J Korean Med Sci.
2021 Feb;36(7):e48. 10.3346/jkms.2021.36.e48.
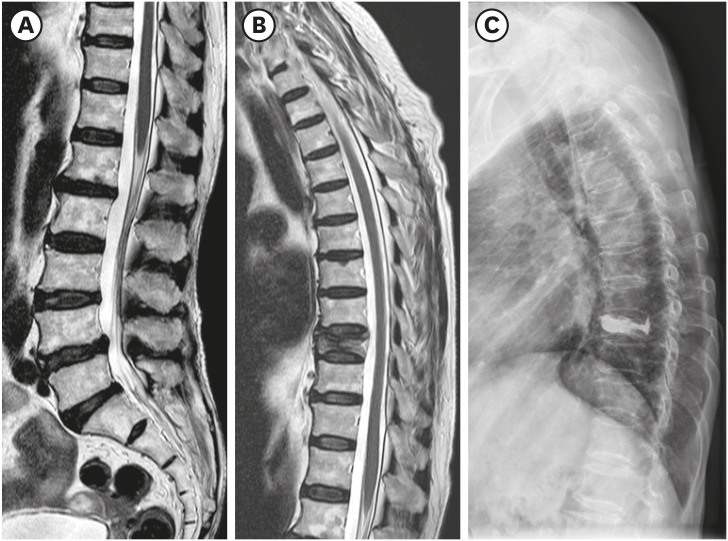
Coexisting Spine Lesions on Whole Spine T2 Sagittal MRI in Evaluating Spinal Degenerative Disease
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Orthopedic Surgery, Seoul National University College of Medicine, SMG-SNU Boramae Medical Center, Seoul, Korea
- KMID: 2513072
- DOI: http://doi.org/10.3346/jkms.2021.36.e48
Abstract
- Background
Studies have reported on the usefulness of whole spine magnetic resonance imaging (MRI) in evaluating specific diseases such as spinal tuberculosis, spinal trauma, spondyloarthropathies, and multiple myeloma. In studies concerning degenerative spinal disease, sample sizes were small and some did not provide information on how symptomatic coexisting lesions were treated. We evaluated the types and prevalence of coexisting spine lesions found on whole spine T2 sagittal screening performed at the time of routine cervical and lumbar spine MRI and evaluated the efficacy of such screening in degenerative diseases of the cervical and lumbar spine.
Methods
We reviewed 1,757 and 2,266 consecutive cases where whole spine T2 sagittal screening had been performed with routine cervical and lumbar spine MRI, respectively, in patients with cervical and lumbar spinal degenerative diseases. Coexisting spine lesions were documented and statistical analysis was performed to investigate significant differences according to sex, age, and initial diagnosis. Electronic medical records were reviewed to determine whether additional interventions were necessary following such findings.
Results
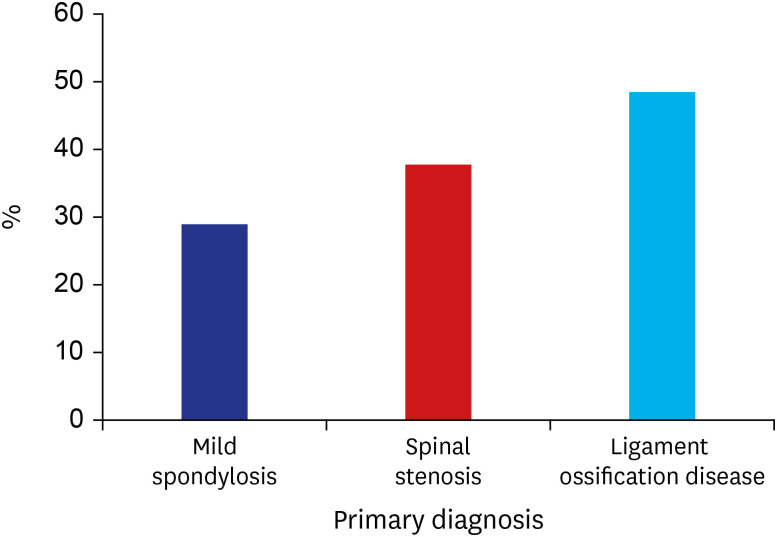
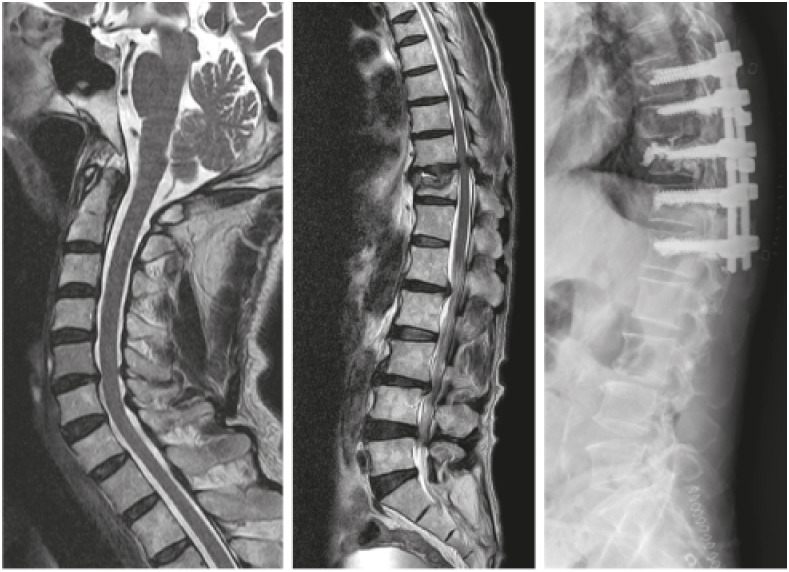
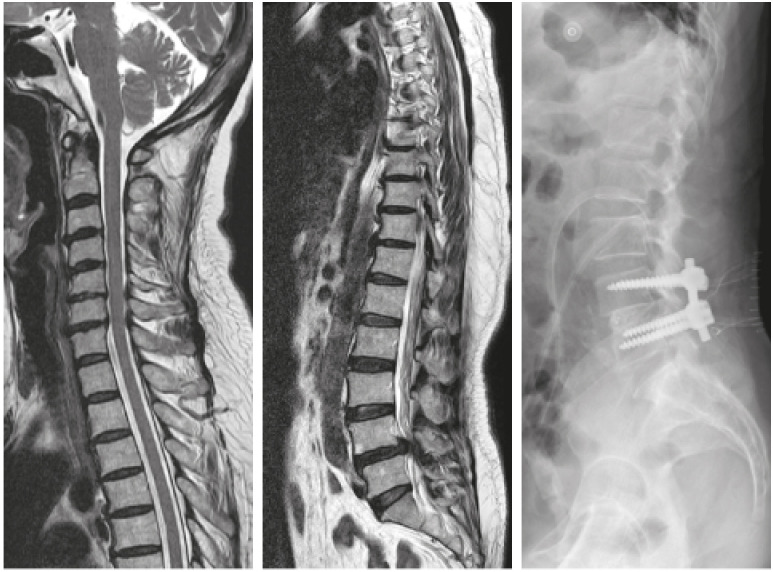
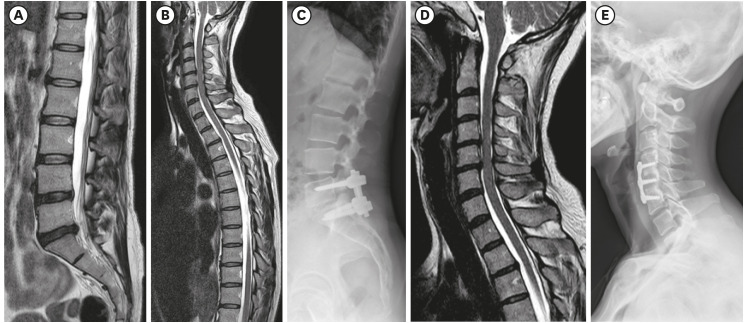
We reviewed 1,252 and 1,689 consecutive cases of routine cervical and lumbar spine MRI respectively, with whole spine T2 sagittal screening. Of the 1,252, 419 (33.5%) patients with cervical spinal degenerative disease had coexisting lesions in the thoracolumbar spine. Patients with ligament ossification disease of the cervical spine showed a higher prevalence of coexisting spine lesions. Sixty of the 419 (14.3%) patients with coexisting spine lesions warranted additional intervention or surgical treatment. Four hundred and eighty-one of 1,689 (28.5%) patients with lumbar degenerative disease had coexisting spine lesions in the cervicothoracic spine. Forty-eight of the 481 (10.0%) patients with coexisting spine lesions warranted additional intervention. In both patient groups, older patients showed a significantly higher prevalence of coexisting spine lesions than younger patients.
Conclusion
Considering the minimal extra time and cost in performing whole spine screening, its application to routine spine MRI can be considered in evaluating cervical and lumbar spinal degenerative diseases.
Figure
Reference
-
1. Flanders AE, Spettell CM, Friedman DP, Marino RJ, Herbison GJ. The relationship between the functional abilities of patients with cervical spinal cord injury and the severity of damage revealed by MR imaging. AJNR Am J Neuroradiol. 1999; 20(5):926–934. PMID: 10369368.2. Yamashita Y, Takahashi M, Matsuno Y, Sakamoto Y, Oguni T, Sakae T, et al. Chronic injuries of the spinal cord: assessment with MR imaging. Radiology. 1990; 175(3):849–854. PMID: 2343135.
Article3. Shah LM, Ross JS. Imaging of degenerative and infectious conditions of the spine. Neurosurgery. 2016; 79(3):315–335. PMID: 27352276.
Article4. Hou YN, Ding WY, Shen Y, Yang DL, Wang LF, Zhang P. Meta-analysis of magnetic resonance imaging for the differential diagnosis of spinal degeneration. Int J Clin Exp Med. 2015; 8(8):11947–11957. PMID: 26550109.5. Schmitz A, Jaeger UE, Koenig R, Kandyba J, Wagner UA, Giesecke J, et al. A new MRI technique for imaging scoliosis in the sagittal plane. Eur Spine J. 2001; 10(2):114–117. PMID: 11345631.
Article6. Althoff CE, Appel H, Rudwaleit M, Sieper J, Eshed I, Hamm B, et al. Whole-body MRI as a new screening tool for detecting axial and peripheral manifestations of spondyloarthritis. Ann Rheum Dis. 2007; 66(7):983–985. PMID: 17576787.
Article7. Green RA, Saifuddin A. Whole spine MRI in the assessment of acute vertebral body trauma. Skeletal Radiol. 2004; 33(3):129–135. PMID: 14740183.8. Kaila R, Malhi AM, Mahmood B, Saifuddin A. The incidence of multiple level noncontiguous vertebral tuberculosis detected using whole spine MRI. J Spinal Disord Tech. 2007; 20(1):78–81. PMID: 17285057.
Article9. Dutoit JC, Vanderkerken MA, Verstraete KL. Value of whole body MRI and dynamic contrast enhanced MRI in the diagnosis, follow-up and evaluation of disease activity and extent in multiple myeloma. Eur J Radiol. 2013; 82(9):1444–1452. PMID: 23726124.
Article10. Overley SC, Kim JS, Gogel BA, Merrill RK, Hecht AC. Tandem spinal stenosis: a systematic review. JBJS Rev. 2017; 5(9):e2.11. Kanna RM, Kamal Y, Mahesh A, Venugopal P, Shetty AP, Rajasekaran S. The impact of routine whole spine MRI screening in the evaluation of spinal degenerative diseases. Eur Spine J. 2017; 26(8):1993–1998. PMID: 28110361.
Article12. Han IH, Suh SH, Kuh SU, Chin DK, Kim KS. Types and prevalence of coexisting spine lesions on whole spine sagittal MR images in surgical degenerative spinal diseases. Yonsei Med J. 2010; 51(3):414–420. PMID: 20376895.
Article13. Bednarik J, Kadanka Z, Dusek L, Novotny O, Surelova D, Urbanek I, et al. Presymptomatic spondylotic cervical cord compression. Spine. 2004; 29(20):2260–2269. PMID: 15480138.
Article14. Teng P, Papatheodorou C. Combined cervical and lumbar spondylosis. Arch Neurol. 1964; 10(3):298–307. PMID: 14106986.
Article15. LaBan MM, Green ML. Concurrent (tandem) cervical and lumbar spinal stenosis: a 10-yr review of 54 hospitalized patients. Am J Phys Med Rehabil. 2004; 83(3):187–190. PMID: 15043352.16. Park MS, Moon SH, Kim TH, Oh JK, Lyu HD, Lee JH, et al. Asymptomatic stenosis in the cervical and thoracic spines of patients with symptomatic lumbar stenosis. Global Spine J. 2015; 5(5):366–371. PMID: 26430589.
Article17. Cho NH, Jung YO, Lim SH, Chung CK, Kim HA. The prevalence and risk factors of low back pain in rural community residents of Korea. Spine (Phila Pa 1976). 2012; 37(24):2001–2010. PMID: 22588379.
Article18. Yamada T, Yoshii T, Yamamoto N, Hirai T, Inose H, Kato T, et al. Clinical outcomes of cervical spinal surgery for cervical myelopathic patients with coexisting lumbar spinal canal stenosis (tandem spinal stenosis): a retrospective analysis of 297 cases. Spine (Phila Pa 1976). 2018; 43(4):E234–E241. PMID: 28614282.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Types and Prevalence of Coexisting Spine Lesions on Whole Spine Sagittal MR Images in Surgical Degenerative Spinal Diseases
- Clinical Utility of Limited T2-Weighted-Only Lumbar Spine MRI in Pain Intervention Clinics
- Efficacy of Dynamic Radiographs in Routine Evaluations for Degenerative Cervical Spine Disease
- The Value of Additional Cervicothoracic Spine Sagittal T2-weighted Images Included in Routine Lumbar Spine MR Imaging
- Spino-Pelvic Parameters in Adult Spinal Deformities