Intest Res.
2018 Apr;16(2):299-305. 10.5217/ir.2018.16.2.299.
Difficult colonoscopy: air, carbon dioxide, or water insufflation?
- Affiliations
-
- 1Department of Gastroenterology, Lokmanya Tilak Municipal Medical College and General Hospital, Mumbai, India. alishachaubal@gmail.com
- KMID: 2417683
- DOI: http://doi.org/10.5217/ir.2018.16.2.299
Abstract
- BACKGROUND/AIMS
This study aimed to compare tolerance to air, carbon dioxide, or water insufflation in patients with anticipated difficult colonoscopy (young, thin, obese individuals, and patients with prior abdominal surgery or irradiation).
METHODS
Patients with body mass index (BMI) less than 18 kg/m2 or more than 30 kg/m2, or who had undergone previous abdominal or pelvic surgeries were randomized to air, carbon dioxide, or water insufflation during colonoscopy. The primary endpoint was cecal intubation with mild pain (less than 5 on visual analogue scale [VAS]), without use of sedation.
RESULTS
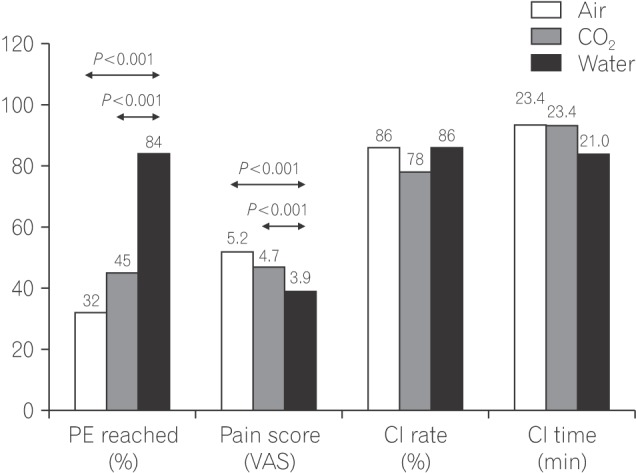
The primary end point was achieved in 32.7%, 43.8%, and 84.9% of cases with air, carbon dioxide and water insufflation (P < 0.001). The mean pain scores were 5.17, 4.72, and 3.93 on the VAS for air, carbon dioxide, and water insufflation (P < 0.001). The cecal intubation rate or procedure time did not differ significantly between the 3 groups.
CONCLUSIONS
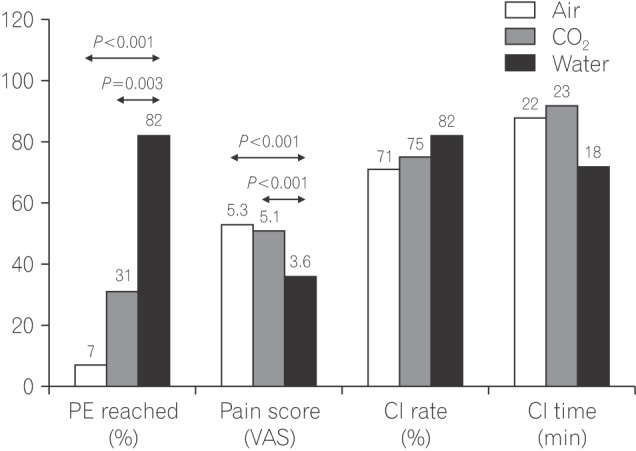
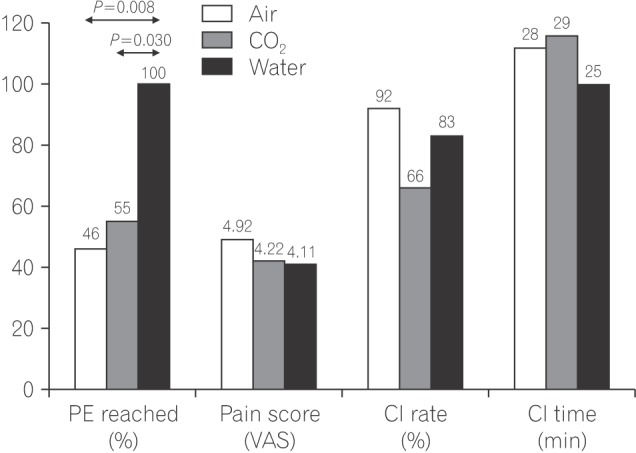
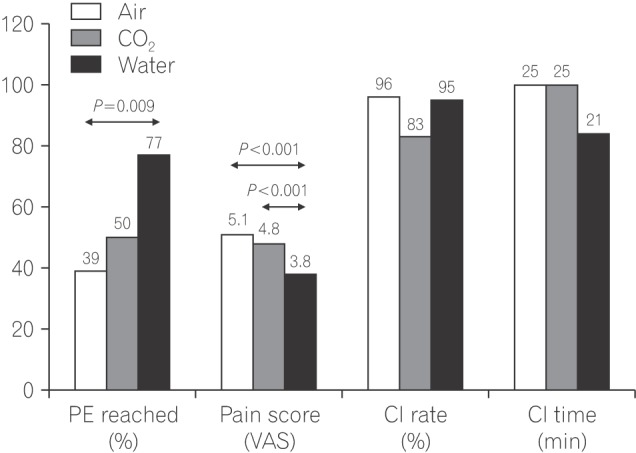
Water insufflation was superior to air or carbon dioxide for pain tolerance. This was seen in the subgroups with BMI < 18 kg/m2 and the post-surgical group, but not in the group with BMI >30 kg/m2.
MeSH Terms
Figure
Cited by 1 articles
-
Can water insufflation and carbon dioxide overcome the difficulties of colonoscope insertion?
Choong-Kyun Noh, Kee Myung Lee
Intest Res. 2018;16(2):166-167. doi: 10.5217/ir.2018.16.2.166.
Reference
-
1. Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Prospective evaluation of factors predicting difficulty and pain during sedation-free colonoscopy. Dis Colon Rectum. 2005; 48:1295–1300. PMID: 15793639.
Article2. Takahashi Y, Tanaka H, Kinjo M, Sakumoto K. Sedation-free colonoscopy. Dis Colon Rectum. 2005; 48:855–859. PMID: 15768182.
Article3. Garborg K, Kaminski MF, Lindenburger W, et al. Water exchange versus carbon dioxide insufflation in unsedated colonoscopy: a multicenter randomized controlled trial. Endoscopy. 2015; 47:192–199. PMID: 25412093.
Article4. Cadoni S, Gallittu P, Sanna S, et al. A two-center randomized controlled trial of water-aided colonoscopy versus air insufflation colonoscopy. Endoscopy. 2014; 46:212–218. PMID: 24218307.
Article5. Ramirez FC, Leung FW. A head-to-head comparison of the water vs. air method in patients undergoing screening colonoscopy. J Interv Gastroenterol. 2011; 1:130–135. PMID: 22163084.6. Lai EJ, Calderwood AH, Doros G, Fix OK, Jacobson BC. The Boston bowel preparation scale: a valid and reliable instrument for colonoscopy-oriented research. Gastrointest Endosc. 2009; 69(3 Pt 2):620–625. PMID: 19136102.
Article7. Martín-Noguerol E, González-Santiago JM, Martínez-Alcalá C, et al. Split-dose sodium picosulphate/magnesium citrate for morning colonoscopies performed 2 to 6 hours after fluid intake. Gastroenterol Hepatol. 2013; 36:254–260. PMID: 23537750.8. Rex DK, Petrini JL, Baron TH, et al. Quality indicators for colonoscopy. Am J Gastroenterol. 2006; 101:873–885. PMID: 16635231.
Article9. McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol Med. 1988; 18:1007–1019. PMID: 3078045.
Article10. Rex DK. Achieving cecal intubation in the very difficult colon. Gastrointest Endosc. 2008; 67:938–944. PMID: 18440383.
Article11. Anderson JC, Messina CR, Cohn W, et al. Factors predictive of difficult colonoscopy. Gastrointest Endosc. 2001; 54:558–562. PMID: 11677470.
Article12. Desormeaux MP, Scicluna M, Friedland S. Colonoscopy in obese patients: a growing problem. Gastrointest Endosc. 2008; 67:AB89–AB90.
Article13. Anderson JC. Water-aided colonoscopy. Gastrointest Endosc Clin N Am. 2015; 25:211–226. PMID: 25839683.
Article14. Leung JW, Thai A, Yen A, et al. Magnetic endoscope imaging (ScopeGuide) elucidates the mechanism of action of the painalleviating impact of water exchange colonoscopy: attenuation of loop formation. J Interv Gastroenterol. 2012; 2:142–146. PMID: 23805397.
Article15. Cadoni S, Sanna S, Gallittu P, et al. A randomized, controlled trial comparing real-time insertion pain during colonoscopy confirmed water exchange to be superior to water immersion in enhancing patient comfort. Gastrointest Endosc. 2015; 81:557–566. PMID: 25262100.
Article16. Leung JW, Mann SK, Siao-Salera R, et al. A randomized, controlled comparison of warm water infusion in lieu of air insufflation versus air insufflation for aiding colonoscopy insertion in sedated patients undergoing colorectal cancer screening and surveillance. Gastrointest Endosc. 2009; 70:505–510. PMID: 19555938.
Article17. Becker GL. The prevention or gas explosions in the large bowel during electrosurgery. Surg Gynecol Obstet. 1953; 97:463–467. PMID: 13102174.19. Sajid MS, Caswell J, Bhatti MI, Sains P, Baig MK, Miles WF. Carbon dioxide insufflation vs conventional air insufflation for colonoscopy: a systematic review and meta-analysis of published randomized controlled trials. Colorectal Dis. 2015; 17:111–123. PMID: 25393051.
Article20. Vemulapalli KC, Rex DK. Water immersion simplifies cecal intubation in patients with redundant colons and previous incomplete colonoscopies. Gastrointest Endosc. 2012; 76:812–817. PMID: 22901988.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Painless Colonoscopy: Available Techniques and Instruments
- Can water insufflation and carbon dioxide overcome the difficulties of colonoscope insertion?
- Carbon Dioxide Insufflation in Endoscopic Submucosal Dissection: Is It an Urgent Need?
- Carbon Dioxide Embolism during Laparoscopic Surgery
- Unsedated Colonoscopy and the Water Method for Minimizing Discomfort in the Unsedated Patients