J Stroke.
2021 Jan;23(1):113-123. 10.5853/jos.2020.03440.
Initiation of Guideline-Matched Oral Anticoagulant in Atrial Fibrillation-Related Stroke
- Affiliations
-
- 1Department of Neurology, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- 2Department of Neurology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Digital Health, Samsung Advanced Institute for Health Sciences & Technology, Sungkyunkwan University, Seoul, Korea
- 4Department of Neurology, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- 5Department of Neurology, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- 6Department of Neurology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 7Department of Neurology, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 8Department of Neurology, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- 9Department of Neurology, Ewha Womans University Seoul Hospital, Ewha Womans University School of Medicine, Seoul, Korea
- 10Department of Neurology, Eunpyeong St. Mary’s Hospital, College of Medicine, The Catholic University of Kore, Seoul, Korea
- 11Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 12Department of Neurology, Kyung Hee University Hospital, Kyung Hee University School of Medicine, Seoul, Korea
- 13Department of Neurology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea
- 14Department of Neurology, Myongji Hospital, Hanyang University College of Medicine, Goyang, Korea
- 15Department of Neurology, Jeju National University Hospital, Jeju National University College of Medicine, Jeju, Korea
- KMID: 2512360
- DOI: http://doi.org/10.5853/jos.2020.03440
Abstract
- Background and Purpose
To evaluate the outcome events and bleeding complications of the European Society of Cardiology (ESC) guideline-matched oral anticoagulant therapy for patients with acute ischemic stroke and atrial fibrillation (AF).
Methods
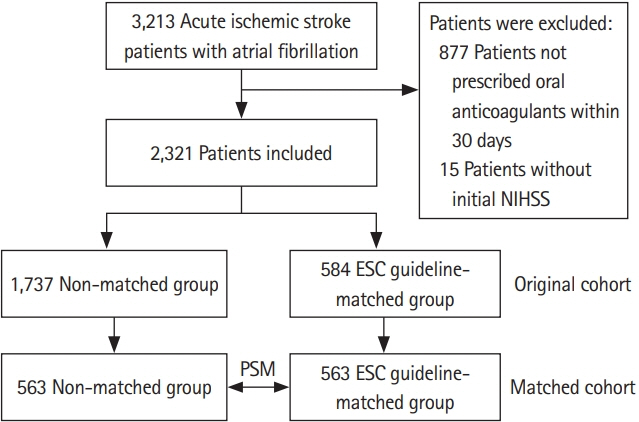
Patients with acute ischemic stroke and AF from a nationwide multicenter registry (Korean ATrial fibrillaTion EvaluatioN regisTry in Ischemic strOke patieNts [K-ATTENTION]) between January 2013 and December 2015 were included in the study. Patients were divided into the ESC guideline-matched and the non-matched groups. The primary outcome was recurrence of any stroke during the 90-day follow-up period. Secondary outcomes were major adverse cerebrovascular and cardiovascular events, ischemic stroke, intracranial hemorrhage, acute coronary syndrome, allcause mortality, and major hemorrhage. Propensity score matching and logistic regression analyses were performed to assess the effect of the treatments administered.
Results
Among 2,321 eligible patients, 1,126 patients were 1:1 matched to the ESC guidelinematched and the non-matched groups. As compared with the non-matched group, the ESC guideline-matched group had a lower risk of any recurrent stroke (1.4% vs. 3.4%; odds ratio [OR], 0.41; 95% confidence interval [CI], 0.18 to 0.95). The risk of recurrent ischemic stroke was lower in the ESC guideline-matched group than in the non-matched group (0.9% vs. 2.7%; OR, 0.32; 95% CI, 0.11 to 0.88). There was no significant difference in the other secondary outcomes between the two groups.
Conclusions
ESC guideline-matched oral anticoagulant therapy was associated with reduced risks of any stroke and ischemic stroke as compared with the non-matched therapy.
Keyword
Figure
Reference
-
References
1. Hart RG, Pearce LA, Aguilar MI. Meta-analysis: antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann Intern Med. 2007; 146:857–867.
Article2. Saxena R, Koudstaal P. Anticoagulants versus antiplatelet therapy for preventing stroke in patients with nonrheumatic atrial fibrillation and a history of stroke or transient ischemic attack. Cochrane Database Syst Rev. 2004; 4:CD000187.
Article3. Hart RG, Coull BM, Hart D. Early recurrent embolism associated with nonvalvular atrial fibrillation: a retrospective study. Stroke. 1983; 14:688–693.
Article4. D’Amelio M, Terruso V, Famoso G, Di Benedetto N, Realmuto S, Valentino F, et al. Early and late mortality of spontaneous hemorrhagic transformation of ischemic stroke. J Stroke Cerebrovasc Dis. 2014; 23:649–654.5. Hong KS, Kwon SU, Lee SH, Lee JS, Kim YJ, Song TJ, et al. Rivaroxaban vs warfarin sodium in the ultra-early period after atrial fibrillation-related mild ischemic stroke: a randomized clinical trial. JAMA Neurol. 2017; 74:1206–1215.6. Butcher KS, Ng K, Sheridan P, Field TS, Coutts SB, Siddiqui M, et al. Dabigatran treatment of acute noncardioembolic ischemic stroke. Stroke. 2020; 51:1190–1198.
Article7. Wilson D, Ambler G, Banerjee G, Shakeshaft C, Cohen H, Yousry TA, et al. Early versus late anticoagulation for ischaemic stroke associated with atrial fibrillation: multicentre cohort study. J Neurol Neurosurg Psychiatry. 2019; 90:320–325.
Article8. Paciaroni M, Agnelli G, Falocci N, Tsivgoulis G, Vadikolias K, Liantinioti C, et al. Early recurrence and major bleeding in patients with acute ischemic stroke and atrial fibrillation treated with non-vitamin-k oral anticoagulants (RAF-NOACs) Study. J Am Heart Assoc. 2017; 6:e007034.
Article9. January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the Heart Rhythm Society. Circulation. 2014; 130:e199–e267.
Article10. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016; 37:2893–2962.
Article11. Ahmed N, Steiner T, Caso V, Wahlgren N; ESO-KSU session participants. Recommendations from the ESO-Karolinska Stroke Update Conference, Stockholm 13-15 November 2016. Eur Stroke J. 2017; 2:95–102.
Article12. Song TJ, Baek IY, Woo HG, Kim YJ, Chang Y, Kim BJ, et al. Characteristics and factors for short-term functional outcome in stroke patients with atrial fibrillation, nationwide retrospective cohort study. Front Neurol. 2019; 10:1101.
Article13. Parsons LS. Performing a 1:N case-control match on propensity score. In : Proceedings of the 29th Annual SAS Users Group International Conference; 2004 May 9-12; Montreal, CA. Cary: SAS Institute. 2004.14. Seiffge DJ, Traenka C, Polymeris A, Hert L, Peters N, Lyrer P, et al. Early start of DOAC after ischemic stroke: risk of intracranial hemorrhage and recurrent events. Neurology. 2016; 87:1856–1862.15. Seiffge DJ, Paciaroni M, Wilson D, Koga M, Macha K, Cappellari M, et al. Direct oral anticoagulants versus vitamin K antagonists after recent ischemic stroke in patients with atrial fibrillation. Ann Neurol. 2019; 85:823–834.
Article16. International Stroke Trial Collaborative Group. The International Stroke Trial (IST): a randomised trial of aspirin, subcutaneous heparin, both, or neither among 19435 patients with acute ischaemic stroke. Lancet. 1997; 349:1569–1581.17. Freedman MD. Oral anticoagulants: pharmacodynamics, clinical indications and adverse effects. J Clin Pharmacol. 1992; 32:196–209.
Article18. Azoulay L, Dell’Aniello S, Simon TA, Renoux C, Suissa S. Initiation of warfarin in patients with atrial fibrillation: early effects on ischaemic strokes. Eur Heart J. 2014; 35:1881–1887.
Article19. Alves HC, Treurniet KM, Jansen IG, Yoo AJ, Dutra BG, Zhang G, et al. Thrombus migration paradox in patients with acute ischemic stroke. Stroke. 2019; 50:3156–3163.
Article20. Gorog DA, Fayad ZA, Fuster V. Arterial thrombus stability: does it matter and can we detect it? J Am Coll Cardiol. 2017; 70:2036–2047.21. Corrado G, Tadeo G, Beretta S, Tagliagambe LM, Manzillo GF, Spata M, et al. Atrial thrombi resolution after prolonged anticoagulation in patients with atrial fibrillation. Chest. 1999; 115:140–143.
Article22. Kaku B. Intra-cardiac thrombus resolution after anti-coagulation therapy with dabigatran in a patient with midventricular obstructive hypertrophic cardiomyopathy: a case report. J Med Case Rep. 2013; 7:238.
Article23. Manning WJ, Silverman DI, Waksmonski CA, Oettgen P, Douglas PS. Prevalence of residual left atrial thrombi among patients with acute thromboembolism and newly recognized atrial fibrillation. Arch Intern Med. 1995; 155:2193–2198.
Article24. Paciaroni M, Bandini F, Agnelli G, Tsivgoulis G, Yaghi S, Furie KL, et al. Hemorrhagic transformation in patients with acute ischemic stroke and atrial fibrillation: time to initiation of oral anticoagulant therapy and outcomes. J Am Heart Assoc. 2018; 7:e010133.25. Xian Y, Xu H, O’Brien EC, Shah S, Thomas L, Pencina MJ, et al. Clinical effectiveness of direct oral anticoagulants vs warfarin in older patients with atrial fibrillation and ischemic stroke: findings from the Patient-Centered Research Into Outcomes Stroke Patients Prefer and Effectiveness Research (PROSPER) Study. JAMA Neurol. 2019; 76:1192–1202.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Practical Issues to Prevent Stroke Associated with Non-valvular Atrial Fibrillation
- Paradoxical Procoagulant Effect of Early Doses of Warfarin: Possible Role of Non-Vitamin K Oral Anticoagulant in Patients with Atrial Fibrillation-Related Stroke
- Tackling Nonatrial Fibrillation Diseases Using Nonvitamin K Antagonist Oral Anticoagulant: by What and for Whom?
- The Mechanism of and Preventive Therapy for Stroke in Patients with Atrial Fibrillation
- Application of New Oral Anticoagulants: Prevention of Stroke in Patients with Nonvalvular Atrial Fibrillation