Anesth Pain Med.
2021 Jan;16(1):1-7. 10.17085/apm.20090.
Who are at high risk of mortality and morbidity among children with congenital heart disease undergoing noncardiac surgery?
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Laboratory for Cardiovascular Dynamics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2512277
- DOI: http://doi.org/10.17085/apm.20090
Abstract
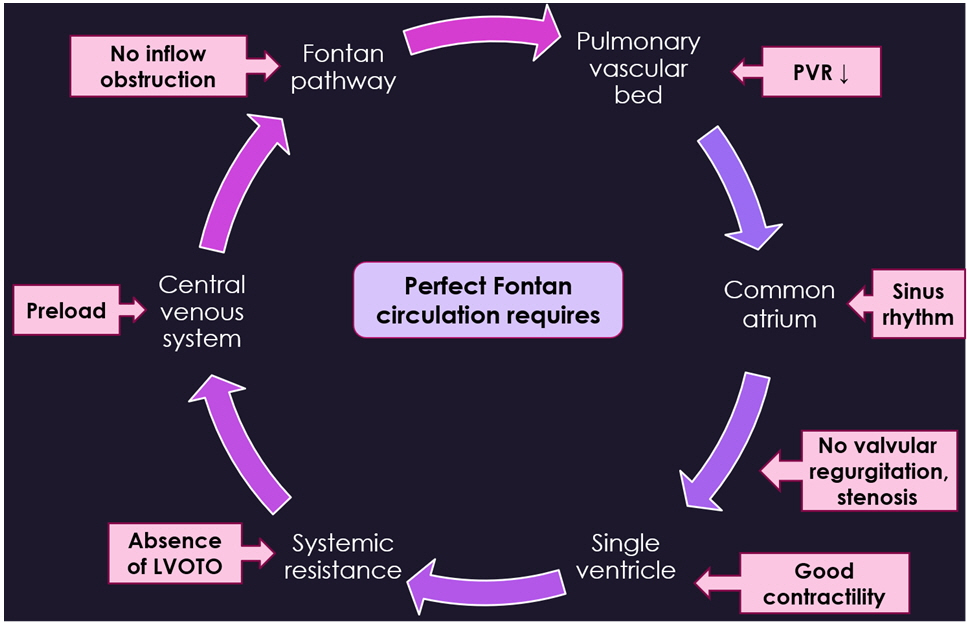
- With advances in the development of surgical and medical treatments for congenital heart disease (CHD), the population of children and adults with CHD is growing. This population requires multiple surgical and diagnostic imaging procedures. Therefore, general anesthesia is inevitable. In many studies, it has been reported that children with CHD have increased anesthesia risks when undergoing noncardiac surgeries compared to children without CHD. The highest risk group included patients with functional single ventricle, suprasystemic pulmonary hypertension, left ventricular outflow obstruction, and cardiomyopathy. In this review, we provide an overview of perioperative risks in children with CHD undergoing noncardiac surgeries and anesthetic considerations in patients classified as having the highest risk.
Keyword
Figure
Reference
-
1. Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am Coll Cardiol. 2002; 39:1890–900.2. Marelli AJ, Ionescu-Ittu R, Mackie AS, Guo L, Dendukuri N, Kaouache M. Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation. 2014; 130:749–56.3. Sulkowski JP, Cooper JN, McConnell PI, Pasquali SK, Shah SS, Minneci PC, et al. Variability in noncardiac surgical procedures in children with congenital heart disease. J Pediatr Surg. 2014; 49:1564–9.4. Baum VC, Barton DM, Gutgesell HP. Influence of congenital heart disease on mortality after noncardiac surgery in hospitalized children. Pediatrics. 2000; 105:332–5.5. Ramamoorthy C, Haberkern CM, Bhananker SM, Domino KB, Posner KL, Campos JS, et al. Anesthesia-related cardiac arrest in children with heart disease: data from the Pediatric Perioperative Cardiac Arrest (POCA) registry. Anesth Analg. 2010; 110:1376–82.6. Flick RP, Sprung J, Harrison TE, Gleich SJ, Schroeder DR, Hanson AC, et al. Perioperative cardiac arrests in children between 1988 and 2005 at a tertiary referral center: a study of 92,881 patients. Anesthesiology. 2007; 106:226–37.7. van der Griend BF, Lister NA, McKenzie IM, Martin N, Ragg PG, Sheppard SJ, et al. Postoperative mortality in children after 101,885 anesthetics at a tertiary pediatric hospital. Anesth Analg. 2011; 112:1440–7.8. Faraoni D, Zurakowski D, Vo D, Goobie SM, Yuki K, Brown ML, et al. Post-operative outcomes in children with and without congenital heart disease undergoing noncardiac surgery. J Am Coll Cardiol. 2016; 67:793–801.9. Miller R, Tumin D, Tobias JD, McKee C. Estimating surgical risk in younger and older children with congenital heart disease. J Surg Res. 2018; 232:298–307.10. Lee S, Reddington E, Koutsogiannaki S, Hernandez MR, Odegard KC, DiNardo JA, et al. Incidence and risk factors for perioperative cardiovascular and respiratory adverse events in pediatric patients with congenital heart disease undergoing noncardiac procedures. Anesth Analg. 2018; 127:724–9.11. Saettele AK, Christensen JL, Chilson KL, Murray DJ. Children with heart disease: risk stratification for non-cardiac surgery. J Clin Anesth. 2016; 35:479–84.12. Ng SM, Jin X, Yates R, Kelsall AW. Outcome of noncardiac surgery in children with congenital heart disease performed outside a cardiac center. J Pediatr Surg. 2016; 51:252–6.13. White MC, Peyton JM. Anaesthetic management of children with congenital heart disease for non-cardiac surgery. Contin Educ Anaesth Crit Care Pain. 2012; 12:17–22.14. Faraoni D, Vo D, Nasr VG, DiNardo JA. Development and validation of a risk stratification score for children with congenital heart disease undergoing noncardiac surgery. Anesth Analg. 2016; 123:824–30.15. Torres A Jr, DiLiberti J, Pearl RH, Wohrley J, Raff GW, Bysani GK, et al. Noncardiac surgery in children with hypoplastic left heart syndrome. J Pediatr Surg. 2002; 37:1399–403.16. Gottlieb EA, Andropoulos DB. Anesthesia for the patient with congenital heart disease presenting for noncardiac surgery. Curr Opin Anaesthesiol. 2013; 26:318–26.17. Mott AR, Alomrani A, Tortoriello TA, Perles Z, East DL, Stayer SA. Changes in cerebral saturation profile in response to mechanical ventilation alterations in infants with bidirectional superior cavopulmonary connection. Pediatr Crit Care Med. 2006; 7:346–50.18. Penny DJ, Hayek Z, Redington AN. The effects of positive and negative extrathoracic pressure ventilation on pulmonary blood flow after the total cavopulmonary shunt procedure. Int J Cardiol. 1991; 30:128–30.19. Redington AN, Penny D, Shinebourne EA. Pulmonary blood flow after total cavopulmonary shunt. Br Heart J. 1991; 65:213–7.20. Yuki K, Casta A, Uezono S. Anesthetic management of noncardiac surgery for patients with single ventricle physiology. J Anesth. 2011; 25:247–56.21. Odegard KC, McGowan FX Jr, Zurakowski D, Dinardo JA, Castro RA, del Nido PJ, et al. Procoagulant and anticoagulant factor abnormalities following the Fontan procedure: increased factor VIII may predispose to thrombosis. J Thorac Cardiovasc Surg. 2003; 125:1260–7.22. Windsor J, Townsley MM, Briston D, Villablanca PA, Alegria JR, Ramakrishna H. Fontan palliation for single-ventricle physiology: perioperative management for noncardiac surgery and analysis of outcomes. J Cardiothorac Vasc Anesth. 2017; 31:2296–303.23. Chau DF, Gangadharan M, Hartke LP, Twite MD. The post-anesthetic care of pediatric patients with pulmonary hypertension. Semin Cardiothorac Vasc Anesth. 2016; 20:63–73.24. Abman SH, Hansmann G, Archer SL, Ivy DD, Adatia I, Chung WK, et al. American Heart Association Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Clinical Cardiology; Council on Cardiovascular Disease in the Young; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Surgery and Anesthesia; and the American Thoracic Society. Pediatric pulmonary hypertension: guidelines from the American Heart Association and American Thoracic Society. Circulation. 2015; 132:2037–99.25. Latham GJ, Yung D. Current understanding and perioperative management of pediatric pulmonary hypertension. Paediatr Anaesth. 2019; 29:441–56.26. Brown ML, DiNardo JA, Nasr VG. Anesthesia in pediatric patients with congenital heart disease undergoing noncardiac surgery: defining the risk. J Cardiothorac Vasc Anesth. 2020; 34:470–8.27. Matisoff AJ, Olivieri L, Schwartz JM, Deutsch N. Risk assessment and anesthetic management of patients with Williams syndrome: a comprehensive review. Paediatr Anaesth. 2015; 25:1207–15.28. Kipps AK, Ramamoorthy C, Rosenthal DN, Williams GD. Children with cardiomyopathy: complications after noncardiac procedures with general anesthesia. Paediatr Anaesth. 2007; 17:775–81.29. Murphy TW, Smith JH, Ranger MR, Haynes SR. General anesthesia for children with severe heart failure. Pediatr Cardiol. 2011; 32:139–44.30. Ing RJ, Ames WA, Chambers NA. Paediatric cardiomyopathy and anaesthesia. Br J Anaesth. 2012; 108:4–12.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Morbidity and Mortality Analysis after Noncardiac Surgery in Patients with Prior Myocardial Infarction
- Genetic Syndromes associated with Congenital Heart Disease
- Pulmonary Arterial Hypertension with Congenital Heart Diseases
- Pediatric Heart Failure: Current State and Future Possibilities
- Noncardiac Chest Pain: Epidemiology, Natural Course and Pathogenesis