Obstet Gynecol Sci.
2021 Jan;64(1):114-121. 10.5468/ogs.20242.
Endometrial polyps: Is the prediction of spontaneous regression possible?
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Saglik Bilimleri University, Gaziosmanpasa Training and Research Hospital, Gaziosmanpasa/İstanbul, Turkey
- 2Department of Obstetrics and Gynecology, Saglik Bilimleri University, Istanbul Kanuni Sultan Suleyman Training and Research Hospital, Küçükçekmece/İstanbul, Turkey
- KMID: 2511572
- DOI: http://doi.org/10.5468/ogs.20242
Abstract
Objective
Endometrial polyps have been considered as a hyperplastic growth of endometrial stromal and glandular tissues. Even asymptomatic polyps in premenopausal women are usually removed as soon as they are diagnosed, although it is still unknown how often endometrial polyps disappear spontaneously. The aim of this study was to investigate the regression rate of endometrial polyps and the possible factors related to their spontaneous regression.
Methods
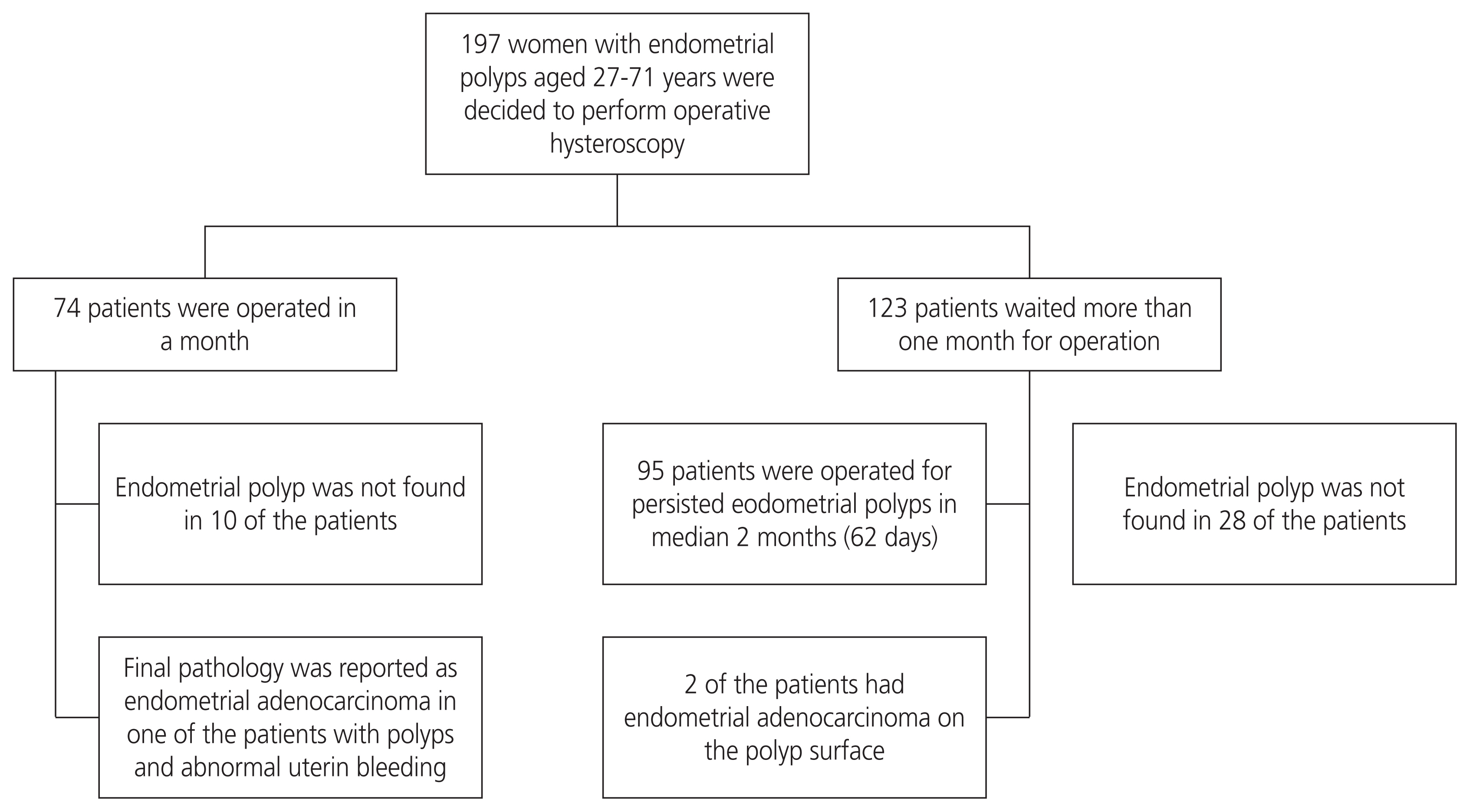
A total of 197 women with endometrial polyps were treated with operative hysteroscopy between January 2017 and April 2019 at our tertiary center. Of these, 123 patients who preferred conservative follow-up were enrolled in the study. Clinical and pathological data were obtained from electronic medical records.
Results
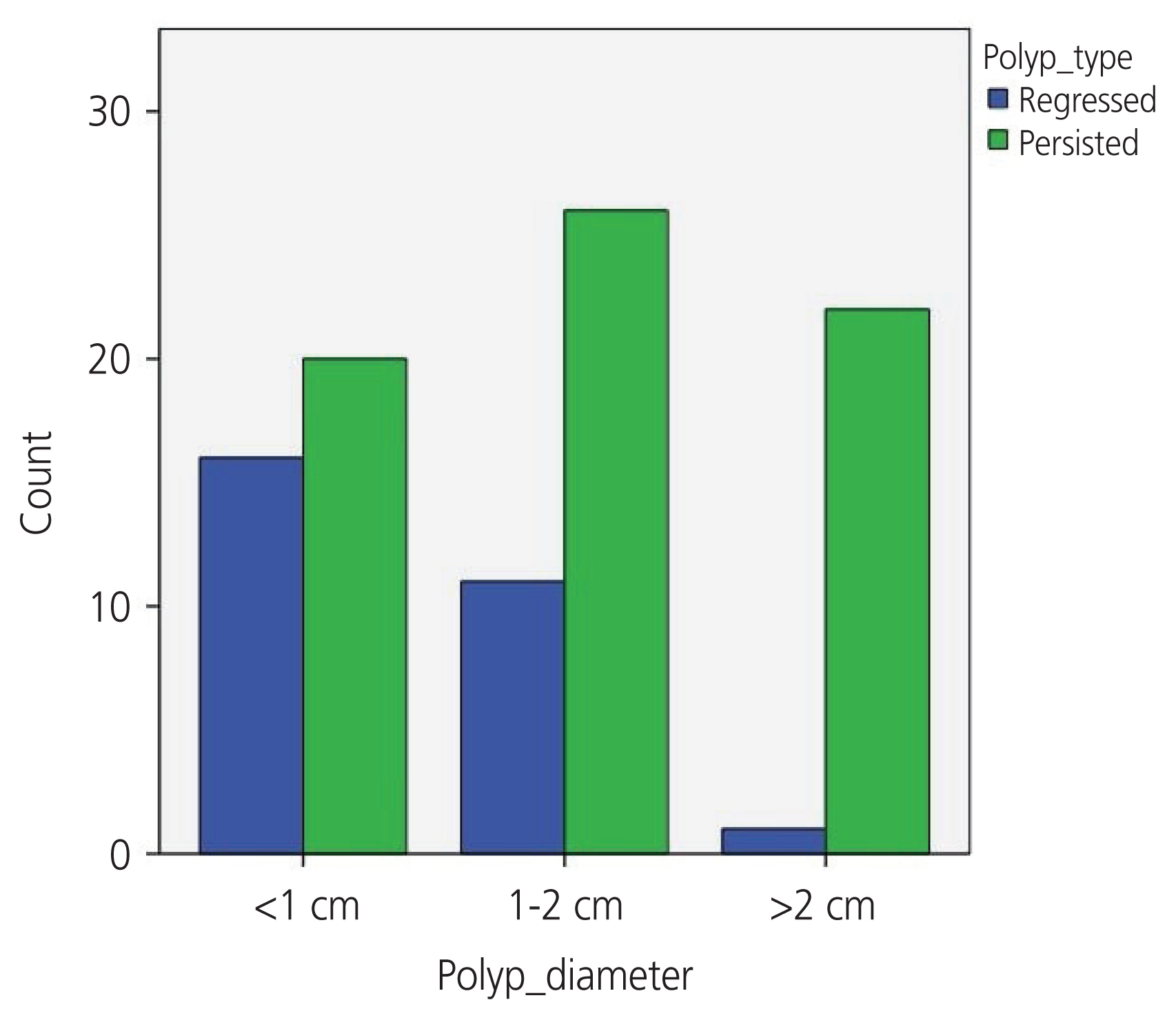
Patients with endometrial polyps were followed up for a median period of 62 days (range 30–360 days). Most women with endometrial polyps (84%) were reported to have gynecologic symptoms. Spontaneous polyp regression was observed in 28 (23%) patients who underwent surgery reevaluation. Patient age (<45 years), premenopausal period, and polyp size (<2 cm) were found to be associated with spontaneous endometrial polyp regression (P<0.05). We also observed more polyp regression in women with abnormal uterine bleeding (P=0.05). Second-look hysteroscopy showed that all postmenopausal women had persistent endometrial polyps.
Conclusion
Patient age (<45 years), premenopausal period, polyp size (<2 cm), and abnormal uterine bleeding may be associated with spontaneous endometrial polyp regression.
Figure
Cited by 1 articles
-
Surgical outcomes of laparoscopic trachelectomy following supracervical hysterectomy: a multicenter study
Ayman Shehata Dawood, Heba Fouad Harras, Hossam Ramadan Moussa, Ahmed Saber Soliman
Obstet Gynecol Sci. 2022;65(6):542-551. doi: 10.5468/ogs.22094.
Reference
-
References
1. Tanos V, Berry KE, Seikkula J, Abi Raad E, Stavroulis A, Sleiman Z, et al. The management of polyps in female reproductive organs. Int J Surg. 2017; 43:7–16.
Article2. Dreisler E, Stampe Sorensen S, Ibsen PH, Lose G. Prevalence of endometrial polyps and abnormal uterine bleeding in a Danish population aged 20–74 years. Ultrasound Obstet Gynecol. 2009; 33:102–8.
Article3. Uglietti A, Buggio L, Farella M, Chiaffarino F, Dridi D, Vercellini P, et al. The risk of malignancy in uterine polyps: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2019; 237:48–56.
Article4. Lieng M, Istre O, Sandvik L, Qvigstad E. Prevalence, 1-year regression rate, and clinical significance of asymptomatic endometrial polyps: cross-sectional study. J Minim Invasive Gynecol. 2009; 16:465–71.
Article5. Wong M, Crnobrnja B, Liberale V, Dharmarajah K, Widschwendter M, Jurkovic D. The natural history of endometrial polyps. Hum Reprod. 2017; 32:340–5.
Article6. Valentin L. Imaging techniques in the management of abnormal vaginal bleeding in non-pregnant women before and after menopause. Best Pract Res Clin Obstet Gynaecol. 2014; 28:637–54.
Article7. American Association of Gynecologic Laparoscopists. AAGL practice report: practice guidelines for the diagnosis and management of endometrial polyps. J Minim Invasive Gynecol. 2012; 19:3–10.8. DeWaay DJ, Syrop CH, Nygaard IE, Davis WA, Van Voorhis BJ. Natural history of uterine polyps and leiomyomata. Obstet Gynecol. 2002; 100:3–7.
Article9. Salim S, Won H, Nesbitt-Hawes E, Campbell N, Abbott J. Diagnosis and management of endometrial polyps: a critical review of the literature. J Minim Invasive Gynecol. 2011; 18:569–81.
Article10. Ferenczy A. Pathophysiology of endometrial bleeding. Maturitas. 2003; 45:1–14.
Article11. Strickland KC, Yuan L, Quade BJ, Nucci MR, Howitt BE. Clinicopathological and immunohistochemical features of uterine adenomyomatous polyps. Hum Pathol. 2019; 84:239–45.
Article12. Sasaki LMP, Andrade KRC, Figueiredo ACMG, Wanderley MDS, Pereira MG. Factors associated with malignancy in hysteroscopically resected endometrial polyps: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2018; 25:777–85.
Article13. Kilicdag EB, Haydardedeoglu B, Cok T, Parlakgumus AH, Simsek E, Bolat FA. Polycystic ovary syndrome and increased polyp numbers as risk factors for malignant transformation of endometrial polyps in premenopausal women. Int J Gynaecol Obstet. 2011; 112:200–3.
Article14. Jiang T, Yuan Q, Zhou Q, Zhu Y, Lv S, Cao Y, et al. Do endometrial lesions require removal? A retrospective study. BMC Womens Health. 2019; 19:61.
Article15. De Azevedo JM, De Azevedo LM, Freitas F, Wender MC. Endometrial polyps: When to resect? Arch Gynecol Obstet. 2016; 293:639–43.
Article16. Pereira AK, Garcia MT, Pinheiro W, Ejzenberg D, Soares JM Jr, Baracat EC. What is the influence of cyclooxygenase-2 on postmenopausal endometrial polyps? Climacteric. 2015; 18:498–502.
Article17. Gu F, Zhang H, Ruan S, Li J, Liu X, Xu Y, et al. High number of endometrial polyps is a strong predictor of recurrence: findings of a prospective cohort study in reproductive-age women. Fertil Steril. 2018; 109:493–500.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Detection of changes in endometrial polyps by sonohysterography
- Spontaneous Regression of Hyperplastic Gastric Polyps
- Investigation of the Roles of Cyclooxygenase-2 and Galectin-3 Expression in the Pathogenesis of Premenopausal Endometrial Polyps
- Management of endometrial polyps in infertile women: A mini-review
- The rate of malignant endometrial polyps and it's associated factors