J Korean Med Sci.
2021 Mar;36(11):e81. 10.3346/jkms.2021.36.e81.
The Prediction of Bronchopulmonary Dysplasia in Very Low Birth Weight Infants through Clinical Indicators within 1 Hour of Delivery
- Affiliations
-
- 1Department of Pediatrics, School of Medicine, Ewha Womans University, Seoul, Korea
- 2Department of Pediatrics, Ewha Womans University Mokdong Hospital, Seoul, Korea
- 3Informatization Department, Ewha Womans University, Seoul, Korea
- KMID: 2514054
- DOI: http://doi.org/10.3346/jkms.2021.36.e81
Abstract
- Background
Despite the advances in neonatology, the incidence of bronchopulmonary dysplasia (BPD) is increasing. It is important to prevent the development of BPD in the first place. The online BPD outcome estimator from National Institute of Children Health and Human Development and Neonatal Research Network is available. However, it is not applicable for Asians. Moreover, limits are set for birth weight and gestational weeks excluding those who may still have BPD. The aim of this study was to develop a prediction model for BPD using first hour perinatal and neonatal factors in Korean very low birth weight infants (VLBWIs).
Methods
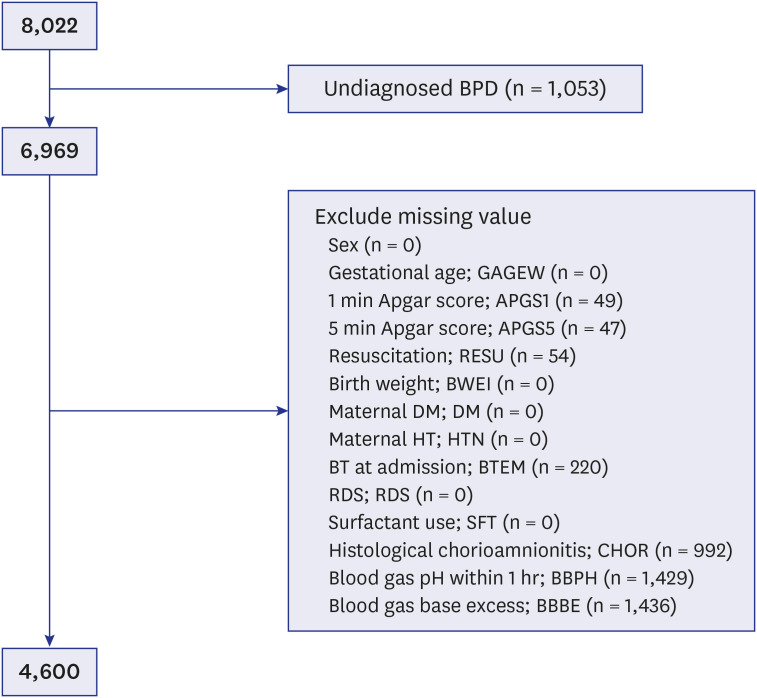
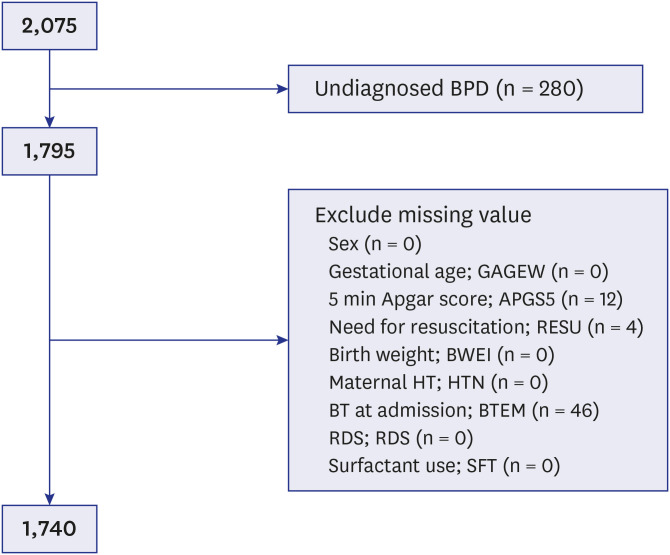
Data were collected for 8,022 VLBWIs with gestational age (GA) ≥ 22 weeks who were born between January 1, 2013 and December 31, 2016, and admitted to the neonatal intensive care units of the KNN. Multiple logistic regression models reanalyzed by stepwise selection with significant clinical indicators for BPD. PROC package was used to calculate the area under curve (AUC) and corresponding 95% confidence intervals. Moreover, it was used to search the best cut-off value. External validation was performed with the 2017 Korean neonatal network (KNN) data.
Results
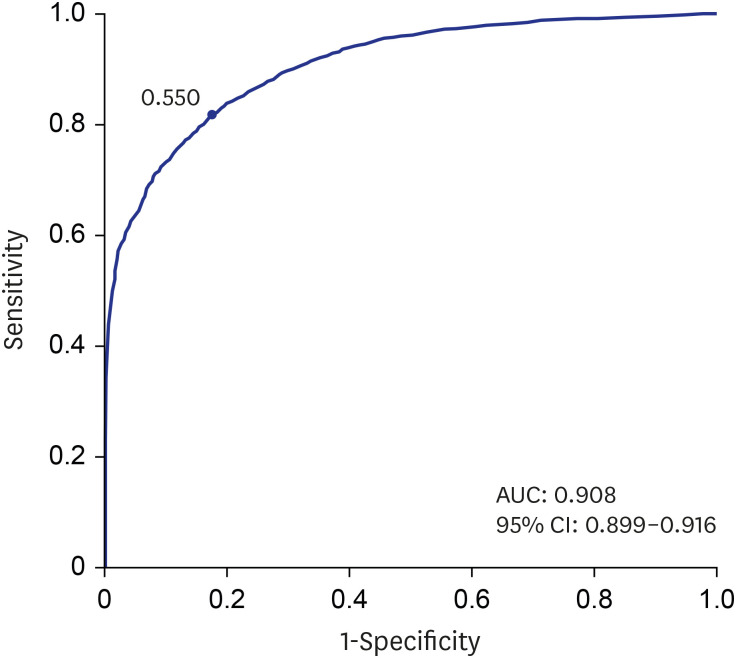
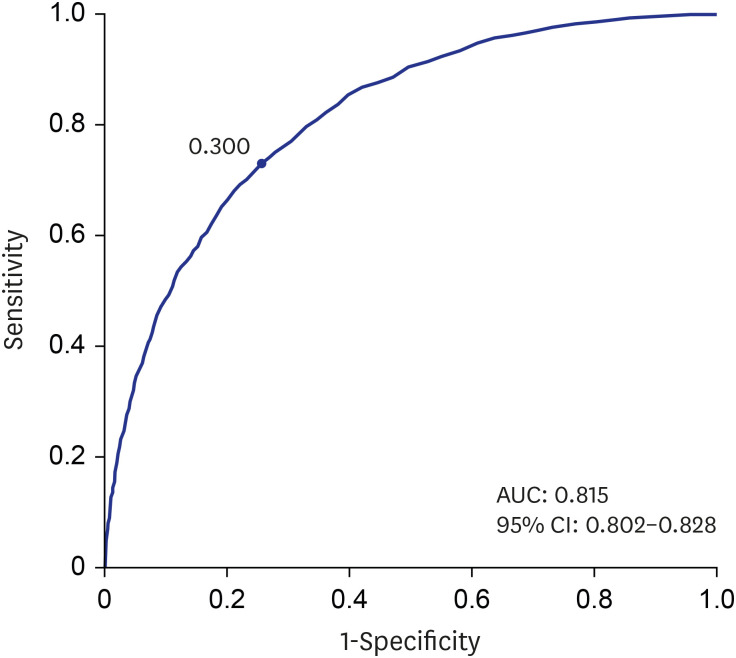
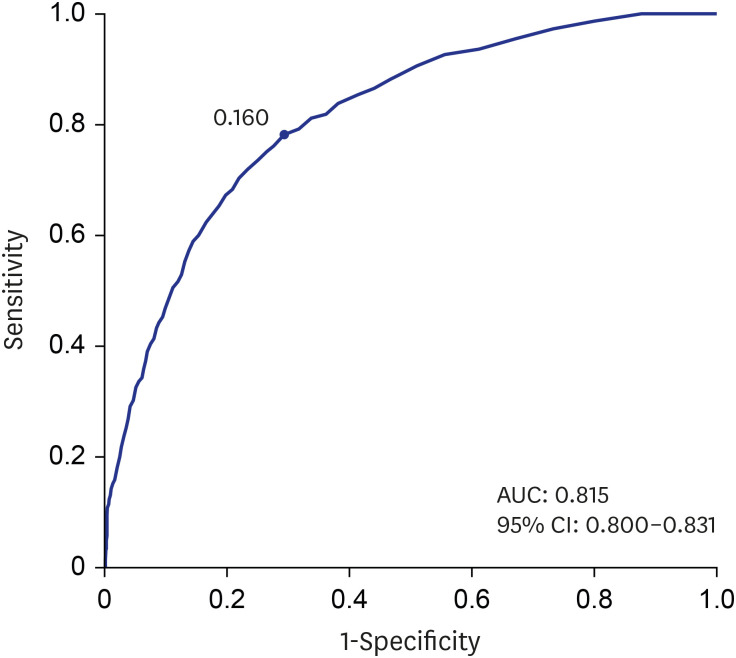
After all missing data were excluded, 4,600 VLBWIs were included in the training dataset of the prediction model. Predictability of presence of BPD was 90.8% and prediction P value cut off was 0.550. Five-minute Apgar score, birth weight, GA, sex, surfactant use were significant indicators. Predictability of severe BPD was 81.5% and prediction P value cut off was 0.160. Five-minute Apgar score, birth weight, maternal PIH, chronic maternal hypertension, GA, sex, respiratory distress syndrome, need of resuscitation at birth were significant indicators. After external validation, sensitivity and specificity did not change significantly.
Conclusion
From this study, high predictability was obtained using clinical parameters obtained within one hour of life. P value for prediction of each grade of BPD and equation for calculation was presented. It can be helpful for the early prediction of BPD in Korean VLBWI. This study will contribute to the prediction of BPD in Asians especially Korean VLBWIs, not currently included in the NICHD BPD online BPD predictor. In addition, the predictive power may be continuously increased with the cumulative data of KNN.
Figure
Reference
-
1. Van Marter LJ. Epidemiology of bronchopulmonary dysplasia. Semin Fetal Neonatal Med. 2009; 14(6):358–366. PMID: 19783238.
Article2. Zysman-Colman Z, Tremblay GM, Bandeali S, Landry JS. Bronchopulmonary dysplasia - trends over three decades. Paediatr Child Health. 2013; 18(2):86–90. PMID: 24421662.
Article3. Smith VC, Zupancic JA, McCormick MC, Croen LA, Greene J, Escobar GJ, et al. Rehospitalization in the first year of life among infants with bronchopulmonary dysplasia. J Pediatr. 2004; 144(6):799–803. PMID: 15192629.
Article4. Dumpa V, Bhandari V. Surfactant, steroids and non-invasive ventilation in the prevention of BPD. Semin Perinatol. 2018; 42(7):444–452. PMID: 30343941.
Article5. Bancalari E, Claure N, Sosenko IR. Bronchopulmonary dysplasia: changes in pathogenesis, epidemiology and definition. Semin Neonatol. 2003; 8(1):63–71. PMID: 12667831.
Article6. Laughon MM, Langer JC, Bose CL, Smith PB, Ambalavanan N, Kennedy KA, et al. Prediction of bronchopulmonary dysplasia by postnatal age in extremely premature infants. Am J Respir Crit Care Med. 2011; 183(12):1715–1722. PMID: 21471086.
Article7. The Executive Committee of Korean Neonatal Network. 2016 Korean Neonatal Network Annual Report. Cheongju: Korea Centers for Disease Control and Prevention;2017.8. Jo HS, Cho KH, Cho SI, Song ES, Kim BI. Recent changes in the incidence of bronchopulmonary dysplasia among very low birth weight infants in Korea. J Korean Med Sci. 2015; 30(Suppl 1):S81–S87. PMID: 26566362.9. Chang YS, Ahn SY, Park WS. The establishment of the Korean Neonatal Network (KNN). Neonatal Med. 2013; 20(2):169–178.
Article10. The Executive Committee of Korean Neonatal Network. 2013 Korean Neonatal Network Annual Report. Cheongju: Korea Centers for Disease Control and Prevention;2014.11. The Executive Committee of Korean Neonatal Network. 2014 Korean Neonatal Network Annual Report. Cheongju: Korea Centers for Disease Control and Prevention;2015.12. The Executive Committee of Korean Neonatal Network. 2015 Korean Neonatal Network Annual Report. Cheongju: Korea Centers for Disease Control and Prevention;2016.13. The Executive Committee of Korean Neonatal Network. 2016 Korean Neonatal Network Annual Report. Cheongju: Korea Centers for Disease Control and Prevention;2017.14. Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005; 116(6):1353–1360. PMID: 16322158.
Article15. The Executive Committee of Korean Neonatal Network. 2017 Korean Neonatal Network Annual Report. Cheongju: Korea Centers for Disease Control and Prevention;2018.16. Onland W, Debray TP, Laughon MM, Miedema M, Cools F, Askie LM, et al. Clinical prediction models for bronchopulmonary dysplasia: a systematic review and external validation study. BMC Pediatr. 2013; 13(1):207–226. PMID: 24345305.
Article17. Parker RA, Lindstrom DP, Cotton RB. Improved survival accounts for most, but not all, of the increase in bronchopulmonary dysplasia. Pediatrics. 1992; 90(5):663–668. PMID: 1408535.18. Henderson-Smart DJ, Hutchinson JL, Donoghue DA, Evans NJ, Simpson JM, Wright I, et al. Prenatal predictors of chronic lung disease in very preterm infants. Arch Dis Child Fetal Neonatal Ed. 2006; 91(1):F40–5. PMID: 16131530.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiology, Clinical Characteristics, and Pathophysiology of Bronchopulmonary Dysplasia
- Risk Factors of Bronchopulmonary Dysplasia and Prediction in Korea
- Prevention and Treatment of Bronchopulmonary Dysplasia
- Rehospitalization of Low-birth-weight Infants Who Were Discharged from NICU
- Recent progress in the understanding of clinical characteristics, epidemiology, and pathogenesis of new bronchopulmonary dysplasia