J Korean Med Sci.
2021 Feb;36(5):e29. 10.3346/jkms.2021.36.e29.
The Impact of Erosive Reflux Esophagitis on the Decline of Lung Function in the General Population
- Affiliations
-
- 1Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 2Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Veterans Health Service Medical Center, Seoul, Korea
- 3Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Kang Dong Sacred Hospital, Seoul, Korea
- 4Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Serim General Hospital, Incheon, Korea
- 5Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 6Department of Internal Medicine, Healthcare Research Institute, Healthcare System Gangnam Center, Seoul National University Hospital, Seoul, Korea
- KMID: 2512461
- DOI: http://doi.org/10.3346/jkms.2021.36.e29
Abstract
- Background
The impact of reflux esophagitis on the decline of lung function has been rarely reported. This study was performed to evaluate the association between erosive reflux esophagitis and lung function changes.
Methods
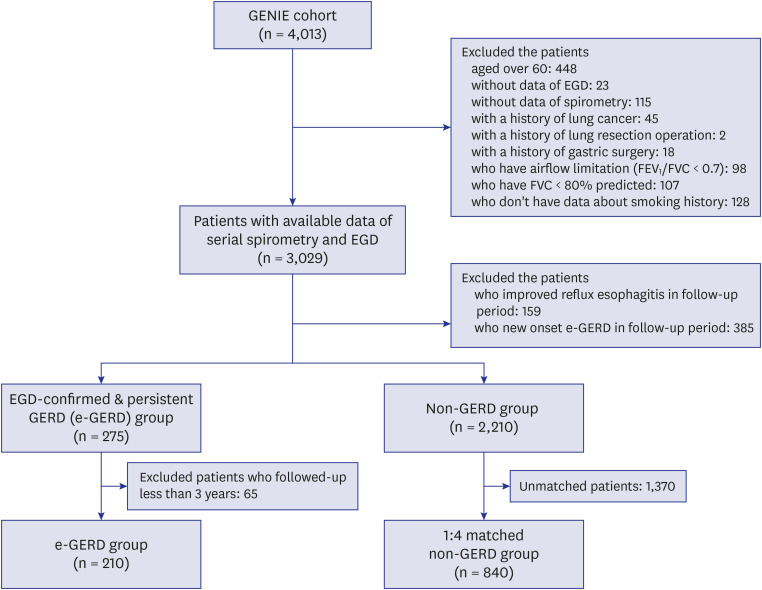
We included patients with normal lung function who underwent esophagogastroduodenoscopy for health screening from a health screening center. Patients with persistent erosive reflux esophagitis on two discrete endoscopic examinations were designated as the erosive reflux esophagitis group. We also selected patients without erosive reflux esophagitis and matched them 1:4 with patients from the erosive reflux esophagitis group. We estimated annual forced expiratory volume in 1 second (FEV1 ) and forced vital capacity (FVC) changes from baseline and compared these estimates by the linear mixed regression model. We also estimated the biannual incidence of chronic obstructive pulmonary disease (COPD).
Results
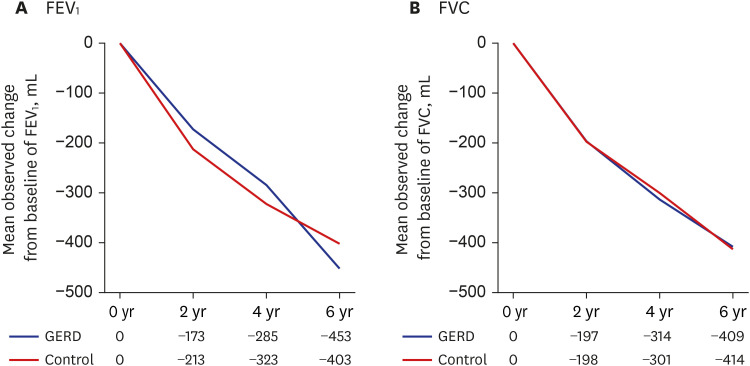
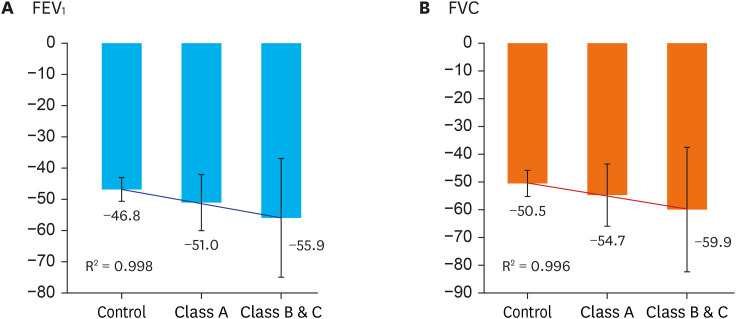
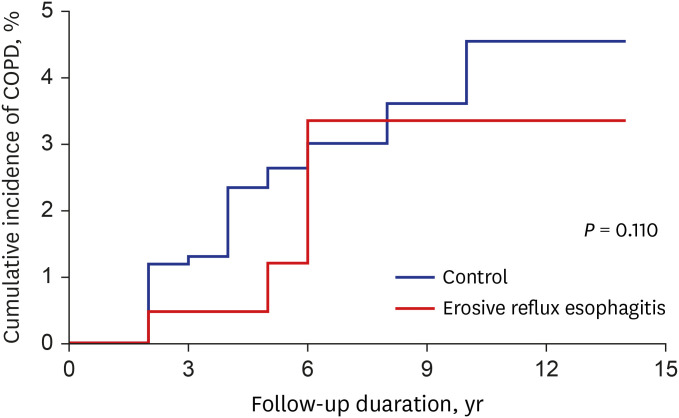
In total, 1,050 patients (210 patients with erosive reflux esophagitis, and 840 matched controls) were included. The median follow-up duration for spirometry was six years. In patients with erosive reflux esophagitis, mild reflux esophagitis (A grade) was most common (165 patients, 78.6%). The adjusted annual FEV1 change in patients with erosive reflux esophagitis was −51.8 mL/yr, while it decreased by 46.8 mL/yr in controls (P = 0.270).The adjusted annual FVC decline was similar between the two groups (−55.8 vs. −50.5 mL/ yr, P = 0.215). The estimated COPD incidence during the follow-up period was not different between the erosive reflux esophagitis and control groups.
Conclusion
In patients with normal lung function, the presence of erosive reflux esophagitis did not affect the annual declines in FEV1 or FVC.
Keyword
Figure
Reference
-
1. Vakil N. Disease definition, clinical manifestations, epidemiology and natural history of GERD. Best Pract Res Clin Gastroenterol. 2010; 24(6):759–764. PMID: 21126691.
Article2. Gaude GS. Pulmonary manifestations of gastroesophageal reflux disease. Ann Thorac Med. 2009; 4(3):115–123. PMID: 19641641.
Article3. Field SK. A critical review of the studies of the effects of simulated or real gastroesophageal reflux on pulmonary function in asthmatic adults. Chest. 1999; 115(3):848–856. PMID: 10084501.
Article4. Iliaz S, Iliaz R, Onur ST, Arici S, Akyuz U, Karaca C, et al. Does gastroesophageal reflux increase chronic obstructive pulmonary disease exacerbations? Respir Med. 2016; 115:20–25. PMID: 27215499.
Article5. Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006; 101(8):1900–1920. PMID: 16928254.
Article6. Nemzek JA, Kim J. Pulmonary inflammation and airway hyperresponsiveness in a mouse model of asthma complicated by acid aspiration. Comp Med. 2009; 59(4):321–330. PMID: 19712571.7. Ravelli AM, Panarotto MB, Verdoni L, Consolati V, Bolognini S. Pulmonary aspiration shown by scintigraphy in gastroesophageal reflux-related respiratory disease. Chest. 2006; 130(5):1520–1526. PMID: 17099032.
Article8. Araujo AC, Aprile LR, Dantas RO, Terra-Filho J, Vianna EO. Bronchial responsiveness during esophageal acid infusion. Lung. 2008; 186(2):123–128. PMID: 18297339.
Article9. Lozo Vukovac E, Lozo M, Mise K, Gudelj I, Puljiz Ž, Jurcev-Savicevic A, et al. Bronchoalveolar pH and inflammatory biomarkers in newly diagnosed IPF and GERD patients: a case-control study. Med Sci Monit. 2014; 20:255–261. PMID: 24535066.
Article10. Wright RA, Miller SA, Corsello BF. Acid-induced esophagobronchial-cardiac reflexes in humans. Gastroenterology. 1990; 99(1):71–73. PMID: 2344943.
Article11. Savarino E, Carbone R, Marabotto E, Furnari M, Sconfienza L, Ghio M, et al. Gastro-oesophageal reflux and gastric aspiration in idiopathic pulmonary fibrosis patients. Eur Respir J. 2013; 42(5):1322–1331. PMID: 23471347.
Article12. Morehead RS. Gastro-oesophageal reflux disease and non-asthma lung disease. Eur Respir Rev. 2009; 18(114):233–243. PMID: 20956148.
Article13. Kiljander TO, Laitinen JO. The prevalence of gastroesophageal reflux disease in adult asthmatics. Chest. 2004; 126(5):1490–1494. PMID: 15539717.
Article14. Benson VS, Müllerová H, Vestbo J, Wedzicha JA, Patel A, Hurst JR, et al. Associations between gastro-oesophageal reflux, its management and exacerbations of chronic obstructive pulmonary disease. Respir Med. 2015; 109(9):1147–1154. PMID: 26166017.
Article15. Hu ZW, Wang ZG, Zhang Y, Wu JM, Liu JJ, Lu FF, et al. Gastroesophageal reflux in bronchiectasis and the effect of anti-reflux treatment. BMC Pulm Med. 2013; 13(1):34. PMID: 23731838.
Article16. Kim SW, Lee JH, Sim YS, Ryu YJ, Chang JH. Prevalence and risk factors for reflux esophagitis in patients with chronic obstructive pulmonary disease. Korean J Intern Med. 2014; 29(4):466–473. PMID: 25045294.
Article17. Lee AL, Goldstein RS. Gastroesophageal reflux disease in COPD: links and risks. Int J Chron Obstruct Pulmon Dis. 2015; 10:1935–1949. PMID: 26392769.
Article18. Mandal P, Morice AH, Chalmers JD, Hill AT. Symptoms of airway reflux predict exacerbations and quality of life in bronchiectasis. Respir Med. 2013; 107(7):1008–1013. PMID: 23683772.
Article19. Houghton LA, Lee AS, Badri H, DeVault KR, Smith JA. Respiratory disease and the oesophagus: reflux, reflexes and microaspiration. Nat Rev Gastroenterol Hepatol. 2016; 13(8):445–460. PMID: 27381074.
Article20. Sharifi A, Ansarin K. Effect of gastroesophageal reflux disease on disease severity and characteristics of lung functional changes in patients with asthma. J Cardiovasc Thorac Res. 2014; 6(4):223–228. PMID: 25610553.
Article21. Lee HB, Lee YD, Kim HC, Lee YC, Lee ST, Rhee YK. Relationship between exercise induced asthma and gastroesophageal reflux. Tuberc Respir Dis. 2000; 48(2):203–209.
Article22. Lundell LR, Dent J, Bennett JR, Blum AL, Armstrong D, Galmiche JP, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999; 45(2):172–180. PMID: 10403727.
Article23. Dent J. Endoscopic grading of reflux oesophagitis: the past, present and future. Best Pract Res Clin Gastroenterol. 2008; 22(4):585–599. PMID: 18656818.
Article24. Choi J, Paek D, Lee J. Normal predictive values of spirometry in Korean population. Tuberc Respir Dis. 2005; 58(3):230–242.
Article25. Miller MR, Crapo R, Hankinson J, Brusasco V, Burgos F, Casaburi R, et al. General considerations for lung function testing. Eur Respir J. 2005; 26(1):153–161. PMID: 15994402.26. Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. Interpretative strategies for lung function tests. Eur Respir J. 2005; 26(5):948–968. PMID: 16264058.27. Ali E, Abdelhamid H, Shalaby H. Effect of gastroesophageal reflux disease on spirometry, lung diffusion, and impulse oscillometry. Egypt J Bronchol. 2016; 10(2):189–196.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Barrett Esophagus Associated with Erosive Reflux Esophagitis in a Patient with Hiatal Hernia
- Clinical Spectrum of Endoscopic Reflux Esophagitis in Routine Check-Up Subjects in Korea
- Minimal Change Esophagitis
- Irritable Bowel Syndrome Is Associated With Gastroesophageal Reflux Symptom but Not Erosive Esophagitis
- Gastro-Esophageal Reflux Disease in Healthy Older Children and Adolescents