Impact of the COVID-19 Outbreak on Trends in Emergency Department Utilization in Children: a Multicenter Retrospective Observational Study in Seoul Metropolitan Area, Korea
- Affiliations
-
- 1Department of Emergency Medicine, Seoul National University Hospital, Seoul, Korea
- 2Department of Emergency Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Emergency Medicine, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 4Department of Emergency Medicine, Samsung Medical Center, Seoul, Korea
- 5Department of Emergency Medicine, Ajou University School of Medicine, Suwon, Korea
- KMID: 2512466
- DOI: http://doi.org/10.3346/jkms.2021.36.e44
Abstract
- Background
Understanding the changes in emergency department (ED) visit patterns during the coronavirus disease 2019 (COVID-19) outbreak is important for effectively operating EDs during the pandemic. We aimed to analyze the changes in pediatric ED visits during the COVID-19 pandemic and examine the relationship between the number of ED visits and the stringency of government social distancing measures.
Methods
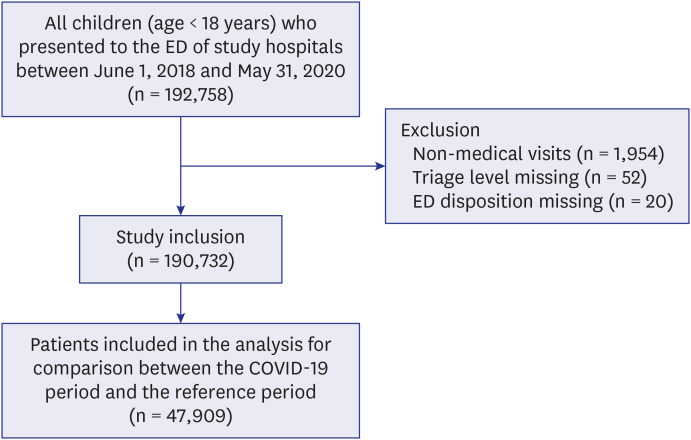
This multicenter retrospective study used data of pediatric (age < 18 years) ED visits in Seoul metropolitan area from June 1, 2018, to May 31, 2020. Patient demographics, ED results, and diagnoses were compared during the COVID-19 period and the previous year.To evaluate the effect of the stringency of social distancing measures on the number of ED visits, a Poisson regression model was developed with month, year, and the average monthly Government Response Stringency Index (GRSI) as fixed effects.
Results
In total, 190,732 patients were included. The number of pediatric ED visits during the COVID-19 period was 58.1% lower than in the previous year. There were disproportionate decreases in the numbers of ED visits for children in early childhood (66.5%), low-acuity children (55.2-63.8%), those who did not use an ambulance (59.0%), and those visiting the ED for noninjury complaints (64.9%). The proportion of admissions increased from 11.9% to 16.6%. For every 10-point increase in the GRSI, there was a 15.1% decrease in monthly ED visits.
Conclusion
A striking decrease in pediatric ED visits was observed during the COVID-19 outbreak, the scale which was associated with the stringency of government policies. Changes in the number and characteristics of children visiting the ED should be considered to facilitate the effective operation of EDs during the pandemic.
Keyword
Figure
Cited by 7 articles
-
Changes in the Occurrence of Gastrointestinal Infections after COVID-19 in Korea
So Yun Ahn, Ji Young Park, In Seok Lim, Soo Ahn Chae, Sin Weon Yun, Na Mi Lee, Su Yeong Kim, Byung Sun Choi, Dae Yong Yi
J Korean Med Sci. 2021;36(24):e180. doi: 10.3346/jkms.2021.36.e180.Long-term impact of coronavirus disease 2019 pandemic on emergency department utilization in a metropolitan emergency department in Korea
Seung Yeon Hwang, Jae Kwang Lee, Hyun Sik Ryu, Seong Soo Park, Jun Young Choi, Hye Ji Lee, Seung Ho Hur, Yeong Geun Park, Hyun Soo Choi
Pediatr Emerg Med J. 2021;8(2):57-65. doi: 10.22470/pemj.2021.00346.Impact of Social Distancing on Intussusception Incidence in Children
Young June Choe, Yoon Lee, Jung Ok Shim
J Korean Med Sci. 2021;37(2):e16. doi: 10.3346/jkms.2022.37.e16.Effect of coronavirus disease 2019 pandemic on children’s visits to the emergency department
Hong Min Kim, Sang Ook Ha, Won Seok Yang, Young Sun Park, Jin Hyouk Kim
Pediatr Emerg Med J. 2022;9(1):10-16. doi: 10.22470/pemj.2021.00381.Coronavirus disease 2019 pandemic-related change in children’s visits to the emergency department
Dae Ho Kang
Pediatr Emerg Med J. 2022;9(1):29-34. doi: 10.22470/pemj.2022.00451.Changes in pediatric psychiatric emergency during the coronavirus disease 2019 pandemic
Jung Il Kwak, Jun Sung Park, Seung Jun Choi, Jong Seung Lee, Jeong-Min Ryu, Jeong-Yong Lee
Pediatr Emerg Med J. 2022;9(1):35-40. doi: 10.22470/pemj.2022.00465.Changes in emergency department utilization by neonates during the coronavirus disease 2019 pandemic: a single-center study in Korea
Sung Hee Lee, Shin Won Yoon, Ju Hyun Jin
Pediatr Emerg Med J. 2024;11(3):107-114. doi: 10.22470/pemj.2024.00976.
Reference
-
1. WHO. World Health Organization coronavirus disease (COVID-2019) situation report - 186. Updated 2020. Accessed July 24, 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports.2. Korean Society of Infectious Diseases. Korean Society of Pediatric Infectious Diseases. Korean Society of Epidemiology. Korean Society for Antimicrobial Therapy. Korean Society for Healthcare-associated Infection Control and Prevention. Korea Centers for Disease Control and Prevention. Report on the epidemiological features of coronavirus disease 2019 (COVID-19) outbreak in the Republic of Korea from January 19 to March 2, 2020. J Korean Med Sci. 2020; 35(10):e112. PMID: 32174069.3. KCDC. Updates on COVID-19 in Republic of Korea, 23 July 2020. Updated 2020. Accessed July 25, 2020. http://ncov.mohw.go.kr/en/tcmBoardList.do?brdId=12&brdGubun=125&dataGubun=&ncvContSeq=&contSeq=&board_id=.4. Jang WM, Jang DH, Lee JY. Social distancing and transmission-reducing practices during the 2019 coronavirus disease and 2015 Middle East respiratory syndrome coronavirus outbreaks in Korea. J Korean Med Sci. 2020; 35(23):e220. PMID: 32537955.
Article5. Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, et al. Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(23):699–704. PMID: 32525856.
Article6. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020; 4(5):e10–1. PMID: 32278365.
Article7. Westgard BC, Morgan MW, Vazquez-Benitez G, Erickson LO, Zwank MD. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med. 2020; 76(5):595–601. PMID: 33008651.
Article8. Huang CC, Yen DH, Huang HH, Kao WF, Wang LM, Huang CI, et al. Impact of severe acute respiratory syndrome (SARS) outbreaks on the use of emergency department medical resources. J Chin Med Assoc. 2005; 68(6):254–259. PMID: 15984818.
Article9. Paek SH, Kim DK, Lee JH, Kwak YH. The impact of Middle East respiratory syndrome outbreak on trends in emergency department utilization patterns. J Korean Med Sci. 2017; 32(10):1576–1580. PMID: 28875599.
Article10. Comelli I, Scioscioli F, Cervellin G. Impact of the COVID-19 epidemic on census, organization and activity of a large urban emergency department. Acta Biomed. 2020; 91(2):45–49.11. Chaiyachati BH, Agawu A, Zorc JJ, Balamuth F. Trends in pediatric emergency department utilization after institution of COVID-19 mandatory social distancing. J Pediatr. 2020; 226:274–277.e1.12. Hong KJ, Shin SD, Ro YS, Song KJ, Singer AJ. Development and validation of the excess mortality ratio-based Emergency Severity Index. Am J Emerg Med. 2012; 30(8):1491–1500. PMID: 22381578.
Article13. Islam N, Sharp SJ, Chowell G, Shabnam S, Kawachi I, Lacey B, et al. Physical distancing interventions and incidence of coronavirus disease 2019: natural experiment in 149 countries. BMJ. 2020; 370:m2743. PMID: 32669358.
Article14. Hale T, Angrist N, Boby T, Cameron-Blake E, Hallas L, Kira B, et al. Oxford COVID-19 government response tracker. Updated 2020. Accessed July 24, 2020. http://www.bsg.ox.ac.uk/covidtracker.15. Williams K, Thomson D, Seto I, Contopoulos-Ioannidis DG, Ioannidis JP, Curtis S, et al. Standard 6: age groups for pediatric trials. Pediatrics. 2012; 129(Suppl 3):S153–60. PMID: 22661762.
Article16. Shin HY, Lee JY, Kim JE, Lee S, Youn H, Kim H, et al. Cause-of-death statistics in 2016 in the Republic of Korea. J Korean Med Assoc. 2018; 61(9):573–584.
Article17. Kim HB, Kim DK, Kwak YH, Shin SD, Song KJ, Lee SC, et al. Epidemiology of traumatic head injury in Korean children. J Korean Med Sci. 2012; 27(4):437–442. PMID: 22468109.
Article18. Wong LE, Hawkins JE, Langness S, Murrell KL, Iris P, Sammann A. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catal. Forthcoming. 2020.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of regional COVID-19 outbreak to emergency department response on acute myocardial infarction: a multicenter retrospective study
- Impact of COVID-19 pandemic on emergency department visits during daytime and nighttime
- Food service industry in the era of COVID-19: trends and research implications
- The Effects of COVID-19 on the Self-Harm in Children and Adolescents Observed in a University Hospital
- Impact of the COVID-19 Pandemic on Gastric Cancer Screening in South Korea: Results From the Korean National Cancer Screening Survey (2017–2021)