Obstet Gynecol Sci.
2021 Mar;64(2):226-233. 10.5468/ogs.20243.
The baseline recurrence risk of patients with intermediate-risk cervical cancer
- Affiliations
-
- 1Department of Gynecology, National Cancer Center Hospital, Tokyo, Japan
- 2Department of Obstetrics and Gynecology, Shiga University of Medical Science, Shiga, Japan
- KMID: 2513952
- DOI: http://doi.org/10.5468/ogs.20243
Abstract
Objective
This study aimed to investigate the prognosis of patients with intermediate-risk cervical cancer and to evaluate the necessity of adjuvant therapy.
Methods
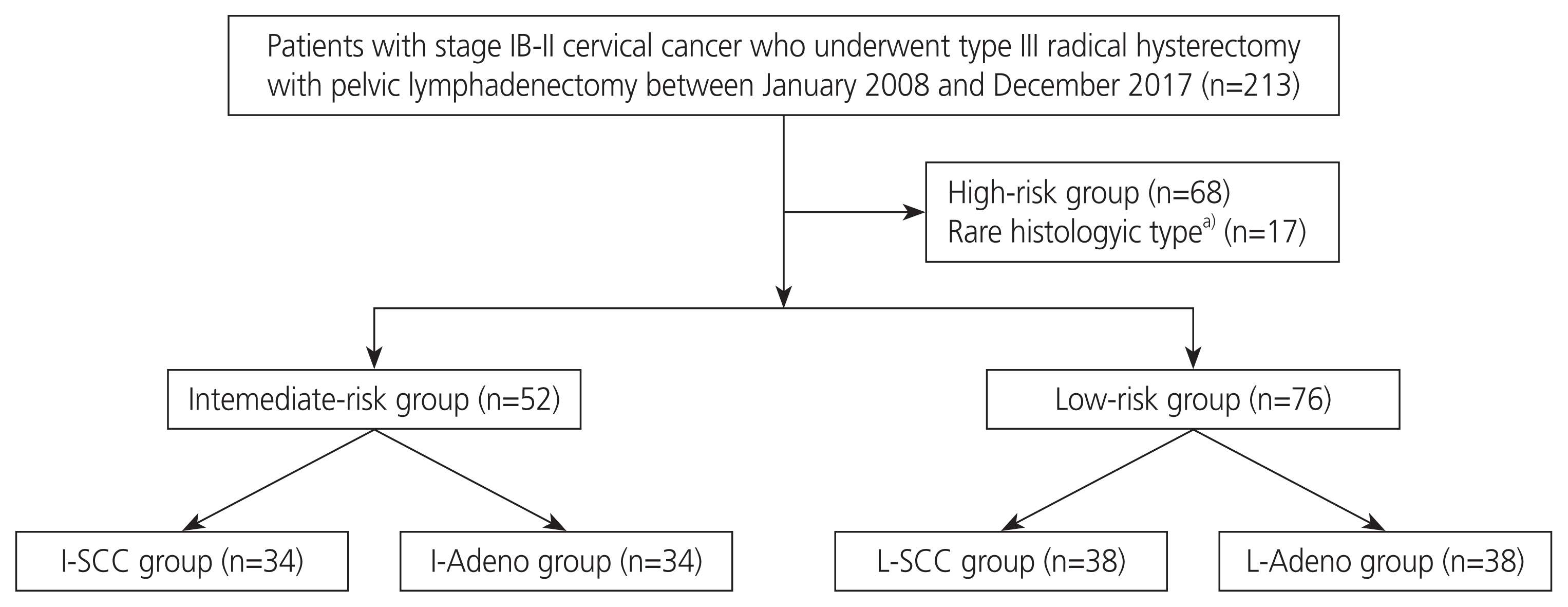
We conducted a retrospective chart review of patients with stage IB–II cervical cancer who underwent type III radical hysterectomy with pelvic lymphadenectomy between 2008 and 2017. In our institution, radical hysterectomy is performed as an open surgery and not as a minimally invasive surgery, and adjuvant therapy is not administered to patients with intermediate-risk cervical cancer. The intermediate-risk group included patients with 2 or more of the following factors: tumor size >4 cm, stromal invasion >1/2, and lymphovascular stromal invasion. Intermediaterisk patients with squamous cell carcinoma were included in the I-SCC group, whereas those with endocervical adenocarcinoma, usual type, or adenosquamous carcinoma were included in the I-Adeno group.
Results
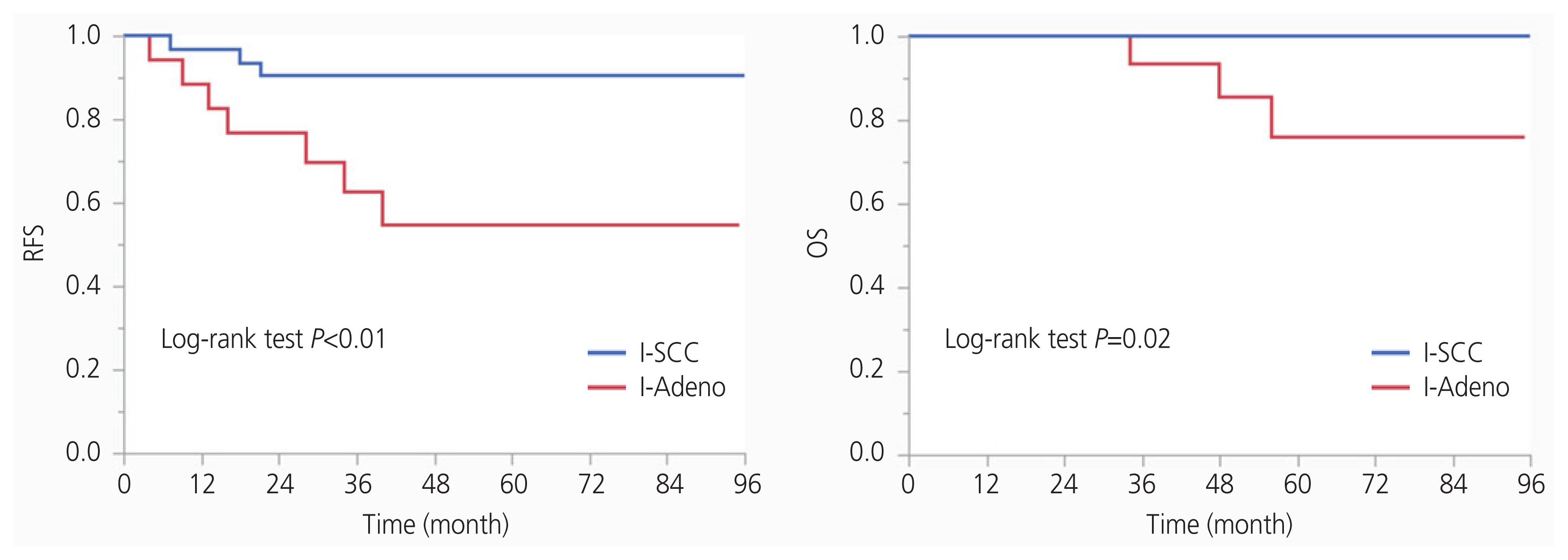
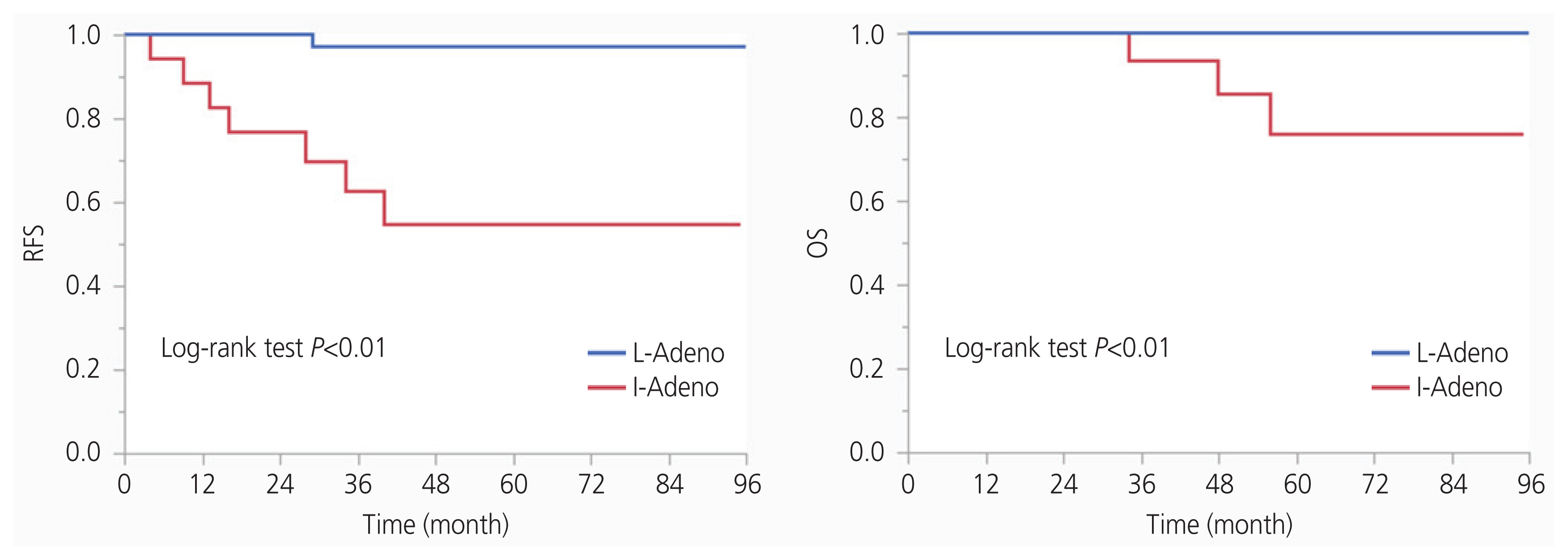
There were 34 and 18 patients in the I-SCC and I-Adeno groups, respectively. The 5-year recurrence-free survival (RFS) and overall survival rates in the I-SCC group were 90.5% (95% confidence interval [CI], 85.3–95.7%) and 100% (95% CI, 100%), respectively, whereas those in the I-Adeno group were 54.9% (95% CI, 42.0–67.9%) and 76.1% (95% CI, 63.7–88.4%), respectively. Multivariate analysis revealed that endocervical adenocarcinoma, usual type, or adenosquamous carcinoma, and tumor size >4 cm had worse RFS.
Conclusion
The I-SCC group had good prognosis without adjuvant therapy; therefore, adjuvant therapy may be omitted in these patients. In contrast, the I-Adeno group had poor prognosis without adjuvant therapy; therefore, adjuvant therapy should be considered in their treatment.
Figure
Reference
-
References
1. Sedlis A, Bundy BN, Rotman MZ, Lentz SS, Muderspach LI, Zaino RJ. A randomized trial of pelvic radiation therapy versus no further therapy in selected patients with stage IB carcinoma of the cervix after radical hysterectomy and pelvic lymphadenectomy: a Gynecologic Oncology Group study. Gynecol Oncol. 1999; 73:177–83.
Article2. Rotman M, Sedlis A, Piedmonte MR, Bundy B, Lentz SS, Muderspach LI, et al. A phase III randomized trial of postoperative pelvic irradiation in stage IB cervical carcinoma with poor prognostic features: follow-up of a gynecologic oncology group study. Int J Radiat Oncol Biol Phys. 2006; 65:169–76.
Article3. Cibula D, Abu-Rustum NR, Fischerova D, Pather S, Lavigne K, Slama J, et al. Surgical treatment of “intermediate risk” lymph node negative cervical cancer patients without adjuvant radiotherapy - A retrospective cohort study and review of the literature. Gynecol Oncol. 2018; 151:438–43.4. Nakamura K, Kitahara Y, Satoh T, Takei Y, Takano M, Nagao S, et al. Analysis of the effect of adjuvant radiotherapy on outcomes and complications after radical hysterectomy in FIGO stage IB1 cervical cancer patients with intermediate risk factors (GOTIC study). World J Surg Oncol. 2016; 14:173.
Article5. National Comprehensive Cancer Network (NCCN). NCCN Clinical Practice Guidelines in Oncology. Cervical cancer version 2. 2020 [Internet]. In : Plymouth Meeting, PA: NCCN; 2020; [cited 2020 Oct 2]. Available from: https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf .6. Ebina Y, Mikami M, Nagase S, Tabata T, Kaneuchi M, Tashiro H, et al. Japan Society of Gynecologic Oncology guidelines 2017 for the treatment of uterine cervical cancer. Int J Clin Oncol. 2019; 24:1–19.
Article7. Ryu SY, Kim MH, Nam BH, Lee TS, Song ES, Park CY, et al. Intermediate-risk grouping of cervical cancer patients treated with radical hysterectomy: a Korean Gynecologic Oncology Group study. Br J Cancer. 2014; 110:278–85.
Article8. Machida H, Matsuo K, Furusawa A, Kita T, Kitagawa R, Mikami M. Profile of treatment-related complications in women with clinical stage IB-IIB cervical cancer: a nationwide cohort study in Japan. PLoS One. 2019; 14:e0210125.
Article9. Jung PS, Kim DY, Lee SW, Park JY, Suh DS, Kim JH, et al. Clinical role of adjuvant chemotherapy after radical hysterectomy for FIGO stage IB-IIA cervical cancer: comparison with adjuvant RT/CCRT using inverse-probability-of-treatment weighting. PLoS One. 2015; 10:e0132298.
Article10. Lai CH, Chou HH, Chang CJ, Wang CC, Hsueh S, Huang YT, et al. Clinical implications of human papillomavirus genotype in cervical adeno-adenosquamous carcinoma. Eur J Cancer. 2013; 49:633–41.
Article11. Baek MH, Park JY, Kim D, Suh DS, Kim JH, Kim YM, et al. Comparison of adenocarcinoma and adenosquamous carcinoma in patients with early-stage cervical cancer after radical surgery. Gynecol Oncol. 2014; 135:462–7.
Article12. Huang YT, Wang CC, Tsai CS, Lai CH, Chang TC, Chou HH, et al. Clinical behaviors and outcomes for adenocarcinoma or adenosquamous carcinoma of cervix treated by radical hysterectomy and adjuvant radiotherapy or chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2012; 84:420–7.
Article13. Noh JM, Park W, Kim YS, Kim JY, Kim HJ, Kim J, et al. Comparison of clinical outcomes of adenocarcinoma and adenosquamous carcinoma in uterine cervical cancer patients receiving surgical resection followed by radiotherapy: a multicenter retrospective study (KROG 13–10). Gynecol Oncol. 2014; 132:618–23.
Article14. Pan X, Yang W, Wen Z, Li F, Tong L, Tang W. Does adenocarcinoma have a worse prognosis than squamous cell carcinoma in patients with cervical cancer? A real-world study with a propensity score matching analysis. J Gynecol Oncol. 2020; 31:e80.
Article15. Matsuo K, Shimada M, Yokota H, Satoh T, Katabuchi H, Kodama S, et al. Effectiveness of adjuvant systemic chemotherapy for intermediate-risk stage IB cervical cancer. Oncotarget. 2017; 8:106866–75.
Article16. Lee KB, Lee JM, Ki KD, Lee SK, Park CY, Ha SY. Comparison of adjuvant chemotherapy and radiation in patients with intermediate risk factors after radical surgery in FIGO stage IB-IIA cervical cancer. Int J Gynecol Cancer. 2008; 18:1027–31.
Article17. Shimada M, Nishimura R, Hatae M, Hiura M, Takehara K, Tase T, et al. Comparison of adjuvant chemotherapy and radiotherapy in patients with cervical adenocarcinoma of the uterus after radical hysterectomy: SGSG/TGCU Inter group surveillance. Eur J Gynaecol Oncol. 2013; 34:425–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of postoperative adjuvant platinum-based chemotherapy and no further therapy after radical surgery in intermediate-risk early-stage cervical cancer
- Adjuvant pelvic radiation versus observation in intermediate-risk early-stage cervical cancer patients following primary radical surgery: a propensity score-adjusted analysis
- Chemoradiotherapy is not superior to radiotherapy alone after radical surgery for cervical cancer patients with intermediate-risk factor
- Baseline risk of recurrence in stage I–II endometrial carcinoma
- Diagnostic Whole-Body Scan May Not Be Necessary for Intermediate-Risk Patients with Differentiated Thyroid Cancer after Low-Dose (30 mCi) Radioactive Iodide Ablation