Intest Res.
2021 Jan;19(1):106-114. 10.5217/ir.2019.00136.
Patients with celiac disease are at high risk of developing metabolic syndrome and fatty liver
- Affiliations
-
- 1Department of Gastroenterology and Human Nutrition, All India Institute of Medical Sciences, New Delhi, India
- KMID: 2512106
- DOI: http://doi.org/10.5217/ir.2019.00136
Abstract
- Background/Aims
Gluten-free diet has an excess of fats and simple sugars and puts patients with celiac disease at risk of metabolic complications including metabolic syndrome and fatty liver. We assessed prevalence of metabolic syndrome and fatty liver in two cohorts of celiac disease.
Methods
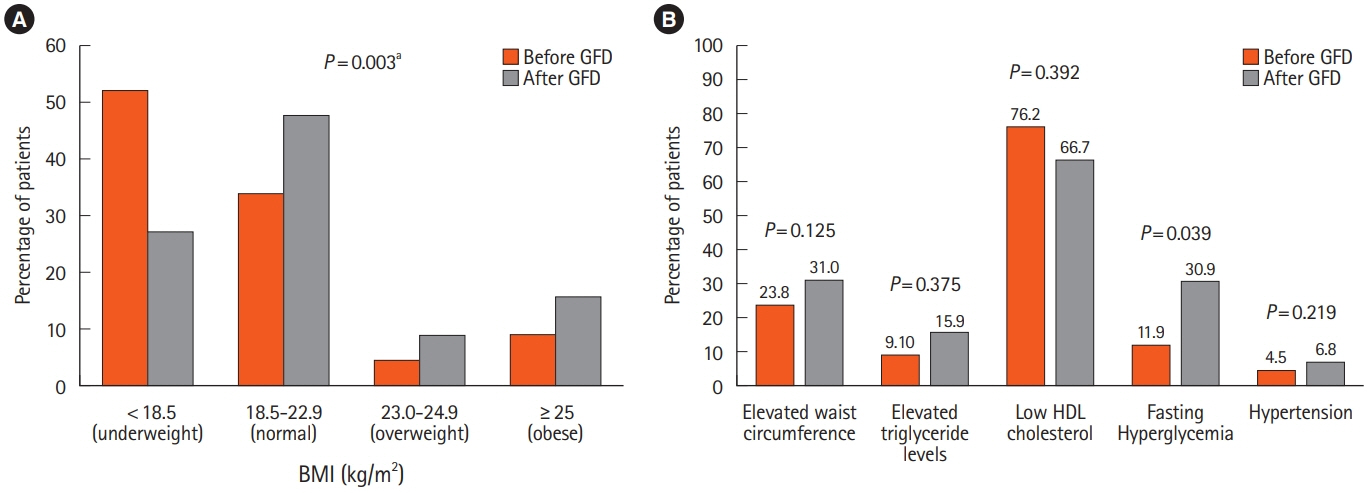
Study was done in 2 groups. In group 1, 54 treatment naïve patients with celiac disease were recruited. Of them, 44 returned after 1-year of gluten-free diet and were reassessed. In group 2, 130 celiac disease patients on gluten-free diet for ≥1 year were recruited. All patients were assessed for anthropometric and metabolic parameters and fatty liver. Metabolic syndrome was defined as per consensus definition for Asian Indians. Fatty liver was defined as controlled attenuation parameter value >263 decibels by FibroScan.
Results
In group 1, of 44 treatment naïve patients with celiac disease, metabolic syndrome was present in 5 patients (11.4%) at baseline and 9 (18.2%) after 1 year of gluten-free diet. Patients having fatty liver increased from 6 patients (14.3%) at baseline to 13 (29.5%) after 1year of gluten-free diet (P=0.002). In group 2, of 130 patients with celiac disease on gluten-free diet for a median duration of 4 years, 30 out of 114 (26.3%) and 30 out of 130 patients (23%) had metabolic syndrome and fatty liver, respectively.
Conclusions
Patients with celiac disease are at high risk of developing metabolic syndrome and fatty liver, which increases further with gluten-free diet. These patients should be assessed for nutritional and metabolic features and counseled about balanced diet and physical activity regularly.
Keyword
Figure
Cited by 1 articles
-
Obesity and Colorectal Cancer
Jundeok Lee, Su Young Kim
Korean J Gastroenterol. 2023;82(2):63-72. doi: 10.4166/kjg.2023.083.
Reference
-
1. Singh I, Agnihotri A, Sharma A, et al. Patients with celiac disease may have normal weight or may even be overweight. Indian J Gastroenterol. 2016; 35:20–24.
Article2. Tucker E, Rostami K, Prabhakaran S, Al Dulaimi D. Patients with coeliac disease are increasingly overweight or obese on presentation. J Gastrointestin Liver Dis. 2012; 21:11–15.3. Stein AC, Liao C, Paski S, Polonsky T, Semrad CE, Kupfer SS. Obesity and cardiovascular risk in adults with celiac disease. J Clin Gastroenterol. 2016; 50:545–550.
Article4. Kabbani TA, Goldberg A, Kelly CP, et al. Body mass index and the risk of obesity in coeliac disease treated with the glutenfree diet. Aliment Pharmacol Ther. 2012; 35:723–729.
Article5. Ukkola A, Mäki M, Kurppa K, et al. Changes in body mass index on a gluten-free diet in coeliac disease: a nationwide study. Eur J Intern Med. 2012; 23:384–388.
Article6. Cheng J, Brar PS, Lee AR, Green PH. Body mass index in celiac disease: beneficial effect of a gluten-free diet. J Clin Gastroenterol. 2010; 44:267–271.7. Dickey W, Kearney N. Overweight in celiac disease: prevalence, clinical characteristics, and effect of a gluten-free diet. Am J Gastroenterol. 2006; 101:2356–2359.
Article8. Reilly NR, Aguilar K, Hassid BG, et al. Celiac disease in normal-weight and overweight children: clinical features and growth outcomes following a gluten-free diet. J Pediatr Gastroenterol Nutr. 2011; 53:528–531.9. Tortora R, Capone P, De Stefano G, et al. Metabolic syndrome in patients with coeliac disease on a gluten-free diet. Aliment Pharmacol Ther. 2015; 41:352–359.
Article10. Diamanti A, Capriati T, Basso MS, et al. Celiac disease and overweight in children: an update. Nutrients. 2014; 6:207–220.
Article11. Papastamataki M, Papassotiriou I, Bartzeliotou A, et al. Incretins, amylin and other gut-brain axis hormones in children with coeliac disease. Eur J Clin Invest. 2014; 44:74–82.
Article12. Dam-Larsen S, Becker U, Franzmann MB, Larsen K, Christoffersen P, Bendtsen F. Final results of a long-term, clinical follow-up in fatty liver patients. Scand J Gastroenterol. 2009; 44:1236–1243.
Article13. Naschitz JE, Yeshurun D, Zuckerman E, Arad E, Boss JH. Massive hepatic steatosis complicating adult celiac disease: report of a case and review of the literature. Am J Gastroenterol. 1987; 82:1186–1189.14. Bardella MT, Valenti L, Pagliari C, et al. Searching for coeliac disease in patients with non-alcoholic fatty liver disease. Dig Liver Dis. 2004; 36:333–336.
Article15. Lo Iacono O, Petta S, Venezia G, et al. Anti-tissue transglutaminase antibodies in patients with abnormal liver tests: is it always coeliac disease? Am J Gastroenterol. 2005; 100:2472–2477.
Article16. Rahimi AR, Daryani NE, Ghofrani H, et al. The prevalence of celiac disease among patients with non-alcoholic fatty liver disease in Iran. Turk J Gastroenterol. 2011; 22:300–304.
Article17. Reilly NR, Lebwohl B, Hultcrantz R, Green PH, Ludvigsson JF. Increased risk of non-alcoholic fatty liver disease after diagnosis of celiac disease. J Hepatol. 2015; 62:1405–1411.
Article18. Tovoli F, Negrini G, Farì R, et al. Increased risk of nonalcoholic fatty liver disease in patients with coeliac disease on a glutenfree diet: beyond traditional metabolic factors. Aliment Pharmacol Ther. 2018; 48:538–546.
Article19. Emilsson L, Lebwohl B, Sundström J, Ludvigsson JF. Cardiovascular disease in patients with coeliac disease: a systematic review and meta-analysis. Dig Liver Dis. 2015; 47:847–852.
Article20. Husby S, Koletzko S, Korponay-Szabó IR, et al. European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. J Pediatr Gastroenterol Nutr. 2012; 54:136–160.
Article21. World Health Organization. STEPwise approach to surveillance (STEPS) [Internet]. c2018 [cited 2018 Jul 10]. http://www.who.int/ncds/surveillance/steps/en/.22. Misra A, Chowbey P, Makkar BM, et al. Consensus statement for diagnosis of obesity, abdominal obesity and the metabolic syndrome for Asian Indians and recommendations for physical activity, medical and surgical management. J Assoc Physicians India. 2009; 57:163–170.23. Rout G, Kedia S, Nayak B, et al. Controlled attenuation parameter for assessment of hepatic steatosis in Indian patients. J Clin Exp Hepatol. 2019; 9:13–21.
Article24. Sawant A, Mankeshwar R, Shah S, et al. Prevalence of metabolic syndrome in urban India. Cholesterol. 2011; 2011:920983.
Article25. Gupta R, Deedwania PC, Gupta A, Rastogi S, Panwar RB, Kothari K. Prevalence of metabolic syndrome in an Indian urban population. Int J Cardiol. 2004; 97:257–261.
Article26. Singh SP, Nayak S, Swain M, et al. Prevalence of nonalcoholic fatty liver disease in coastal eastern India: a preliminary ultrasonographic survey. Trop Gastroenterol. 2004; 25:76–79.27. Amarapurkar D, Kamani P, Patel N, et al. Prevalence of non-alcoholic fatty liver disease: population based study. Ann Hepatol. 2007; 6:161–163.
Article28. Mohan V, Farooq S, Deepa M, Ravikumar R, Pitchumoni CS. Prevalence of non-alcoholic fatty liver disease in urban south Indians in relation to different grades of glucose intolerance and metabolic syndrome. Diabetes Res Clin Pract. 2009; 84:84–91.
Article29. Macabuag-Oliva AM, Capellan ML, Benitez B. A comparison of the sensitivity and specificity of ultrasound elastography compared to liver ultrasound, ALT, and AST in the detection of fatty liver and fibrosis in patients with metabolic syndrome and type 2 diabetes mellitus. J ASEAN Fed Endocr Soc. 2014; 29:59–64.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical impact of nonalcoholic fatty liver disease on other medical diseases
- Non-Alcoholic Fatty Liver Disease and Metabolic Syndrome
- The crosstalk between insulin resistance and nonalcoholic fatty liver disease/metabolic dysfunction-associated fatty liver disease: a culprit or a consequence?
- Nonalcoholic fatty liver disease as a risk factor of cardiovascular disease
- As sociation of Non-alcoholic Fatty Liver Disease with Metabolic Syndrome over 65 Years Elderly