Restor Dent Endod.
2020 Nov;45(4):e50. 10.5395/rde.2020.45.e50.
Incorporation of amoxicillin-loaded microspheres in mineral trioxide aggregate cement: an in vitro study
- Affiliations
-
- 1Department of Dental Materials, School of Dentistry, Federal University of Rio Grande do Sul, Porto Alegre, RS, Brazil
- 2Department of Orthodontics and Biomaterials, Centro Universitário UDF, Brasília, DF, Brazil
- 3Cosmetology Laboratory, School of Pharmaceutical Sciences, Federal University of Rio Grande do Sul, Porto Alegre, RS, Brazil
- 4Yller Biomaterials, Pelotas, RS, Brazil
- 5Program in Biomedical Sciences, University of Maryland School of Dentistry, Baltimore, MD, USA
- 6Division of Operative Dentistry, Department of General Dentistry, University of Maryland School of Dentistry, Baltimore, MD, USA
- KMID: 2512041
- DOI: http://doi.org/10.5395/rde.2020.45.e50
Abstract
Objectives
In this study, we investigated the potential of amoxicillin-loaded polymeric microspheres to be delivered to tooth root infection sites via a bioactive reparative cement.
Materials and Methods
Amoxicillin-loaded microspheres were synthesized by a spray-dray method and incorporated at 2.5% and 5% into a mineral trioxide aggregate cement clinically used to induce a mineralized barrier at the root tip of young permanent teeth with incomplete root development and necrotic pulp. The formulations were modified in liquid:powder ratios and in composition by the microspheres. The optimized formulations were evaluated in vitro for physical and mechanical eligibility. The morphology of microspheres was observed under scanning electron microscopy.
Results
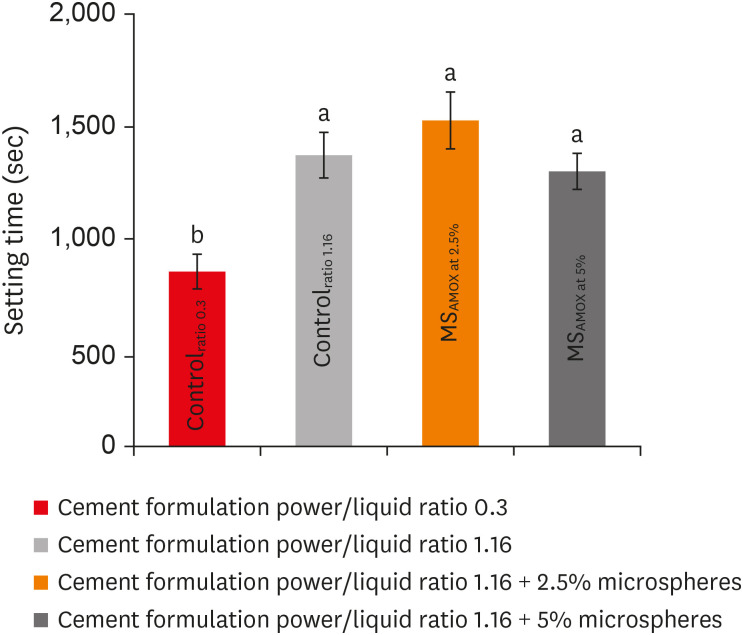
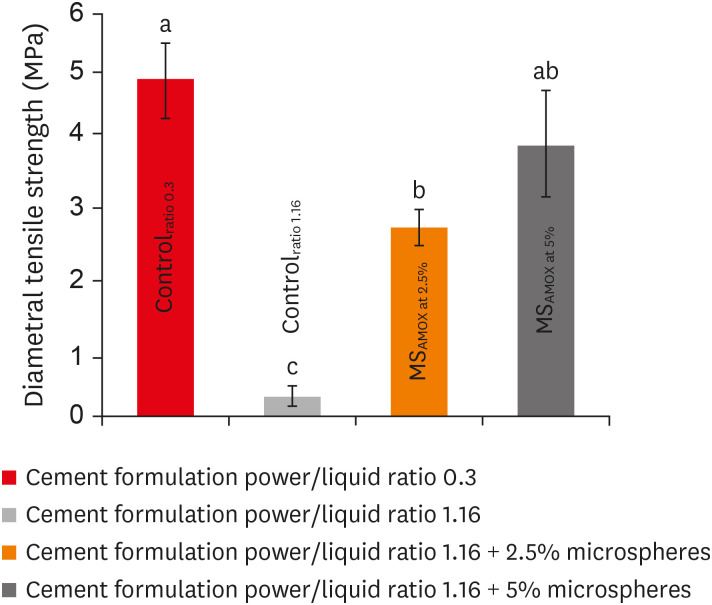
The optimized cement formulation containing microspheres at 5% exhibited a delayed-release response and maintained its fundamental functional properties. When mixed with amoxicillin-loaded microspheres, the setting times of both test materials significantly increased. The diametral tensile strength of cement containing microspheres at 5% was similar to control. However, phytic acid had no effect on this outcome (p > 0.05). When mixed with modified liquid:powder ratio, the setting time was significantly longer than that original liquid:powder ratio (p < 0.05).
Conclusions
Lack of optimal concentrations of antibiotics at anatomical sites of the dental tissues is a hallmark of recurrent endodontic infections. Therefore, targeting the controlled release of broad-spectrum antibiotics may improve the therapeutic outcomes of current treatments. Overall, these results indicate that the carry of amoxicillin by microspheres could provide an alternative strategy for the local delivery of antibiotics for the management of tooth infections.
Figure
Reference
-
1. Ricucci D, Loghin S, Niu LN, Tay FR. Changes in the radicular pulp-dentine complex in healthy intact teeth and in response to deep caries or restorations: a histological and histobacteriological study. J Dent. 2018; 73:76–90. PMID: 29660488.
Article2. Ricucci D, Siqueira JF Jr, Loghin S, Lin LM. Pulp and apical tissue response to deep caries in immature teeth: a histologic and histobacteriologic study. J Dent. 2017; 56:19–32. PMID: 27744048.
Article3. Farges JC, Alliot-Licht B, Renard E, Ducret M, Gaudin A, Smith AJ, Cooper PR. Dental pulp defence and repair mechanisms in dental caries. Mediators Inflamm. 2015; 2015:230251. PMID: 26538821.
Article4. Martin FE. Carious pulpitis: microbiological and histopathological considerations. Aust Endod J. 2003; 29:134–137. PMID: 14700398.
Article5. Guerrero F, Mendoza A, Ribas D, Aspiazu K. Apexification: a systematic review. J Conserv Dent. 2018; 21:462–465. PMID: 30294103.
Article6. Flanagan TA. What can cause the pulps of immature, permanent teeth with open apices to become necrotic and what treatment options are available for these teeth. Aust Endod J. 2014; 40:95–100. PMID: 25470507.
Article7. Conde MCM, Chisini LA, Sarkis-Onofre R, Schuch HS, Nör JE, Demarco FF. A scoping review of root canal revascularization: relevant aspects for clinical success and tissue formation. Int Endod J. 2017; 50:860–874. PMID: 27770435.
Article8. Felippe WT, Felippe MCS, Rocha MJC. The effect of mineral trioxide aggregate on the apexification and periapical healing of teeth with incomplete root formation. Int Endod J. 2006; 39:2–9. PMID: 16409322.
Article9. Pace R, Giuliani V, Nieri M, Di Nasso L, Pagavino G. Mineral trioxide aggregate as apical plug in teeth with necrotic pulp and immature apices: a 10-year case series. J Endod. 2014; 40:1250–1254. PMID: 25069943.
Article10. Torabinejad M, Nosrat A, Verma P, Udochukwu O. Regenerative endodontic treatment or mineral trioxide aggregate apical plug in teeth with necrotic pulps and open apices: a systematic review and meta-analysis. J Endod. 2017; 43:1806–1820. PMID: 28822564.
Article11. Mohammadi Z, Shalavi S. Effect of hydroxyapatite and bovine serum albumin on the antibacterial activity of MTA. Iran Endod J. 2011; 6:136–139. PMID: 23130067.12. Kim RJY, Kim MO, Lee KS, Lee DY, Shin JH. An in vitro evaluation of the antibacterial properties of three mineral trioxide aggregate (MTA) against five oral bacteria. Arch Oral Biol. 2015; 60:1497–1502. PMID: 26263538.
Article13. Piluso S, Soultan AH, Patterson J. Molecularly engineered polymer-based systems in drug delivery and regenerative medicine. Curr Pharm Des. 2017; 23:281–294. PMID: 27774909.
Article14. Merkle HP. Drug delivery's quest for polymers: where are the frontiers? Eur J Pharm Biopharm. 2015; 97:293–303. PMID: 26614554.
Article15. Cuppini M, Zatta KC, Mestieri LB, Grecca FS, Leitune VCB, Guterres SS, Collares FM. Antimicrobial and anti-inflammatory drug-delivery systems at endodontic reparative material: synthesis and characterization. Dent Mater. 2019; 35:457–467. PMID: 30642636.
Article16. Ghosh Dastidar D, Saha S, Chowdhury M. Porous microspheres: synthesis, characterisation and applications in pharmaceutical & medical fields. Int J Pharm. 2018; 548:34–48. PMID: 29940297.
Article17. Gupta V, Khan Y, Berkland CJ, Laurencin CT, Detamore MS. Microsphere-based scaffolds in regenerative engineering. Annu Rev Biomed Eng. 2017; 19:135–161. PMID: 28633566.
Article18. Chawla A, Sharma P, Pawar P. Eudragit S-100 coated sodium alginate microspheres of naproxen sodium: formulation, optimization and in vitro evaluation. Acta Pharm. 2012; 62:529–545. PMID: 23333888.
Article19. Kaur G, Grewal J, Jyoti K, Jain UK, Chandra R, Madan J. Oral controlled and sustained drug delivery systems: concepts, advances, preclinical, and clinical status. In : Grumezescu AM, editor. Drug targeting and stimuli sensitive drug delivery systems. Norwich, NY: William Andrew Publishing;2018. p. 567–626.20. Bolfoni MR, Pappen FG, Pereira-Cenci T, Jacinto RC. Antibiotic prescription for endodontic infections: a survey of Brazilian endodontists. Int Endod J. 2018; 51:148–156. PMID: 28744872.
Article21. Segura-Egea JJ, Gould K, Şen BH, Jonasson P, Cotti E, Mazzoni A, Sunay H, Tjäderhane L, Dummer PM. Antibiotics in endodontics: a review. Int Endod J. 2017; 50:1169–1184. PMID: 28005295.
Article22. Dornelles NB, Collares FM, Genari B, de Souza Balbinot G, Samuel SMW, Arthur RA, Visioli F, Guterres SS, Leitune VCB. Influence of the addition of microsphere load amoxicillin in the physical, chemical and biological properties of an experimental endodontic sealer. J Dent. 2018; 68:28–33. PMID: 29107135.
Article23. Kokubo T, Takadama H. How useful is SBF in predicting in vivo bone bioactivity? Biomaterials. 2006; 27:2907–2915. PMID: 16448693.
Article24. Ha WN, Nicholson T, Kahler B, Walsh LJ. Methodologies for measuring the setting times of mineral trioxide aggregate and Portland cement products used in dentistry. Acta Biomater Odontol Scand. 2016; 2:25–30. PMID: 28642908.
Article25. Parhizkar A, Nojehdehian H, Asgary S. Triple antibiotic paste: momentous roles and applications in endodontics: a review. Restor Dent Endod. 2018; 43:e28. PMID: 30135847.
Article26. Lee G, Chung C, Kim S, Shin SJ. Observation of an extracted premolar 2.5 years after mineral trioxide aggregate apexification using micro-computed tomography. Restor Dent Endod. 2019; 45:e4. PMID: 32483529.
Article27. Cartagena AF, Esmerino LA, Polak-Junior R, Olivieri Parreiras S, Domingos Michél M, Farago PV, Campanha NH. New denture adhesive containing miconazole nitrate polymeric microparticles: antifungal, adhesive force and toxicity properties. Dent Mater. 2017; 33:e53–e61. PMID: 27745775.
Article28. Gavini E, Bonferoni MC, Rassu G, Obinu A, Ferrari F, Giunchedi P. Biodegradable microspheres as intravitreal delivery systems for prolonged drug release. what is their eminence in the nanoparticle era? Curr Drug Deliv. 2018; 15:930–940. PMID: 29484995.
Article29. Duarte MA, Demarchi AC, Yamashita JC, Kuga MC, Fraga SC. pH and calcium ion release of 2 root-end filling materials. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003; 95:345–347. PMID: 12627108.
Article30. Javid B, Panahandeh N, Torabzadeh H, Nazarian H, Parhizkar A, Asgary S. Bioactivity of endodontic biomaterials on dental pulp stem cells through dentin. Restor Dent Endod. 2019; 45:e3. PMID: 32110533.
Article31. Mestieri LB, Zaccara IM, Pinheiro LS, Barletta FB, Kopper PMP, Grecca FS. Cytocompatibility and cell proliferation evaluation of calcium phosphate-based root canal sealers. Restor Dent Endod. 2019; 45:e2. PMID: 32110532.
Article32. Fridland M, Rosado R. Mineral trioxide aggregate (MTA) solubility and porosity with different water-to-powder ratios. J Endod. 2003; 29:814–817. PMID: 14686812.
Article33. Basturk FB, Nekoofar MH, Günday M, Dummer PM. The effect of various mixing and placement techniques on the compressive strength of mineral trioxide aggregate. J Endod. 2013; 39:111–114. PMID: 23228268.
Article34. Bouyarmane H, El Hanbali I, El Karbane M, Rami A, Saoiabi A, Saoiabi S, Masse S, Coradin T, Laghzizil A. Parameters influencing ciprofloxacin, ofloxacin, amoxicillin and sulfamethoxazole retention by natural and converted calcium phosphates. J Hazard Mater. 2015; 291:38–44. PMID: 25749000.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mineral trioxied aggregate and its substitutes
- Evaluation of the rat tissue reaction to experimental new resin cement and mineral trioxide aggregate cement
- Use of mineral trioxide aggregate in the treatment of horizontal root fracture with a 4-year follow-up: case report
- Effect of Drug Carrier Melting Points on Drug Release of Dexamethasone-Loaded Microspheres
- Prolonged Regional Anesthesia with Lidocaine Microspheres by Using a Biodegradable Polymer