Clin Endosc.
2021 Mar;54(2):242-249. 10.5946/ce.2020.275.
Insufflation of Carbon Dioxide versus Air During Colonoscopy Among Pediatric Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
- Affiliations
-
- 1Gastrointestinal Endoscopy Unit, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo, Brazil
- 2Gastroenterology and Hepatology Pediatric Unit, Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, São Paulo, Brazil
- 3Servicio de Gastroenterología, Clínica Maison de Sante del Sur Lima-Perú, Lima, Perú
- 4Division of Gastroenterology, Hepatology and Endoscopy, Brigham and Women’s Hospital, Boston, MA, USA
- KMID: 2514179
- DOI: http://doi.org/10.5946/ce.2020.275
Abstract
- Background/Aims
Carbon dioxide is increasingly used in insufflation during colonoscopy in adult patients; however, air insufflation remains the primary practice among pediatric gastroenterologists. This systematic review and meta-analysis aims to evaluate insufflation using CO2 versus air in colonoscopies in pediatric patients.
Methods
Individualized search strategies were performed using MEDLINE, Cochrane Library, EMBASE, and LILACS databases following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and Cochrane working methodology. Randomized control trials (RCTs) were selected for the present meta-analysis. Pooled proportions were calculated for outcomes including procedure time and abdominal pain immediately and 24 hours post-procedure.
Results
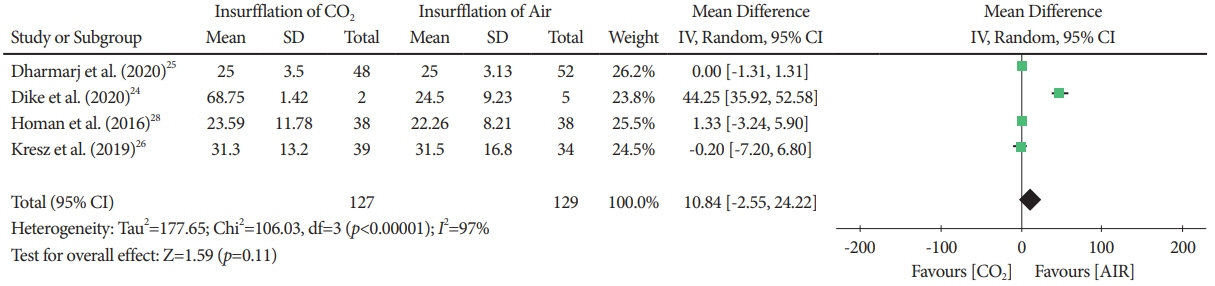
The initial search yielded 644 records, of which five RCTs with a total of 358 patients (CO2: n=178 versus air: n=180) were included in the final analysis. The procedure time was not different between the CO2 and air insufflation groups (mean difference, 10.84; 95% confidence interval [CI], -2.55 to 24.22; p=0.11). Abdominal pain immediately post-procedure was significantly lower in the CO2 group (risk difference, -0.15; 95% CI; -0.26 to -0.03; p=0.01) while abdominal pain at 24 hours post-procedure was similar (risk difference, -0.05; 95% CI; -0.11 to 0.01; p=0.11).
Conclusions
Based on this systematic review and meta-analysis of RCT data, CO2 insufflation reduced abdominal pain immediately following the procedure, while pain was similar at 24 hours post-procedure. These results suggest that CO2 is a preferred insufflation technique when performing colonoscopy in pediatric patients.
Keyword
Figure
Reference
-
1. Thomson M, Tringali A, Dumonceau J-M, et al. Paediatric gastrointestinal endoscopy. J Pediatr Gastroenterol Nutr. 2017; 64:133–153.2. Kiani M-A, Khodadad A, Mohammadi S, et al. Effect of peppermint on pediatrics’ pain under endoscopic examination of the large bowel. J HerbMed Pharmacol. 2013; 2:41–44.3. Yoshioka S, Takedatsu H, Fukunaga S, et al. Study to determine guidelines for pediatric colonoscopy. World J Gastroenterol. 2017; 21(23):5773.
Article4. Rocha RS de P, Ribeiro IB, de Moura DTH, et al. Sodium picosulphate or polyethylene glycol before elective colonoscopy in outpatients? a systematic review and meta-analysis. World J Gastrointest Endosc. 2018; 16(10):422–441.5. de Moura DT, Guedes H, Tortoretto V, et al. [Comparison of colon-cleansing methods in preparation for colonoscopy-comparative of solutions of mannitol and sodium picosulfate]. Rev Gastroenterol Peru. 2016; 36:293–297.6. Chen Y-J, Lee J, Puryear M, et al. A Randomized controlled study comparing room air with carbon dioxide for abdominal pain, distention, and recovery time in patients undergoing colonoscopy. Gastroenterol Nurs. 2014; 37:273–278.
Article7. Kim SY, Chung J-W, Park DK, et al. Comparison of carbon dioxide and air insufflation during consecutive EGD and colonoscopy in moderate-sedation patients: a prospective, double-blind, randomized controlled trial. Gastrointest Endosc. 2017; 85:1255–1262.8. Fernández-Calderón M, Muñoz-Navas MÁ, Carrascosa-Gil J, et al. Carbon dioxide vs. air insufflation in ileo-colonoscopy and in gastroscopy plus ileo-colonoscopy: a comparative study. Rev Esp Enferm Dig. 2012; 104:237–241.
Article9. de Miranda Neto AA, de Moura DTH, Hathorn KE, Tustumi F, de Moura EGH, Ribeiro IB. Efficacy and patient tolerability of split-dose sodium picosulfate/magnesium citrate (SPMC) oral solution compared to the polyethylene glycol (PEG) solution for bowel preparation in outpatient colonoscopy: an evidence-based review. Clin Exp Gastroenterol. 2020; 13:449–457.10. Victoria NC, Murphy AZ. Exposure to early life pain: long term consequences and contributing mechanisms. Curr Opin Behav Sci. 2016; 7:61–68.
Article11. Lee GY, Yamada J, Kyololo O, Shorkey A, Stevens B. Pediatric clinical practice guidelines for acute procedural pain: a systematic review. Pediatrics. 2014; 133:500–515.
Article12. Kiani MA, Heydarian F, Feyzabadi Z, Saeidi M, Jafari SA, Hebrani P. Effect of music and toys on reducing pain during colonoscopy and acceptance of colonoscopy by children: a randomized clinical trial. Electron physician. 2019; 11:7652–7659.
Article13. Memon MA, Memon B, Yunus RM, Khan S. Carbon dioxide versus air insufflation for elective colonoscopy. Surg Laparosc Endosc Percutan Tech. 2016; 26:102–116.
Article14. Nishizawa T, Suzuki H, Fujimoto A, Ochiai Y, Kanai T, Naohisa Y. Effects of carbon dioxide insufflation in balloon-assisted enteroscopy: a systematic review and meta-analysis. United Eur Gastroenterol J. 2016; 4:11–17.
Article15. Nambu R, Hagiwara S-I, Kakuta F, et al. Current role of colonoscopy in infants and young children: a multicenter study. BMC Gastroenterol. 2019; 19:149.
Article16. Ribeiro IB, Moura DTH de, Thompson CC, Moura EGH de. Acute abdominal obstruction: colon stent or emergency surgery? an evidence-based review. World J Gastrointest Endosc. 2019; 11:193–208.
Article17. Rogers BH. The safety of carbon dioxide insufflation during colonoscopic electrosurgical polypectomy. Gastrointest Endosc. 1974; 20:115–117.18. Dellon ES, Hawk JS, Grimm IS, Shaheen NJ. The use of carbon dioxide for insufflation during GI endoscopy: a systematic review. Gastrointest Endosc. 2009; 69:843–849.
Article19. Passos ML, Ribeiro IB, de Moura DTH, et al. Efficacy and safety of carbon dioxide insufflation versus air insufflation during endoscopic retrograde cholangiopancreatography in randomized controlled trials: a systematic review and meta-analysis. Endosc Int open. 2019; 7:E487–E497.
Article20. Aquino JCM, Bernardo WM, de Moura DTH, et al. Carbon dioxide versus air insufflation enteroscopy: a systematic review and meta-analysis based on randomized controlled trials. Endosc Int Open. 2018; 06:E637–E645.
Article21. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. 2009; 62:e1–e34.
Article22. Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019; 366:l4898.
Article23. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005; 5:13.
Article24. Dike CR, Rahhal R, Bishop WP. Is carbon dioxide insufflation during endoscopy in children as safe and as effective as we think? J Pediatr Gastroenterol Nutr. 2020; 71:211–215.
Article25. Dharmaraj R, Dunn R, Fritz J, et al. Efficacy and safety of carbon dioxide versus air insufflation for colonoscopy in deeply sedated pediatric patients. J Pediatr Gastroenterol Nutr. 2020; 71:34–39.
Article26. Kresz A, Mayer B, Zernickel M, Posovszky C. Carbon dioxide versus room air for colonoscopy in deeply sedated pediatric patients: a randomized controlled trial. Endosc Int Open. 2019; 07:E290–E297.
Article27. Thornhill C, Navarro F, Alabd Alrazzak B,, et al. Insufflation with carbon dioxide during pediatric colonoscopy for control of postprocedure pain. J Clin Gastroenterol. 2018; 52:715–720.
Article28. Homan M, Mahkovic D, Orel R, Mamula P. Randomized, double-blind trial of CO2 versus air insufflation in children undergoing colonoscopy. Gastrointest Endosc. 2016; 83:993–997.
Article29. de Moura DT, Guedes H, Tortoretto V, et al. Comparison of colon-cleansing methods in preparation for colonoscopy-comparative of solutions of mannitol and sodium picosulfate. Rev Gastroenterol Peru. 2016; 36:293–297.30. Saltzman HA, Sieker HO. Intestinal response to changing gaseous environments: normobaric and hyperbaric observations. Ann N Y Acad Sci. 1968; 150:31–39.
Article31. Sajid MS, Caswell J, Bhatti MI, Sains P, Baig MK, Miles WFA. Carbon dioxide insufflation vs conventional air insufflation for colonoscopy: a systematic review and meta-analysis of published randomized controlled trials. Color Dis. 2015; 17:111–123.32. Bassan MS, Holt B, Moss A, Williams SJ, Sonson R, Bourke MJ. Carbon dioxide insufflation reduces number of postprocedure admissions after endoscopic resection of large colonic lesions: a prospective cohort study. Gastrointest Endosc. 2013; 77:90–95.
Article33. Coronel M, Korkischko N, Bernardo WM, et al. Comparison between carbon dioxide and air insufflation in colonoscopy: a systematic review and meta-analysis based on randomized control trials. J Gastroenterol Pancreatol Liver Disord. 2017; 4:1–11.
Article34. Rogers AC, Van De Hoef D, Sahebally SM, Winter DC. A meta-analysis of carbon dioxide versus room air insufflation on patient comfort and key performance indicators at colonoscopy. Int J Colorectal Dis. 2020; 35:455–464.
Article35. HoRutterzo MD, Chattree A, Barbour JA, et al. British Society of Gastroenterology/Association of Coloproctologists of Great Britain and Ireland guidelines for the management of large non-pedunculated colorectal polyps. Gut. 2015; 64:1847–1873.
Article36. Valori R, Rey J-F, Atkin W, et al. European guidelines for quality assurance in colorectal cancer screening and diagnosis. First Edition – Quality assurance in endoscopy in colorectal cancer screening and diagnosis. Endoscopy. 2012; 44(Suppl 3):SE88–SE105.
Article37. Paspatis GA, Dumonceau J-M, Barthet M, et al. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement. Endoscopy. 2014; 46:693–711.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Carbon Dioxide versus Air Insufflation in Gastric Endoscopic Submucosal Dissection: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
- Difficult colonoscopy: air, carbon dioxide, or water insufflation?
- Painless Colonoscopy: Available Techniques and Instruments
- Can water insufflation and carbon dioxide overcome the difficulties of colonoscope insertion?
- Carbon Dioxide Insufflation in Endoscopic Submucosal Dissection: Is It an Urgent Need?