J Stroke.
2021 Jan;23(1):51-60. 10.5853/jos.2020.03391.
Residual Risk and Its Risk Factors for Ischemic Stroke with Adherence to Guideline-Based Secondary Stroke Prevention
- Affiliations
-
- 1Department of Neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing, China
- 2China National Clinical Research Center for Neurological Diseases, Beijing, China
- KMID: 2512354
- DOI: http://doi.org/10.5853/jos.2020.03391
Abstract
- Background and Purpose
Despite administration of evidence-based therapies, residual risk of stroke recurrence persists. This study aimed to evaluate the residual risk of recurrent stroke in acute ischemic stroke or transient ischemic attack (TIA) with adherence to guideline-based secondary stroke prevention and identify the risk factors of the residual risk.
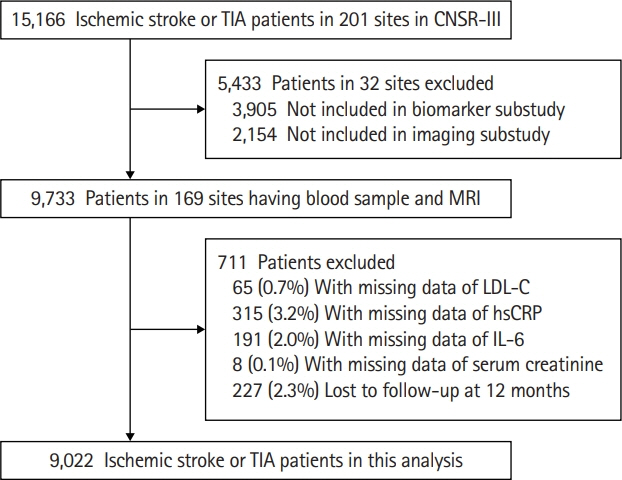
Methods
Patients with acute ischemic stroke or TIA within 7 hours were enrolled from 169 hospitals in Third China National Stroke Registry (CNSR-III) in China. Adherence to guideline-based secondary stroke prevention was defined as persistently receiving all of the five secondary prevention medications (antithrombotic, antidiabetic and antihypertensive agents, statin and anticoagulants) during hospitalization, at discharge, at 3, 6, and 12 months if eligible. The primary outcome was a new stroke at 12 months.
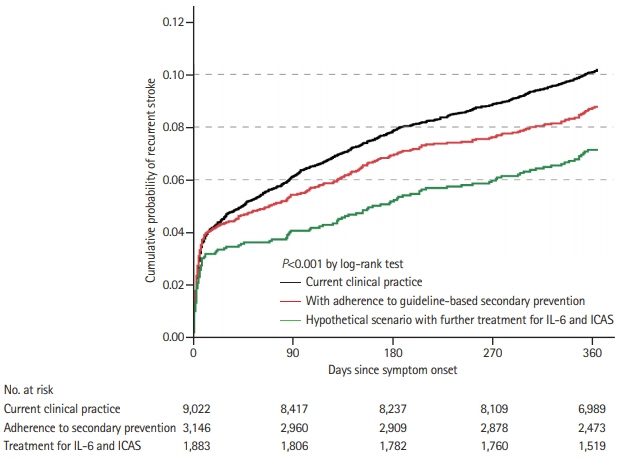
Results
Among 9,022 included patients (median age 63.0 years and 31.7% female), 3,146 (34.9%) were identified as adherence to guideline-based secondary prevention. Of all, 864 (9.6%) patients had recurrent stroke at 12 months, and the residual risk in patients with adherence to guidelinebased secondary prevention was 8.3%. Compared with those without adherence, patients with adherence to guideline-based secondary prevention had lower rate of recurrent stroke (hazard ratio, 0.85; 95% confidence interval, 0.74 to 0.99; P=0.04) at 12 months. Female, history of stroke, interleukin-6 ≥5.63 ng/L, and relevant intracranial artery stenosis were independent risk factors of the residual risk.
Conclusions
There was still a substantial residual risk of 12-month recurrent stroke even in patients with persistent adherence to guideline-based secondary stroke prevention. Future research should focus on efforts to reduce the residual risk.
Keyword
Figure
Reference
-
References
1. Chen Y, Wright N, Guo Y, Turnbull I, Kartsonaki C, Yang L, et al. Mortality and recurrent vascular events after first incident stroke: a 9-year community-based study of 0.5 million Chinese adults. Lancet Glob Health. 2020; 8:e580–e590.2. Lin B, Zhang Z, Mei Y, Wang C, Xu H, Liu L, et al. Cumulative risk of stroke recurrence over the last 10 years: a systematic review and meta-analysis. Neurol Sci. 2020; Oct. 10. [Epub]. https://doi.org/10.1007/s10072-020-04797-5.
Article3. Wang Y, Li Z, Zhao X, Wang C, Wang X, Wang D, et al. Effect of a multifaceted quality improvement intervention on hospital personnel adherence to performance measures in patients with acute ischemic stroke in China: a randomized clinical trial. JAMA. 2018; 320:245–254.4. Amarenco P, Lavallée PC, Labreuche J, Albers GW, Bornstein NM, Canhão P, et al. One-year risk of stroke after transient ischemic attack or minor stroke. N Engl J Med. 2016; 374:1533–1542.
Article5. Xie X, Wang X, Li Z, Zhao X, Miao Z, Liu L, et al. Prognostic value of international normalized ratio in ischemic stroke patients without atrial fibrillation or anticoagulation therapy. J Atheroscler Thromb. 2019; 26:378–387.
Article6. Li Z, Wang C, Zhao X, Liu L, Wang C, Li H, et al. Substantial progress yet significant opportunity for improvement in stroke care in China. Stroke. 2016; 47:2843–2849.
Article7. Ji R, Liu G, Shen H, Wang Y, Li H, Peterson E, et al. Persistence of secondary prevention medications after acute ischemic stroke or transient ischemic attack in Chinese population: data from China National Stroke Registry. Neurol Res. 2013; 35:29–36.
Article8. Patel KV, Pandey A, de Lemos JA. Conceptual framework for addressing residual atherosclerotic cardiovascular disease risk in the era of precision medicine. Circulation. 2018; 137:2551–2553.
Article9. Ridker PM. Residual inflammatory risk: addressing the obverse side of the atherosclerosis prevention coin. Eur Heart J. 2016; 37:1720–1722.
Article10. Wang Y, Jing J, Meng X, Pan Y, Wang Y, Zhao X, et al. The Third China National Stroke Registry (CNSR-III) for patients with acute ischaemic stroke or transient ischaemic attack: design, rationale and baseline patient characteristics. Stroke Vasc Neurol. 2019; 4:158–164.
Article11. Stroke: 1989. Recommendations on stroke prevention, diagnosis, and therapy. Report of the WHO Task Force on Stroke and other Cerebrovascular Disorders. Stroke. 1989; 20:1407–1431.12. Nordestgaard BG, Langlois MR, Langsted A, Chapman MJ, Aakre KM, Baum H, et al. Quantifying atherogenic lipoproteins for lipid-lowering strategies: consensus-based recommendations from EAS and EFLM. Atherosclerosis. 2020; 294:46–61.
Article13. Ma YC, Zuo L, Chen JH, Luo Q, Yu XQ, Li Y, et al. Modified glomerular filtration rate estimating equation for Chinese patients with chronic kidney disease. J Am Soc Nephrol. 2006; 17:2937–2944.
Article14. Levey AS, Coresh J, Greene T, Stevens LA, Zhang YL, Hendriksen S, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006; 145:247–254.
Article15. Samuels OB, Joseph GJ, Lynn MJ, Smith HA, Chimowitz MI. A standardized method for measuring intracranial arterial stenosis. AJNR Am J Neuroradiol. 2000; 21:643–646.16. Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993; 24:35–41.
Article17. Pan Y, Chen R, Li Z, Li H, Zhao X, Liu L, et al. Socioeconomic status and the quality of acute stroke care: The China National Stroke Registry. Stroke. 2016; 47:2836–2842.18. Xian Y, Holloway RG, Chan PS, Noyes K, Shah MN, Ting HH, et al. Association between stroke center hospitalization for acute ischemic stroke and mortality. JAMA. 2011; 305:373–380.
Article19. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999; 94:496–509.
Article20. Brookhart MA, Wyss R, Layton JB, Stürmer T. Propensity score methods for confounding control in nonexperimental research. Circ Cardiovasc Qual Outcomes. 2013; 6:604–611.
Article21. Jiang J, Cai X, Pan Y, Du X, Zhu H, Yang X, et al. Relationship of obesity to adipose tissue insulin resistance. BMJ Open Diabetes Res Care. 2020; 8:e000741.
Article22. Bushnell CD, Olson DM, Zhao X, Pan W, Zimmer LO, Goldstein LB, et al. Secondary preventive medication persistence and adherence 1 year after stroke. Neurology. 2011; 77:1182–1190.
Article23. Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011; 365:993–1003.24. Cainzos-Achirica M, Enjuanes C, Greenland P, McEvoy JW, Cushman M, Dardari Z, et al. The prognostic value of interleukin 6 in multiple chronic diseases and all-cause death: the Multi-Ethnic Study of Atherosclerosis (MESA). Atherosclerosis. 2018; 278:217–225.
Article25. Jenny NS, Callas PW, Judd SE, McClure LA, Kissela B, Zakai NA, et al. Inflammatory cytokines and ischemic stroke risk: the REGARDS cohort. Neurology. 2019; 92:e2375–e2384.26. Elkind MS, Luna JM, McClure LA, Zhang Y, Coffey CS, Roldan A, et al. C-reactive protein as a prognostic marker after lacunar stroke: levels of inflammatory markers in the treatment of stroke study. Stroke. 2014; 45:707–716.27. Li J, Zhao X, Meng X, Lin J, Liu L, Wang C, et al. High-sensitive c-reactive protein predicts recurrent stroke and poor functional outcome: subanalysis of the clopidogrel in high-risk patients with acute nondisabling cerebrovascular events trial. Stroke. 2016; 47:2025–2030.28. Ridker PM, Everett BM, Thuren T, MacFadyen JG, Chang WH, Ballantyne C, et al. Antiinflammatory therapy with canakinumab for atherosclerotic disease. N Engl J Med. 2017; 377:1119–1131.
Article29. Wang Y, Zhao X, Liu L, Soo YO, Pu Y, Pan Y, et al. Prevalence and outcomes of symptomatic intracranial large artery stenoses and occlusions in China: the Chinese Intracranial Atherosclerosis (CICAS) Study. Stroke. 2014; 45:663–669.30. Derdeyn CP, Chimowitz MI, Lynn MJ, Fiorella D, Turan TN, Janis LS, et al. Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): the final results of a randomised trial. Lancet. 2014; 383:333–341.31. Yang XM, Rao ZZ, Gu HQ, Zhao XQ, Wang CJ, Liu LP, et al. Atrial fibrillation known before or detected after stroke share similar risk of ischemic stroke recurrence and death. Stroke. 2019; 50:1124–1129.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antiplatelet Therapy for Secondary Stroke Prevention in Patients with Ischemic Stroke or Transient Ischemic Attack
- Pharmacological Secondary Prevention of Ischemic Stroke
- Blood Pressure Management for Stroke Prevention and in Acute Stroke
- The connection between diabetes mellitus and stroke: a brief review
- Risk Factors and Biomarkers of Ischemic Stroke in Cancer Patients