Restor Dent Endod.
2020 Nov;45(4):e45. 10.5395/rde.2020.45.e45.
A new phantom to evaluate the tissue dissolution ability of endodontic irrigants and activating devices
- Affiliations
-
- 1Marquette University School of Dentistry, Milwaukee, WI, USA
- 2Inter Med-Vista Dental, Racine, WI, USA
- 3Faculty of Dentistry, Mansoura University, Mansoura, Egypt
- KMID: 2512036
- DOI: http://doi.org/10.5395/rde.2020.45.e45
Abstract
Objective
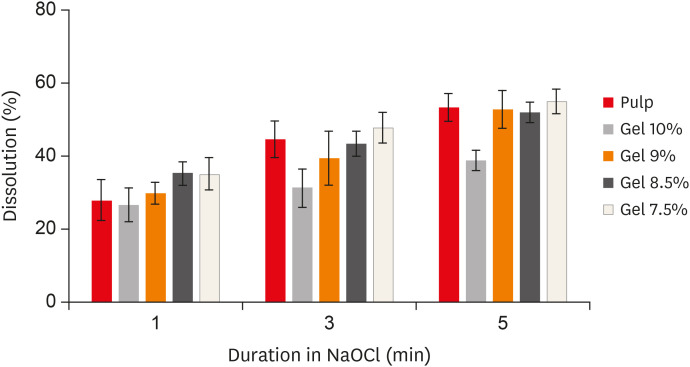
The aim of this study was to introduce a gelatin/bovine serum albumin (BSA) tissue standard, which provides dissolution properties identical to those of biological tissues. Further, the study evaluated whether the utilization of endodontic activating devices led to enhanced phantom dissolution rates.
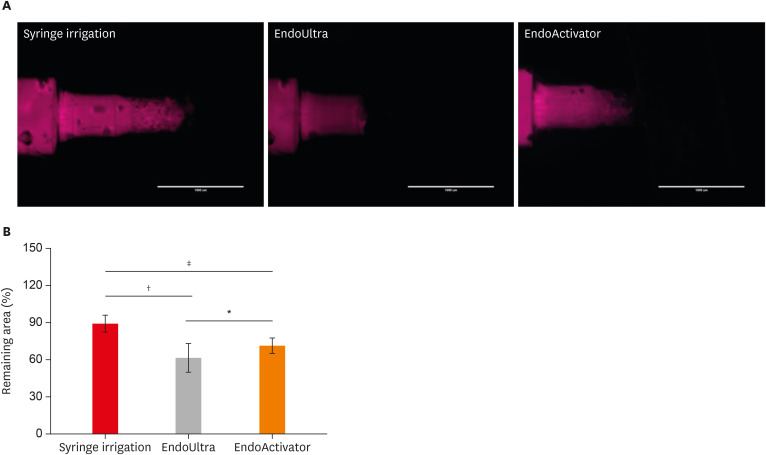
Materials and Methods
Bovine pulp tissue was obtained to determine a benchmark of tissue dissolution. The surface area and mass of samples were held constant while the ratio of gelatin and BSA were varied, ranging from 7.5% to 10% gelatin and 5% BSA. Each sample was placed in an individual test tube that was filled with an appropriate sodium hypochlorite solution for 1, 3, and 5 minutes, and then removed from the solution, blotted dry, and weighed again. The remaining tissue was calculated as the percent of initial tissue to determine the tissue dissolution rate. A radiopaque agent (sodium diatrizoate) and a fluorescent dye (methylene blue) were added to the phantom to allow easy quantification of phantom dissolution in a canal block model when activated using ultrasonic (EndoUltra) or sonic (EndoActivator) energy.
Results
The 9% gelatin + 5% BSA phantom showed statistically equivalent dissolution to bovine pulp tissue at all time intervals. Furthermore, the EndoUltra yielded significantly more phantom dissolution in the canal block than the EndoActivator or syringe irrigation.
Conclusions
Our phantom is comparable to biological tissue in terms of tissue dissolution and could be utilized for in vitro tests due to its injectability and detectability.
Figure
Reference
-
1. Nair PN, Henry S, Cano V, Vera J. Microbial status of apical root canal system of human mandibular first molars with primary apical periodontitis after “one-visit” endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005; 99:231–252. PMID: 15660098.
Article3. Peters OA, Peters CI, Basrani B. Cleaning and shaping of the root canal system. In : Cohen S, Hargreaves KM, editors. Cohen's pathways of the pulp. St. Louis, MO: Elsevier;2006. p. 209–357.4. Clarkson RM, Podlich HM, Savage NW, Moule AJ. A survey of sodium hypochlorite use by general dental practitioners and endodontists in Australia. Aust Dent J. 2003; 48:20–26. PMID: 14640153.
Article5. Naenni N, Thoma K, Zehnder M. Soft tissue dissolution capacity of currently used and potential endodontic irrigants. J Endod. 2004; 30:785–787. PMID: 15505511.6. Baumgartner JC, Cuenin PR. Efficacy of several concentrations of sodium hypochlorite for root canal irrigation. J Endod. 1992; 18:605–612. PMID: 1298800.
Article7. Poggio C, Ceci M, Beltrami R, Colombo M, Dagna A. Viscosity of endodontic irrigants: influence of temperature. Dent Res J (Isfahan). 2015; 12:425–430. PMID: 26604955.
Article8. Cheung GS, Stock CJ. In vitro cleaning ability of root canal irrigants with and without endosonics. Int Endod J. 1993; 26:334–343. PMID: 8144242.
Article9. Yang SF, Rivera EM, Baumgardner KR, Walton RE, Stanford C. Anaerobic tissue-dissolving abilities of calcium hydroxide and sodium hypochlorite. J Endod. 1995; 21:613–616. PMID: 8596083.
Article10. Cunningham WT, Balekjian AY. Effect of temperature on collagen-dissolving ability of sodium hypochlorite endodontic irrigant. Oral Surg Oral Med Oral Pathol. 1980; 49:175–177. PMID: 6928291.
Article11. Zehnder M, Kosicki D, Luder H, Sener B, Waltimo T. Tissue-dissolving capacity and antibacterial effect of buffered and unbuffered hypochlorite solutions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002; 94:756–762. PMID: 12464903.
Article12. Christensen CE, McNeal SF, Eleazer P. Effect of lowering the pH of sodium hypochlorite on dissolving tissue in vitro . J Endod. 2008; 34:449–452. PMID: 18358894.
Article13. Stojicic S, Zivkovic S, Qian W, Zhang H, Haapasalo M. Tissue dissolution by sodium hypochlorite: effect of concentration, temperature, agitation, and surfactant. J Endod. 2010; 36:1558–1562. PMID: 20728727.
Article14. Koskinen KP, Stenvall H, Uitto VJ. Dissolution of bovine pulp tissue by endodontic solutions. Eur J Oral Sci. 1980; 88:406–411.
Article15. Thé SD. The solvent action of sodium hypochlorite on fixed and unfixed necrotic tissue. Oral Surg Oral Med Oral Pathol. 1979; 47:558–561. PMID: 286277.
Article16. Clarkson RM, Moule AJ, Podlich H, Kellaway R, Macfarlane R, Lewis D, Rowell J. Dissolution of porcine incisor pulps in sodium hypochlorite solutions of varying compositions and concentrations. Aust Dent J. 2006; 51:245–251. PMID: 17037892.
Article17. Macedo RG, Wesselink PR, Zaccheo F, Fanali D, Van Der Sluis LW. Reaction rate of NaOCl in contact with bovine dentine: effect of activation, exposure time, concentration and pH. Int Endod J. 2010; 43:1108–1115. PMID: 20812947.
Article18. Cameron JA. The use of 4 per cent sodium hypochlorite, with or without ultrasound, in cleansing of uninstrumented immature root canals; SEM study. Aust Dent J. 1987; 32:204–213. PMID: 3479109.
Article19. Pascon FM, Puppin-Rontani RM. The influence of cleansers on the permeability index of primary tooth root dentin. J Clin Pediatr Dent. 2006; 31:93–97. PMID: 17315802.
Article20. Gu LS, Kim JR, Ling J, Choi KK, Pashley DH, Tay FR. Review of contemporary irrigant agitation techniques and devices. J Endod. 2009; 35:791–804. PMID: 19482174.
Article21. Christo JE, Zilm PS, Sullivan T, Cathro PR. Efficacy of low concentrations of sodium hypochlorite and low-powered Er,Cr:YSGG laser activated irrigation against an Enterococcus faecalis biofilm. Int Endod J. 2016; 49:279–286. PMID: 25772335.
Article22. Linde A. The extracellular matrix of the dental pulp and dentin. J Dent Res. 1985; 64 Spec No:523–529. PMID: 3857252.23. de Almeida LH, Leonardo NG, Gomes AP, Giardino L, Souza EM, Pappen FG. Pulp tissue dissolution capacity of sodium hypochlorite combined with cetrimide and polypropylene glycol. Braz Dent J. 2013; 24:477–481. PMID: 24474288.
Article24. Selvam S, Sarkar I. Bile salt induced solubilization of methylene blue: study on methylene blue fluorescence properties and molecular mechanics calculation. J Pharm Anal. 2017; 7:71–75. PMID: 29404020.
Article25. Culjat MO, Goldenberg D, Tewari P, Singh RS. A review of tissue substitutes for ultrasound imaging. Ultrasound Med Biol. 2010; 36:861–873. PMID: 20510184.
Article26. Moffitt T, Chen YC, Prahl SA. Preparation and characterization of polyurethane optical phantoms. J Biomed Opt. 2006; 11:041103. PMID: 16965131.
Article27. Pogue BW, Patterson MS. Review of tissue simulating phantoms for optical spectroscopy, imaging and dosimetry. J Biomed Opt. 2006; 11:041102. PMID: 16965130.
Article28. Kutty SK, Lekshmi MS, Mohan A, Isaac L. Pulp tissue dissolution in endodontics- A review. Int J Appl Dent Sci. 2017; 3:193–196.29. Frank RM, Nalbandian J. Structure and ultrastructure of the dental pulp. In : Berkovitz BK, Boyde A, Frank RM, Höhling HJ, Moxham BJ, Nalbandian J, Tonge CH, editors. Teeth. Berlin: Springer;1989. p. 249–307.30. Madsen EL, Zagzebski JA, Banjavie RA, Jutila RE. Tissue mimicking materials for ultrasound phantoms. Med Phys. 1978; 5:391–394. PMID: 713972.
Article31. Hand RE, Smith ML, Harrison JW. Analysis of the effect of dilution on the necrotic tissue dissolution property of sodium hypochlorite. J Endod. 1978; 4:60–64. PMID: 277629.
Article32. Türkün M, Cengiz T. The effects of sodium hypochlorite and calcium hydroxide on tissue dissolution and root canal cleanliness. Int Endod J. 1997; 30:335–342. PMID: 9477824.
Article33. Beltz RE, Torabinejad M, Pouresmail M. Quantitative analysis of the solubilizing action of MTAD, sodium hypochlorite, and EDTA on bovine pulp and dentin. J Endod. 2003; 29:334–337. PMID: 12775005.
Article34. Abou-Rass M, Oglesby SW. The effects of temperature, concentration, and tissue type on the solvent ability of sodium hypochlorite. J Endod. 1981; 7:376–377. PMID: 6943272.
Article35. Moorer WR, Wesselink PR. Factors promoting the tissue dissolving capability of sodium hypochlorite. Int Endod J. 1982; 15:187–196. PMID: 6964523.
Article36. Estrela C, Estrela CR, Barbin EL, Spanó JC, Marchesan MA, Pécora JD. Mechanism of action of sodium hypochlorite. Braz Dent J. 2002; 13:113–117. PMID: 12238801.
Article37. Ahmad M, Pitt Ford TR, Crum LA. Ultrasonic debridement of root canals: an insight into the mechanisms involved. J Endod. 1987; 13:93–101. PMID: 3471836.
Article38. Cameron JA. The synergistic relationship between ultrasound and sodium hypochlorite: a scanning electron microscope evaluation. J Endod. 1987; 13:541–545. PMID: 3482099.
Article39. Weller RN, Brady JM, Bernier WE. Efficacy of ultrasonic cleaning. J Endod. 1980; 6:740–743. PMID: 6935384.
Article40. Sabins RA, Johnson JD, Hellstein JW. A comparison of the cleaning efficacy of short-term sonic and ultrasonic passive irrigation after hand instrumentation in molar root canals. J Endod. 2003; 29:674–678. PMID: 14606795.
Article41. Mayer BE, Peters OA, Barbakow F. Effects of rotary instruments and ultrasonic irrigation on debris and smear layer scores: a scanning electron microscopic study. Int Endod J. 2002; 35:582–589. PMID: 12190897.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Correction of missing funding information. A new phantom to evaluate the tissue dissolution ability of endodontic irrigants and activating devices
- Interaction of Hydroxyethylidene bisphosphonate (HEBP) with other endodontic irrigants on tissue dissolving capacity and antimicrobial effect
- Chemically induced osteomyelitis in the mandible: A case report
- Accuracy of Root ZX in teeth with simulated root perforation in the presence of gel or liquid type endodontic irrigant
- Comparison of various activation methods of root canal irrigants for soft-tissue removal