J Stroke.
2021 Jan;23(1):69-81. 10.5853/jos.2020.02110.
Delayed Lesions on Diffusion-Weighted Imaging in Initially Lesion-Negative Stroke Patients
- Affiliations
-
- 1Department of Neurology and Cerebrovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Lyda Hill Department of Bioinformatics, UT Southwestern Medical Center, Dallas, TX, USA
- 3Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2512356
- DOI: http://doi.org/10.5853/jos.2020.02110
Abstract
- Background and Purpose
Lesions on diffusion-weighted imaging (DWI) occasionally appear on follow-up magnetic resonance imaging (MRI) among initially DWI-negative but clinically suspicious stroke patients. We established the prevalence of positive conversion in DWI-negative stroke and determined the clinical factors associated with it.
Methods
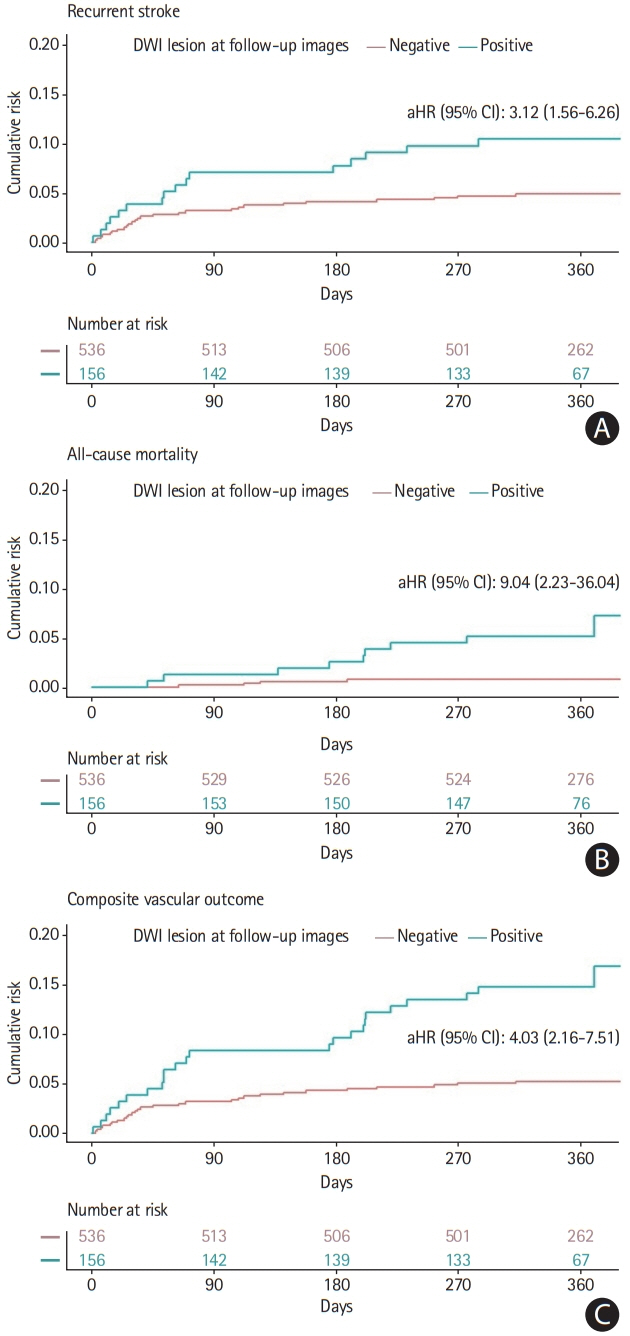
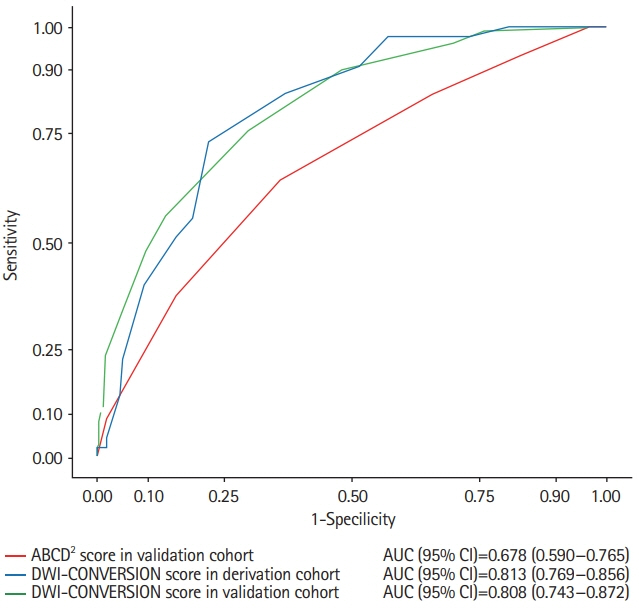
This retrospective, observational, single-center study included 5,271 patients hospitalized due to stroke/transient ischemic attack (TIA) in a single university hospital during 2010 to 2017. Patients without initial DWI lesions underwent follow-up DWI imaging as a routine practice. Adjusted hazard ratios (aHRs) for recurrent stroke risk according to positive conversion were determined using Cox proportional hazard regression. Adjusted odds ratios (aORs) and 95% confidence intervals (CIs) for positive conversion among initially DWI-negative patients were estimated.
Results
In total, 694 (13.2%) patients (mean±standard deviation age, 62.9±13.7 years; male, 404 [58.2%]) were initially DWI-negative. Among them, 22.5% had positive-conversion on follow-up DWI. Positive conversion was associated with a higher risk of recurrent stroke (aHR, 3.12; 95% CI, 1.56 to 6.26). Early neurologic deterioration (aOR, 15.1; 95% CI, 5.71 to 47.66), atrial fibrillation (aOR, 6.17; 95% CI, 3.23 to 12.01), smoking (aOR, 3.76; 95% CI, 2.19 to 6.63), pre-stroke dependency (aOR, 1.62; 95% CI, 1.15 to 2.27), objective hemiparesis (aOR, 4.39; 95% CI, 1.90 to 10.32), longer symptom duration (aOR, 2.17; 95% CI, 1.57 to 3.08), high cholesterol (aOR, 4.70; 95% CI, 1.78 to 12.77), National Institutes of Health Stroke Scale score (aOR, 1.44; 95% CI, 1.08 to 1.91), and high systolic blood pressure (aOR, 1.01; 95% CI, 1.00 to 1.02) were associated with a higher incidence of lesions with delayed appearance. Regarding the location of lesions on follow-up DWI, 34.6% and 21.2% were in the cortex and brainstem, respectively.
Conclusions
In DWI-negative stroke/TIA, positive conversion is associated with a higher risk of recurrent stroke. DWI-negative stroke with factors related to positive conversion may require follow-up MRI for a definitive diagnosis.
Figure
Reference
-
References
1. Easton JD, Saver JL, Albers GW, Alberts MJ, Chaturvedi S, Feldmann E, et al. Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists. Stroke. 2009; 40:2276–2293.2. Edlow BL, Hurwitz S, Edlow JA. Diagnosis of DWI-negative acute ischemic stroke: a meta-analysis. Neurology. 2017; 89:256–262.3. Lövblad KO, Laubach HJ, Baird AE, Curtin F, Schlaug G, Edelman RR, et al. Clinical experience with diffusion-weighted MR in patients with acute stroke. AJNR Am J Neuroradiol. 1998; 19:1061–1066.4. Lutsep HL, Albers GW, DeCrespigny A, Kamat GN, Marks MP, Moseley ME. Clinical utility of diffusion-weighted magnetic resonance imaging in the assessment of ischemic stroke. Ann Neurol. 1997; 41:574–580.
Article5. Oppenheim C, Stanescu R, Dormont D, Crozier S, Marro B, Samson Y, et al. False-negative diffusion-weighted MR findings in acute ischemic stroke. AJNR Am J Neuroradiol. 2000; 21:1434–1440.6. Sylaja PN, Coutts SB, Krol A, Hill MD, Demchuk AM; VISION Study Group. When to expect negative diffusion-weighted images in stroke and transient ischemic attack. Stroke. 2008; 39:1898–1900.
Article7. Chang WL, Lai JC, Chen RF, Hu HH, Pan CS. Case report of false-negative diffusion-weighted image of brain maggnetic resonance imaging (MRI) in acute ischemic stroke. Am J Case Rep. 2017; 18:76–79.
Article8. Seo MJ, Roh SY, Kyun YS, Yu HJ, Cho YK. Diffusion weighted imaging findings in the acute lateral medullary infarction. J Clin Neurol. 2006; 2:107–112.
Article9. Al-Khaled M, Eggers J. MRI findings and stroke risk in TIA patients with different symptom durations. Neurology. 2013; 80:1920–1926.
Article10. Giles MF, Albers GW, Amarenco P, Arsava EM, Asimos AW, Ay H, et al. Early stroke risk and ABCD2 score performance in tissue- vs time-defined TIA: a multicenter study. Neurology. 2011; 77:1222–1228.
Article11. Hurford R, Li L, Lovett N, Kubiak M, Kuker W, Rothwell PM, et al. Prognostic value of “tissue-based” definitions of TIA and minor stroke: population-based study. Neurology. 2019; 92:e2455–e2461.12. Sato M, Nakai Y, Tsurushima H, Shiigai M, Masumoto T, Matsumura A. Risk factors of ischemic lesions related to cerebral angiography and neuro-interventional procedures. Neurol Med Chir (Tokyo). 2013; 53:381–387.
Article13. Obeid T, Awada A. Posterior leukoencephalopathy without severe hypertension: utility of diffusion-weighted MRI. Neurology. 1999; 53:1372–1373.
Article14. Kim BJ, Park JM, Kang K, Lee SJ, Ko Y, Kim JG, et al. Case characteristics, hyperacute treatment, and outcome information from the clinical research center for stroke-fifth division registry in South Korea. J Stroke. 2015; 17:38–53.
Article15. Kim BJ, Kim H, Jeong HG, Yang MH, Jung CK, Han MK, et al. Tenacity of collateral perfusion in proximal cerebral arterial occlusions 6-12 h after onset. Cerebrovasc Dis. 2018; 45:263–269.
Article16. Rothwell PM, Giles MF, Flossmann E, Lovelock CE, Redgrave JN, Warlow CP, et al. A simple score (ABCD) to identify individuals at high early risk of stroke after transient ischaemic attack. Lancet. 2005; 366:29–36.
Article17. Sullivan LM, Massaro JM, D’Agostino RB Sr. Presentation of multivariate data for clinical use: the Framingham Study risk score functions. Stat Med. 2004; 23:1631–1660.
Article18. Johnston SC, Rothwell PM, Nguyen-Huynh MN, Giles MF, Elkins JS, Bernstein AL, et al. Validation and refinement of scores to predict very early stroke risk after transient ischaemic attack. Lancet. 2007; 369:283–292.
Article19. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845.
Article20. Makin SD, Doubal FN, Dennis MS, Wardlaw JM. Clinically confirmed stroke with negative diffusion-weighted imaging magnetic resonance imaging: longitudinal study of clinical outcomes, stroke recurrence, and systematic review. Stroke. 2015; 46:3142–3148.21. Brunser AM, Hoppe A, Illanes S, Díaz V, Muñoz P, Cárcamo D, et al. Accuracy of diffusion-weighted imaging in the diagnosis of stroke in patients with suspected cerebral infarct. Stroke. 2013; 44:1169–1171.
Article22. Doubal FN, Dennis MS, Wardlaw JM. Characteristics of patients with minor ischaemic strokes and negative MRI: a cross-sectional study. J Neurol Neurosurg Psychiatry. 2011; 82:540–542.
Article23. Watts J, Wood B, Kelly A, Alvaro A. Stroke syndromes associated with DWI-negative MRI include ataxic hemiparesis and isolated internuclear ophthalmoplegia. Neurol Clin Pract. 2013; 3:186–191.
Article24. Stadnik TW, Demaerel P, Luypaert RR, Chaskis C, Van Rompaey KL, Michotte A, et al. Imaging tutorial: differential diagnosis of bright lesions on diffusion-weighted MR images. Radiographics. 2003; 23:e7.
Article25. Yamaguchi NH. Smoking, immunity, and DNA damage. Transl Lung Cancer Res. 2019; 8(Suppl 1):S3–S6.
Article26. Linton MRF, Yancey PG, Davies SS, Jerome WG, Linton EF, Song WL, et al. The role of lipids and lipoproteins in atherosclerosis. In : Feingold KR, Anawalt B, Boyce A, Chrousos G, Dungan K, Grossman A, editors. Endotext. South Dartmouth, MA: MDText.com;2000.27. Tabas I. Consequences of cellular cholesterol accumulation: basic concepts and physiological implications. J Clin Invest. 2002; 110:905–911.
Article28. Marsh EB, Lawrence E, Hillis AE, Chen K, Gottesman RF, Llinas RH. Pre-stroke employment results in better patient-reported outcomes after minor stroke: short title. Functional outcomes after minor stroke. Clin Neurol Neurosurg. 2018; 165:38–42.29. Marsh EB, Llinas RH. Stroke recovery: does one size fit all? Neurology. 2018; 91:1038–1039.30. Lamassa M, Di Carlo A, Pracucci G, Basile AM, Trefoloni G, Vanni P, et al. Characteristics, outcome, and care of stroke associated with atrial fibrillation in Europe: data from a multicenter multinational hospital-based registry (The European Community Stroke Project). Stroke. 2001; 32:392–398.31. Coutts SB, Simon JE, Eliasziw M, Sohn CH, Hill MD, Barber PA, et al. Triaging transient ischemic attack and minor stroke patients using acute magnetic resonance imaging. Ann Neurol. 2005; 57:848–854.
Article32. Coutts SB, Moreau F, Asdaghi N, Boulanger JM, Camden MC, Campbell BCV, et al. Rate and prognosis of brain ischemia in patients with lower-risk transient or persistent minor neurologic events. JAMA Neurol. 2019; 76:1439–1445.
Article33. Ortiz de Mendivil A, Alcalá-Galiano A, Ochoa M, Salvador E, Millán JM. Brainstem stroke: anatomy, clinical and radiological findings. Semin Ultrasound CT MR. 2013; 34:131–141.34. Currier RD, Giles CL, Westerberg MR. The prognosis of some brain stem vascular syndromes. Neurology. 1958; 8:664–668.
Article35. Suzuki K, Kutsuzawa T, Takita K, Ito M, Sakamoto T, Hirayama A, et al. Clinico-epidemiologic study of stroke in Akita, Japan. Stroke. 1987; 18:402–406.
Article36. Kim CH, Kim JS. Development of cerebral infarction shortly after intracerebral hemorrhage. Eur Neurol. 2007; 57:145–149.
Article37. St Louis EK, Wijdicks EF, Li H. Predicting neurologic deterioration in patients with cerebellar hematomas. Neurology. 1998; 51:1364–1369.
Article38. Arboix A, Alió J. Cardioembolic stroke: clinical features, specific cardiac disorders and prognosis. Curr Cardiol Rev. 2010; 6:150–161.
Article39. Reeves M, Khoury J, Alwell K, Moomaw C, Flaherty M, Woo D, et al. Distribution of National Institutes of Health stroke scale in the Cincinnati/Northern Kentucky Stroke Study. Stroke. 2013; 44:3211–3213.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reversal of a Large Ischemic Lesion with Low Apparent Diffusion Coefficient Value by Rapid Spontaneous Recanalization
- Transient global amnesia associated with multiple lesions in the corpus callosum and hippocampus
- A Comparison of Lesion Detection and Conspicuity on T2-weighted Images (T2 FFE), FLAIR and Diffusion-weighted Images in Patients with Traumatic Brain Injury
- MR Imaging of Skeletal Muscle Injury in Rabbit: Comparison bet ween Diffusion and T2-weighted MR Images
- Global Aphasia without Hemiparesis: Lesion Analysis and its Mechanism in 12 Patients