Ann Hepatobiliary Pancreat Surg.
2021 Feb;25(1):18-24. 10.14701/ahbps.2021.25.1.18.
How successful is liver resection for colorectal cancer liver metastases in patients over 75 years old?
- Affiliations
-
- 1Cardiff Liver Unit, University Hospital of Wales, UK
- 2Cardiff University School of Medicine, Cardiff, UK
- 3Department of Surgery, Moritz Kaposi Teaching General Hospital, Kaposvár, Hungary
- 4Department of Surgery, Tan Tock Seng Hospital, Singapore
- KMID: 2513171
- DOI: http://doi.org/10.14701/ahbps.2021.25.1.18
Abstract
- Backgrounds/Aims
As populations age, an increased incidence of colorectal cancer will generate an increase in colorectal cancer liver metastases (CRLM). In order to guide treatment decisions, this study aimed to identify the contemporary complication rates of elderly patients undergoing liver resection for CRLM in a, centralised, UK centre.
Methods
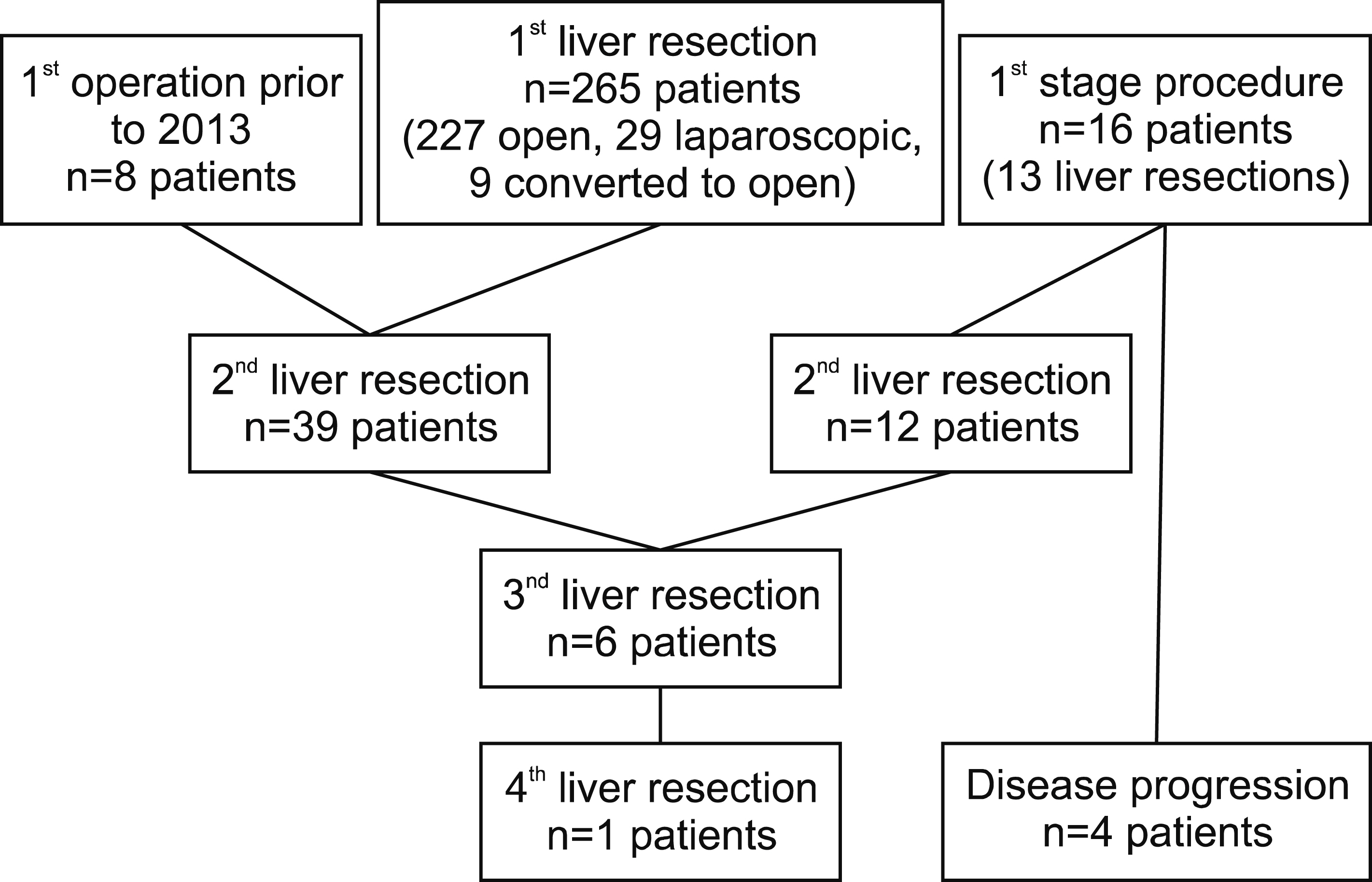
All patients undergoing operative procedures for CRLM between January 2013 and January 2019 were included. Patient, tumour and operative data were analysed, including the prognostic marker; tumour burden score.
Results
339 operations were performed on 289 consecutive patients with CRLM (272 patients <75 years old, 67 patients ≥75 years old). Median age was 66 years (range 20-93). There was no difference in major complication rates between the two age cohorts (6.65 vs. 6.0%, p=0.847) or operative mortality (1.1% vs. 1.4%, p=0.794). Younger patients had higher R1 resection rates (20.4% vs. 4.5%,p=0.002) and post-operative chemotherapy rates (60.3% vs. 35.8%,p< 0.001). The 1, 3 and 5-year OS was 90.2%, 70.5% and 52.3% respectively, median 70 months, with no difference between age cohorts (p=0.772). Tumour Burden score and operation type were independent predictors of overall survival.
Conclusions
Liver resection for CRLM in patients 75 years and older is feasible, safe and confers a similar 5-year survival rate to younger patients. The current outcomes from surgery are better than historical datasets.
Keyword
Figure
Reference
-
1. Office for National Statistics. 2018. National Population Projections: 2016-based statistical bulletin. Office for National Statistics;Newport: Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/bulletins/nationalpopulationprojections/2016 basedstatisticalbulletin. cited 2020 Jan 10.2. Cancer Research UK. 2020. Bowel cancer incidence statistics 2018. Cancer Research UK;London: Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/bowel-cancer/incidence#heading-One. cited 2020 Jan 10.3. Engstrand J, Nilsson H, Strömberg C, Jonas E, Freedman J. 2018; Colorectal cancer liver metastases - a population-based study on incidence, management and survival. BMC Cancer. 18:78. DOI: 10.1186/s12885-017-3925-x. PMID: 29334918. PMCID: PMC5769309.
Article4. Hackl C, Neumann P, Gerken M, Loss M, Klinkhammer-Schalke M, Schlitt HJ. 2014; Treatment of colorectal liver metastases in Germany: a ten-year population-based analysis of 5772 cases of primary colorectal adenocarcinoma. BMC Cancer. 14:810. DOI: 10.1186/1471-2407-14-810. PMID: 25369977. PMCID: PMC4230526.
Article5. Booth CM, Nanji S, Wei X, Mackillop WJ. 2015; Management and outcome of colorectal cancer liver metastases in elderly patients: a population-based study. JAMA Oncol. 1:1111–1119. DOI: 10.1001/jamaoncol.2015.2943. PMID: 26355283.6. Kumar N, Duncan T, O'Reilly D, Káposztás Z, Parry C, Rees J, et al. 2019; Partial ALPPS with a longer wait between procedures is safe and yields adequate future liver remnant hypertrophy. Ann Hepatobiliary Pancreat Surg. 23:13–19. DOI: 10.14701/ahbps.2019.23.1.13. PMID: 30863803. PMCID: PMC6405373.
Article7. Sasaki K, Morioka D, Conci S, Margonis GA, Sawada Y, Ruzzenente A, et al. 2018; The Tumor Burden Score: a new "Metro-ticket" prognostic tool for colorectal liver metastases based on tumor size and number of tumors. Ann Surg. 267:132–141. DOI: 10.1097/SLA.0000000000002064. PMID: 27763897.8. Studer P, Horn T, Haynes A, Candinas D, Banz VM. 2018; Quality of life after hepatic resection. Br J Surg. 105:237–243. DOI: 10.1002/bjs.10735. PMID: 29405277.
Article9. van Tuil T, Dhaif AA, Te Riele WW, van Ramshorst B, van Santvoort HC. 2019; Systematic review and meta-analysis of liver resection for colorectal metastases in elderly patients. Dig Surg. 36:111–123. DOI: 10.1159/000487274. PMID: 29502126.
Article10. Cook EJ, Welsh FK, Chandrakumaran K, John TG, Rees M. 2012; Resection of colorectal liver metastases in the elderly: does age matter? Colorectal Dis. 14:1210–1216. DOI: 10.1111/j.1463-1318.2012.02946.x. PMID: 22251850.
Article11. Filmann N, Walter D, Schadde E, Bruns C, Keck T, Lang H, et al. 2019; Mortality after liver surgery in Germany. Br J Surg. 106:1523–1529. DOI: 10.1002/bjs.11236. PMID: 31339558.
Article12. Munker S, Gerken M, Fest P, Ott C, Schnoy E, Fichtner-Feigl S, et al. 2018; Chemotherapy for metastatic colon cancer: no effect on survival when the dose is reduced due to side effects. BMC Cancer. 18:455. DOI: 10.1186/s12885-018-4380-z. PMID: 29685155. PMCID: PMC5913883.
Article13. Mauri D, Filis P, Tsali L, Zarkavelis G, Pentheroudakis G. 2018; Role of chemotherapy in resectable liver metastases from colorectal cancer: food for thought from pooled evidence. ESMO Open. 3:e000367. DOI: 10.1136/esmoopen-2018-000367. PMID: 29942665. PMCID: PMC6012563.
Article14. Wang Y, Wang ZQ, Wang FH, Yuan YF, Li BK, Ding PR, et al. 2017; The role of adjuvant chemotherapy for colorectal liver metastasectomy after pre-operative chemotherapy: is the treatment worthwhile? J Cancer. 8:1179–1186. DOI: 10.7150/jca.18091. PMID: 28607592. PMCID: PMC5463432.
Article15. Dunne DF, Jack S, Jones RP, Jones L, Lythgoe DT, Malik HZ, et al. 2016; Randomized clinical trial of prehabilitation before planned liver resection. Br J Surg. 103:504–512. DOI: 10.1002/bjs.10096. PMID: 26864728.
Article16. Melloul E, Hübner M, Scott M, Snowden C, Prentis J, Dejong CH, et al. 2016; Guidelines for perioperative care for liver surgery: Enhanced Recovery After Surgery (ERAS) Society recommendations. World J Surg. 40:2425–2440. DOI: 10.1007/s00268-016-3700-1. PMID: 27549599.
Article