Obstet Gynecol Sci.
2021 Jan;64(1):27-33. 10.5468/ogs.20206.
Role of repeat procalcitonin estimation at 48 hours for outcome in pregnancy associated sepsis: a prospective observational study
- Affiliations
-
- 1Department of Obstetrics &Gynaecology, University College of Medical Sciences & Guru Teg Bahadur Hospital, Delhi, India
- 2Department of Biochemistry, University College of Medical Sciences & Guru Teg Bahadur Hospital, Delhi, India
- 3Department of Anaesthesia, University College of Medical Sciences & Guru Teg Bahadur Hospital, Delhi, India
- KMID: 2511562
- DOI: http://doi.org/10.5468/ogs.20206
Abstract
Objectives
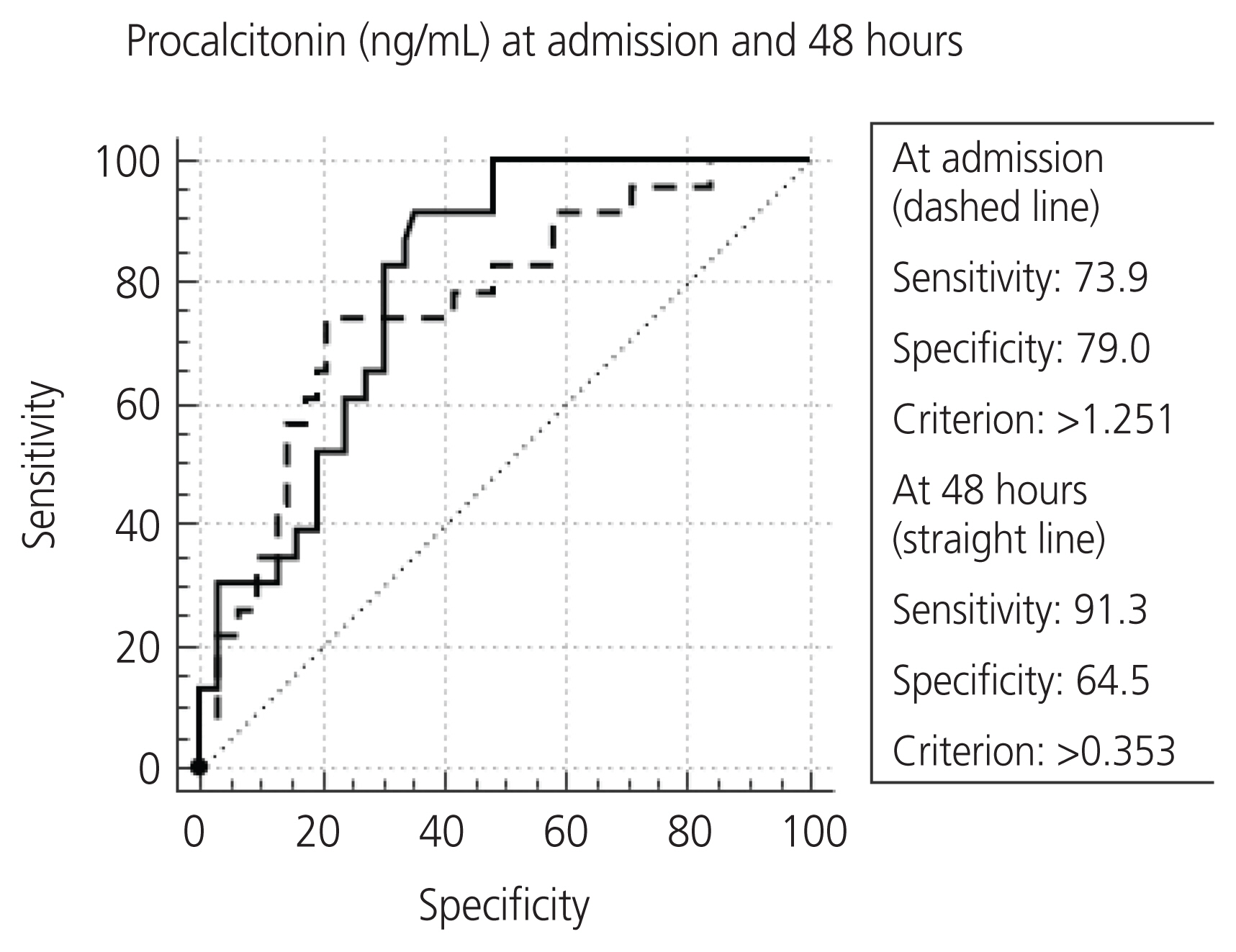
We assessed whether repeat procalcitonin (PCT) estimation has a role in detecting organ dysfunctions and mortality in pregnancy associated sepsis (PAS).
Methods
The study included 85 pregnant, post-abortal, and postpartum women with PAS, diagnosed using the quick Sequential Organ Failure Assessment criteria. Median interquartile range PCT levels were documented at admission and 48 hours later. Statistical comparisons were performed between the groups with non-severe and severe (≥1 organ failure) PAS, and between the survivor and mortality groups. The relationship between PCT and the number of organ failures was also assessed.
Results
Most of the subjects with PAS were young and in the postpartum period (mean age 26 years; postpartum 55%). Sixteen (19%) patients died due to PAS. Sixty-two patients (74%) had severe PAS at presentation. Bacteria were isolated on culture in 64% of the subjects. PCT levels at admission were higher in patients with severe PAS than in those who did not have severe PAS. At 48 hours, this difference was significant (P=0.014; severe PAS 2.23 ng/mL vs. non-severe PAS 0.20 ng/mL). Furthermore, the number of organ failures increased at 48 hours. The PCT levels were significantly higher in the mortality group than in the survivors’ group at admission (8.31 ng/mL vs. 1.72 ng/mL), and the difference increased further at 48 hours (9.54 ng/mL vs. 1.37 ng/mL).
Conclusion
Repeat PCT estimation at 48 hours could complement the clinical findings and enhance the prognostic value for PAS.
Keyword
Figure
Reference
-
References
1. Meisner M. Current status of procalcitonin in the ICU. Neth J Crit Care. 2013; 17:4–12.2. Wacker C, Prkno A, Brunkhorst FM, Schlattmann P. Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis. 2013; 13:426–35.
Article3. Paccolat C, Harbarth S, Courvoisier D, Irion O, de Tejada BM. Procalcitonin levels during pregnancy, delivery and postpartum. J Perinat Med. 2011; 39:679–83.
Article4. Duckworth S, Griffin M, Seed PT, North R, Myers J, Mackillop L, et al. Diagnostic biomarkers in women with suspected preeclampsia in a prospective multicentre study. Obstet Gynecol. 2016; 128:245–52.5. Ducarme G, Desroys du Roure F, Le Thuaut A, Grange J, Vital M, Dimet J. Efficacy of serum procalcitonin to predict spontaneous preterm birth in women with threatened preterm labour: a prospective observational study. BMC Pregnancy Childbirth. 2018; 18:65.
Article6. Bilir F, Akdemir N, Ozden S, Cevrioglu AS, Bilir C. Increased serum procalcitonin levels in pregnant patients with asymptomatic bacteriuria. Ann Clin Microbiol Antimicrob. 2013; 12:25.
Article7. Velasquez J, Zuleta J, Portilla P, Caicedo K, Portilla L, Patiño J. Usefulness of measuring procalcitonin (PTC) in pregnancy for the initial diagnosis of bacterial infection with systemic features. Am J Obstet Gynecol. 2018; 218:S514–5.8. Agarwal R, Priyadarshini P, Mehndiratta M. Serum procalcitonin in pregnancy-associated sepsis: a case control study. S Afr J Obstet Gynaecol. 2019; 25:15–9.
Article9. Society for Maternal-Fetal Medicine (SMFM). Plante LA, Pacheco LD, Louis JM. SMFM Consult Series #47: Sepsis during pregnancy and the puerperium. Am J Obstet Gynecol. 2019; 220:B2–10.
Article10. Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003; 31:1250–6.
Article11. Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis Campaign: International guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017; 43:304–77.12. Oud L. Pregnancy-associated severe sepsis. Curr Opin Obstet Gynecol. 2016; 28:73–8.
Article13. AlRawahi AN, AlHinai FA, Doig CJ, Ball CG, Dixon E, Xiao Z, et al. The prognostic value of serum procalcitonin measurements in critically injured patients: a systematic review. Crit Care. 2019; 23:390.
Article14. Cabral L, Afreixo V, Almeida L, Paiva JA. The use of procalcitonin (PCT) for diagnosis of sepsis in burn patients: a meta-analysis. PLoS One. 2016; 11:e0168475.
Article15. González-Fernández D, Pons ED, Rueda D, Sinisterra OT, Murillo E, Scott ME, et al. C-reactive protein is differentially modulated by co-existing infections, vitamin deficiencies and maternal factors in pregnant and lactating indigenous Panamanian women. Infect Dis Poverty. 2017; 6:94.
Article16. Azizia MM, Irvine LM, Coker M, Sanusi FA. The role of C-reactive protein in modern obstetric and gynecological practice. Acta Obstet Gynecol Scand. 2006; 85:394–401.
Article17. Hattori T, Nishiyama H, Kato H, Ikegami S, Nagayama M, Asami S, et al. Clinical value of procalcitonin for patients with suspected bloodstream infection. Am J Clin Pathol. 2014; 141:43–51.
Article18. Laukemann S, Kasper N, Kulkarni P, Steiner D, Rast AC, Kutz A, et al. Can we reduce negative blood cultures with clinical scores and blood markers? Results from an observational cohort study. Medicine (Baltimore). 2015; 94:e2264.
Article19. Trásy D, Tánczos K, Németh M, Hankovszky P, Lovas A, Mikor A, et al. Delta procalcitonin is a better indicator of infection than absolute procalcitonin values in critically ill patients: a prospective observational study. J Immunol Res. 2016; 2016:3530752.
Article20. Sharma P, Patel K, Baria K, Lakhia K, Malhotra A, Shah K, et al. Procalcitonin level for prediction of postoperative infection in cardiac surgery. Asian Cardiovasc Thorac Ann. 2016; 24:344–9.
Article21. Jhan JY, Huang YT, Shih CH, Yang JD, Lin YT, Lin SJ, et al. Procalcitonin levels to predict bacterial infection in surgical intensive care unit patients. Formos J Surg. 2017; 50:135–41.22. Andriolo BN, Andriolo RB, Salomão R, Atallah ÁN. Effectiveness and safety of procalcitonin evaluation for reducing mortality in adults with sepsis, severe sepsis or septic shock. Cochrane Database Syst Rev. 2017; 1:CD010959.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Serum procalcitonin and C-reactive protein as indices of early sepsis and mortality in North Indian pediatric burn injuries: a prospective evaluation and literature review
- The value of presepsin, procalcitonin, and C-reactive protein in sepsis associated organ failure in the emergency department: a retrospective analysis according to the Sepsis-3 definition
- The predictive value of procalcitonin for septic shock in sepsis patients
- Clinical utility of procalcitonin in severe odontogenic maxillofacial infection
- Significance of Biomarkers as a Predictive Factor for Post-Traumatic Sepsis