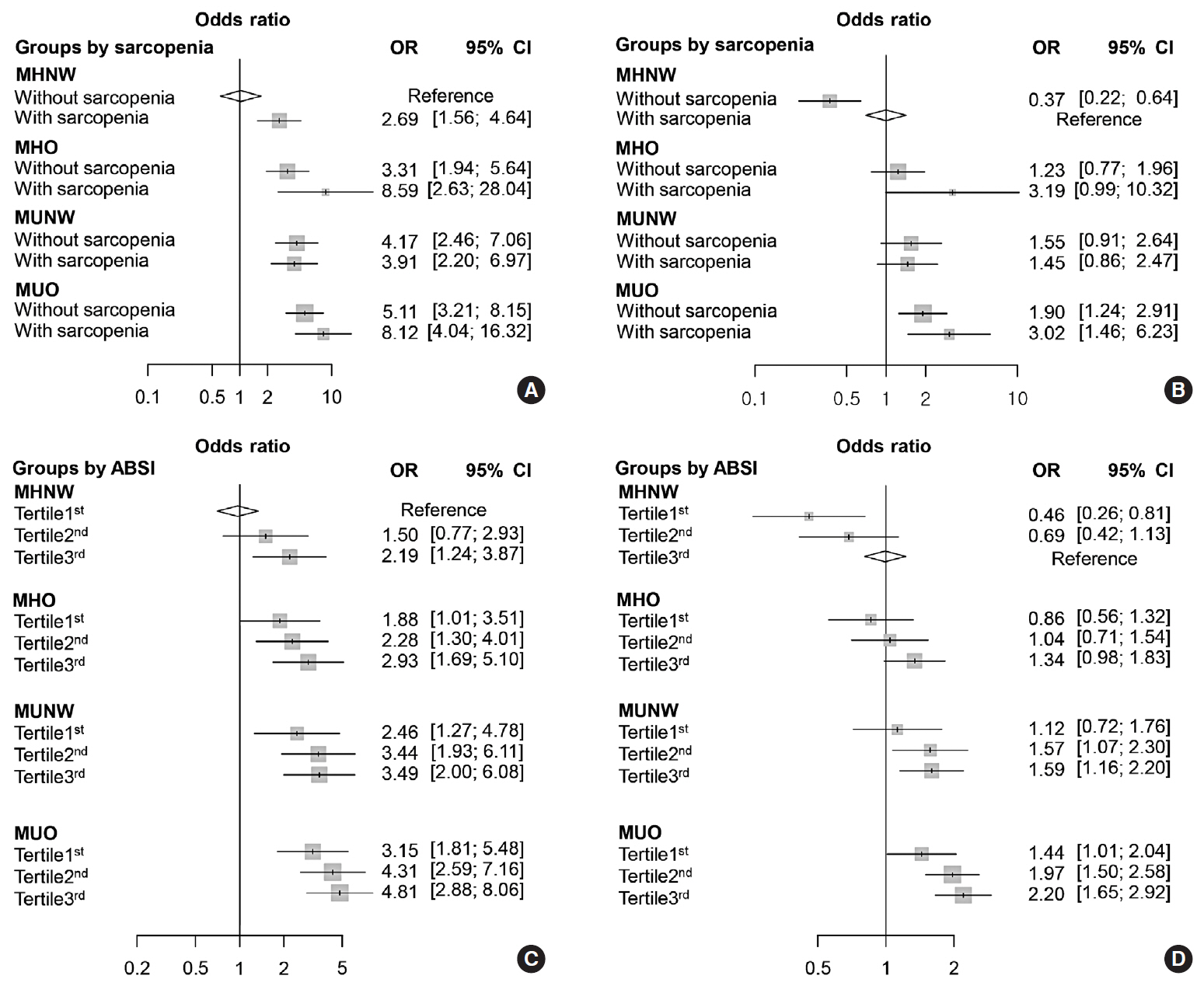
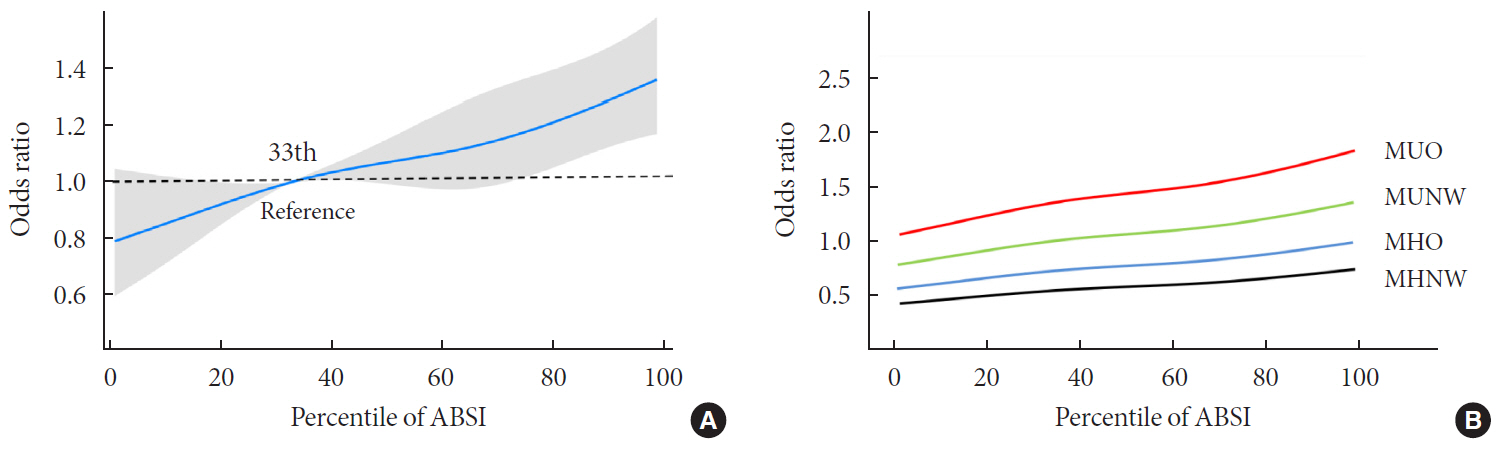
Results The MHNW participants with sarcopenia had higher risk for CVD than those without sarcopenia (OR, 2.69; 95% confidence interval [CI], 1.56 to 4.64). In the analysis with MHNW participants without sarcopenia as a reference, the participants with sarcopenia showed a higher OR for CVD than those without sarcopenia in both MHO (OR in participants without sarcopenia, 3.31; 95% CI, 1.94 to 5.64) (OR in participants with sarcopenia, 8.59; 95% CI, 2.63 to 28.04) and MUO participants (OR in participants without sarcopenia, 5.11; 95% CI, 3.21 to 8.15) (OR in participants with sarcopenia, 8.12; 95% CI, 4.04 to 16.32). Participants within the second and third tertiles of ABSI had higher ORs for CVDs than the counterpart of obesity phenotypes within the first tertile.
Conclusion These results suggest that clinical approaches that consider muscle and body shape are required.
Keyword
Figure
Cited by 2 articles
-
Skeletal Muscle Should Not Be Overlooked
Ji A Seo
Diabetes Metab J. 2021;45(2):173-174. doi: 10.4093/dmj.2021.0024.Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography
Hwi Seung Kim, Jiwoo Lee, Eun Hee Kim, Min Jung Lee, In Young Bae, Woo Je Lee, Joong-Yeol Park, Hong-Kyu Kim, Chang Hee Jung
Diabetes Metab J. 2023;47(1):104-117. doi: 10.4093/dmj.2022.0081.
Reference
-
1. Solomon CG, Manson JE. Obesity and mortality: a review of the epidemiologic data. Am J Clin Nutr. 1997; 66:4 Suppl. 1044S–1050S.2. Krauss RM, Winston M, Fletcher BJ, Grundy SM. Obesity: impact on cardiovascular disease. Circulation. 1998; 98:1472–1476.3. Moon S, Oh CM, Choi MK, Park YK, Chun S, Choi M, et al. The influence of physical activity on risk of cardiovascular disease in people who are obese but metabolically healthy. PLoS One. 2017; 12:e0185127.4. Wallstrom P, Bjartell A, Gullberg B, Olsson H, Wirfalt E. A prospective Swedish study on body size, body composition, diabetes, and prostate cancer risk. Br J Cancer. 2009; 100:1799–1805.
Article5. Kushner RF. Clinical assessment and management of adult obesity. Circulation. 2012; 126:2870–2877.6. Rey-Lopez JP, de Rezende LF, Pastor-Valero M, Tess BH. The prevalence of metabolically healthy obesity: a systematic review and critical evaluation of the definitions used. Obes Rev. 2014; 15:781–790.7. Kim TN, Choi KM. The implications of sarcopenia and sarcopenic obesity on cardiometabolic disease. J Cell Biochem. 2015; 116:1171–1178.8. Mirzababaei A, Djafarian K, Mozafari H, Shab-Bidar S. The long-term prognosis of heart diseases for different metabolic phenotypes: a systematic review and meta-analysis of prospective cohort studies. Endocrine. 2019; 63:439–462.9. Krakauer NY, Krakauer JC. A new body shape index predicts mortality hazard independently of body mass index. PLoS One. 2012; 7:e39504.10. Biolo G, Di Girolamo FG, Breglia A, Chiuc M, Baglio V, Vinci P, Toigo G, Lucchin L, Jurdana M, Praznikar ZJ, et al. Inverse relationship between “a body shape index” (ABSI) and fat-free mass in women and men: insights into mechanisms of sarcopenic obesity. Clin Nutr. 2015; 34:323–327.11. Chung W, Park JH, Chung HS, Yu JM, Kim DS, Moon S. Utility of the Z-score of log-transformed A Body Shape Index (LBSIZ) in the assessment for sarcopenic obesity and cardiovascular disease risk in the United States. Sci Rep. 2019; 9:9292.12. Centers for Disease Control and Prevention. The National Health and Nutrition Examination Survey (NHANES) MEC laboratory procedures manual. cited 2020 Mar 10. Available from: https://wwwn.cdc.gov/nchs/data/nhanes/2015-2016/manuals/2016_mec_laboratory_procedures_manual.pdf.13. World Health Organization. Fact sheet on obesity and overweight. cited 2020 Mar 10. Available from: http://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight.14. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. American Heart Association. National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005; 112:2735–2752.15. Jung CH, Lee MJ, Kang YM, Jang JE, Leem J, Hwang JY, et al. The risk of incident type 2 diabetes in a Korean metabolically healthy obese population: the role of systemic inflammation. J Clin Endocrinol Metab. 2015; 100:934–941.16. Heianza Y, Arase Y, Tsuji H, Fujihara K, Saito K, Hsieh SD, et al. Metabolically healthy obesity, presence or absence of fatty liver, and risk of type 2 diabetes in Japanese individuals: Toranomon Hospital Health Management Center Study 20 (TOPICS 20). J Clin Endocrinol Metab. 2014; 99:2952–2960.17. Hinnouho GM, Czernichow S, Dugravot A, Nabi H, Brunner EJ, Kivimaki M, et al. Metabolically healthy obesity and the risk of cardiovascular disease and type 2 diabetes: the Whitehall II cohort study. Eur Heart J. 2015; 36:551–559.18. Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, et al. Writing Group for the European Working Group on Sarcopenia in Older People 2 (EWGSOP2), and the Extended Group for EWGSOP2. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019; 48:16–31.19. Srikanthan P, Hevener AL, Karlamangla AS. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: findings from the National Health and Nutrition Examination Survey III. PLoS One. 2010; 5:e10805.20. Kim TN, Park MS, Yang SJ, Yoo HJ, Kang HJ, Song W, et al. Prevalence and determinant factors of sarcopenia in patients with type 2 diabetes: the Korean Sarcopenic Obesity Study (KSOS). Diabetes Care. 2010; 33:1497–1499.21. Han SS, Kim KW, Kim KI, Na KY, Chae DW, Kim S, et al. Lean mass index: a better predictor of mortality than body mass index in elderly Asians. J Am Geriatr Soc. 2010; 58:312–317.22. Wannamethee SG, Shaper AG, Lennon L, Whincup PH. Decreased muscle mass and increased central adiposity are independently related to mortality in older men. Am J Clin Nutr. 2007; 86:1339–1346.23. Atkins JL, Whincup PH, Morris RW, Lennon LT, Papacosta O, Wannamethee SG. Sarcopenic obesity and risk of cardiovascular disease and mortality: a population-based cohort study of older men. J Am Geriatr Soc. 2014; 62:253–260.24. Zamboni M, Mazzali G, Fantin F, Rossi A, Di Francesco V. Sarcopenic obesity: a new category of obesity in the elderly. Nutr Metab Cardiovasc Dis. 2008; 18:388–395.25. Choi KM. Sarcopenia and sarcopenic obesity. Endocrinol Metab (Seoul). 2013; 28:86–89.26. Lim S, Kim JH, Yoon JW, Kang SM, Choi SH, Park YJ, et al. Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean Longitudinal Study on Health and Aging (KLoSHA). Diabetes Care. 2010; 33:1652–1654.27. Lu CW, Yang KC, Chang HH, Lee LT, Chen CY, Huang KC. Sarcopenic obesity is closely associated with metabolic syndrome. Obes Res Clin Pract. 2013; 7:e301–e307.28. Choi KM. Sarcopenia and sarcopenic obesity. Korean J Intern Med. 2016; 31:1054–1060.29. Zhang X, Xie X, Dou Q, Liu C, Zhang W, Yang Y, et al. Association of sarcopenic obesity with the risk of all-cause mortality among adults over a broad range of different settings: a updated meta-analysis. BMC Geriatr. 2019; 19:183.30. Morkedal B, Vatten LJ, Romundstad PR, Laugsand LE, Janszky I. Risk of myocardial infarction and heart failure among metabolically healthy but obese individuals: HUNT (Nord-Trondelag Health Study), Norway. J Am Coll Cardiol. 2014; 63:1071–1078.31. Voulgari C, Tentolouris N, Dilaveris P, Tousoulis D, Katsilambros N, Stefanadis C. Increased heart failure risk in normal-weight people with metabolic syndrome compared with metabolically healthy obese individuals. J Am Coll Cardiol. 2011; 58:1343–1350.32. Gomez-Peralta F, Abreu C, Cruz-Bravo M, Alcarria E, Gutierrez-Buey G, Krakauer NY, et al. Relationship between “a body shape index (ABSI)” and body composition in obese patients with type 2 diabetes. Diabetol Metab Syndr. 2018; 10:21.33. Dhana K, Koolhaas CM, Schoufour JD, Rivadeneira F, Hofman A, Kavousi M, et al. Association of anthropometric measures with fat and fat-free mass in the elderly: the Rotterdam study. Maturitas. 2016; 88:96–100.
Article34. Lee DY, Lee MY, Sung KC. Prediction of mortality with a body shape index in young Asians: comparison with body mass index and waist circumference. Obesity (Silver Spring). 2018; 26:1096–1103.
Article35. Dhana K, Kavousi M, Ikram MA, Tiemeier HW, Hofman A, Franco OH. Body shape index in comparison with other anthropometric measures in prediction of total and cause-specific mortality. J Epidemiol Community Health. 2016; 70:90–96.
Article36. Bozorgmanesh M, Sardarinia M, Hajsheikholeslami F, Azizi F, Hadaegh F. CVD-predictive performances of “a body shape index” versus simple anthropometric measures: Tehran lipid and glucose study. Eur J Nutr. 2016; 55:147–157.
Article37. Ji M, Zhang S, An R. Effectiveness of A Body Shape Index (ABSI) in predicting chronic diseases and mortality: a systematic review and meta-analysis. Obes Rev. 2018; 19:737–759.
Article38. Chung W, Park JH, Ryu OH, Yu JM, Yoo HJ, Moon S. Association of Z-score of the log-transformed a body shape index with cardiovascular disease in people who are obese but metabolically healthy: the Korea National Health and Nutrition Examination Survey 2007–2010. J Obes Metab Syndr. 2018; 27:158–165.39. Arnlov J, Ingelsson E, Sundstrom J, Lind L. Impact of body mass index and the metabolic syndrome on the risk of cardiovascular disease and death in middle-aged men. Circulation. 2010; 121:230–236.
Article40. Hinnouho GM, Czernichow S, Dugravot A, Batty GD, Kivimaki M, Singh-Manoux A. Metabolically healthy obesity and risk of mortality: does the definition of metabolic health matter? Diabetes Care. 2013; 36:2294–2300.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Diverse Abnormal Body Composition Phenotypes: Interaction Between Muscle, Fat, and Bone
- Clinical Implication of Sarcopenia in Patients with Inflammatory Bowel Disease
- Sarcopenia: Definition, Epidemiology, and Pathophysiology
- Recent Progression in Sarcopenia and Sarcopenic Obesity
- Sarcopenia and sarcopenic obesity