Ann Clin Neurophysiol.
2020 Oct;22(2):67-74. 10.14253/acn.2020.22.2.67.
Vestibular-evoked myogenic potentials: principle and clinical findings
- Affiliations
-
- 1Dizziness Center, Clinical Neuroscience Center, Department of Neurology, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2511081
- DOI: http://doi.org/10.14253/acn.2020.22.2.67
Abstract
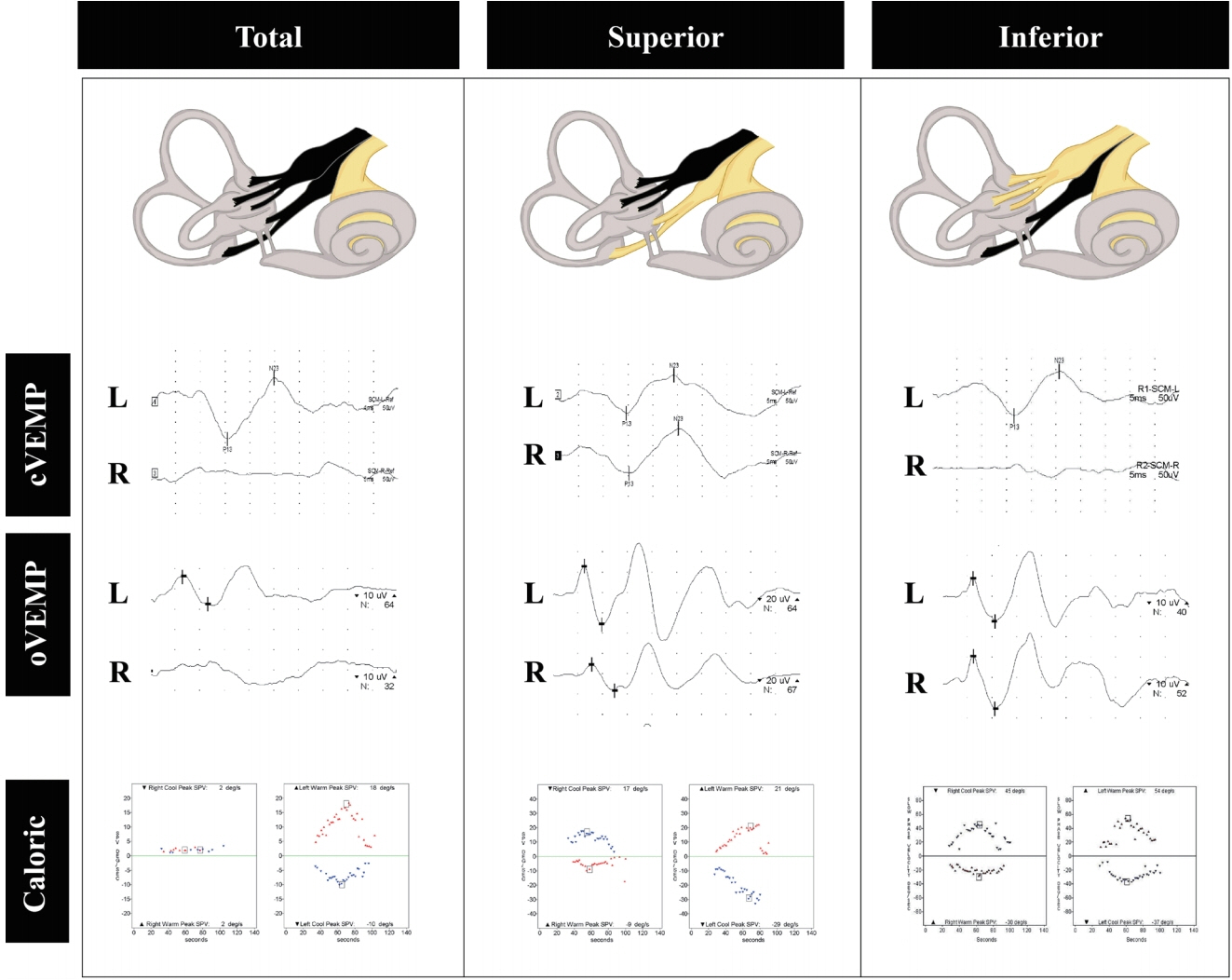
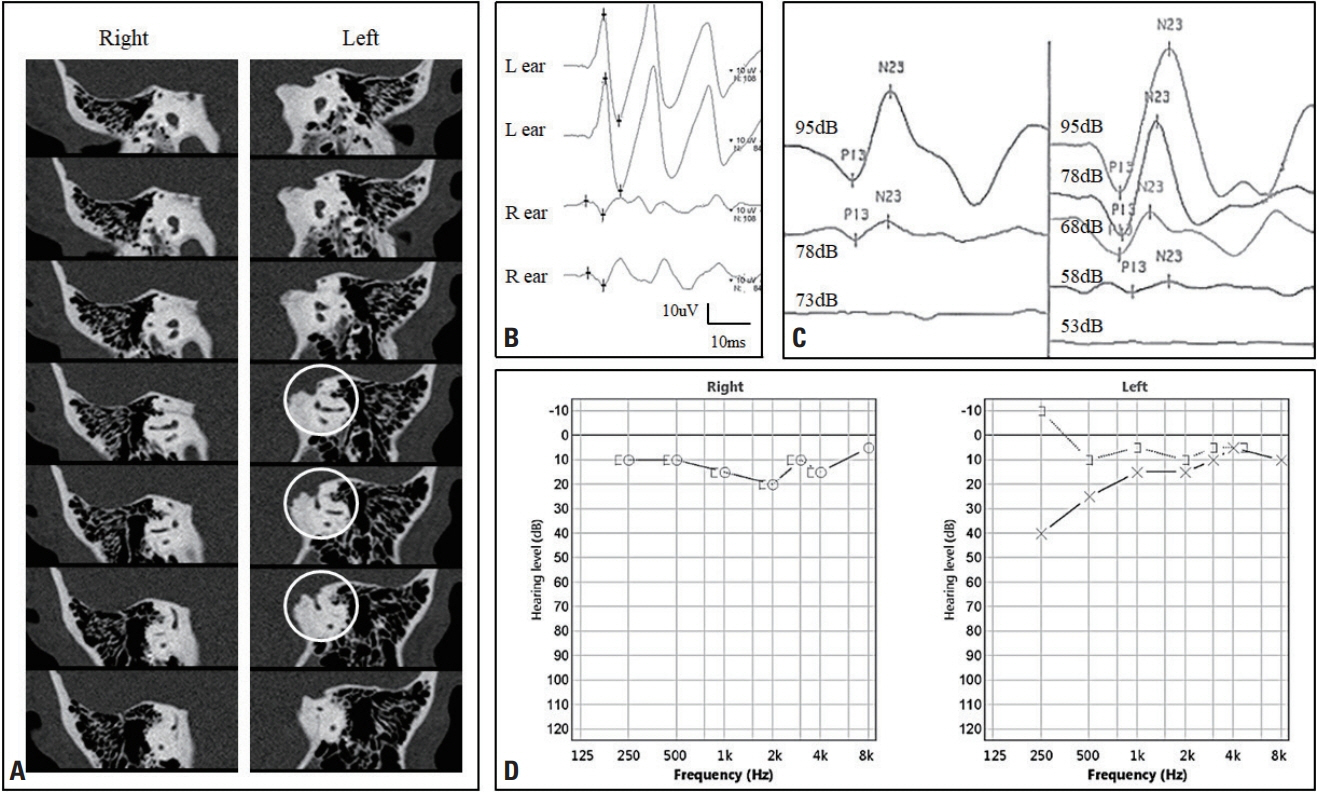
- Vestibular-evoked myogenic potentials (VEMPs) are useful for evaluating the vestibulocollic reflex arising mostly from the saccule and the vestibuloocular reflex originating from the utricle. VEMPs can vary with the characteristics of the applied stimuli and the effects of aging and diseases. VEMPs have been found to be useful for diagnosing superior canal dehiscence, but their usefulness for other clinical disorders remains unclear. This review discusses the principles of VEMP tests and summarizes the findings for VEMPs in common vestibular disorders.
Figure
Reference
-
1. Fife TD, Colebatch JG, Kerber KA, Brantberg K, Strupp M, Lee H, et al. Practice guideline: cervical and ocular vestibular evoked myogenic potential testing: report of the guideline development, dissemination, and implementation subcommittee of the American Academy of Neurology. Neurology. 2017; 89:2288–2296.2. Rosengren SM, Colebatch JG, Young AS, Govender S, Welgampola MS. Vestibular evoked myogenic potentials in practice: Methods, pitfalls and clinical applications. Clin Neurophysiol Pract. 2019; 4:47–68.
Article3. Colebatch JG, Halmagyi GM, Skuse NF. Myogenic potentials generated by a click-evoked vestibulocollic reflex. J Neurol Neurosurg Psychiatry. 1994; 57:190–197.
Article4. Welgampola MS, Colebatch JG. Vestibulocollic reflexes: normal values and the effect of age. Clin Neurophysiol. 2001; 112:1971–1979.
Article5. Todd NP, Rosengren SM, Aw ST, Colebatch JG. Ocular vestibular evoked myogenic potentials (OVEMPs) produced by air- and bone-conducted sound. Clin Neurophysiol. 2007; 118:381–390.
Article6. Rosengren SM, McAngus Todd NP, Colebatch JG. Vestibular-evoked extraocular potentials produced by stimulation with bone-conducted sound. Clin Neurophysiol. 2005; 116:1938–1948.
Article7. Young ED, Fernández C, Goldberg JM. Responses of squirrel monkey vestibular neurons to audio-frequency sound and head vibration. Acta Otolaryngol. 1977; 84:352–360.
Article8. McCue MP, Guinan JJ Jr. Spontaneous activity and frequency selectivity of acoustically responsive vestibular afferents in the cat. J Neurophysiol. 1995; 74:1563–1572.
Article9. Lin MY, Timmer FC, Oriel BS, Zhou G, Guinan JJ, Kujawa SG, et al. Vestibular evoked myogenic potentials (VEMP) can detect asymptomatic saccular hydrops. Laryngoscope. 2006; 116:987–992.
Article10. Taylor RL, Bradshaw AP, Halmagyi GM, Welgampola MS. Tuning characteristics of ocular and cervical vestibular evoked myogenic potentials in intact and dehiscent ears. Audiol Neurootol. 2012; 17:207–218.
Article11. Vanspauwen R, Wuyts FL, Van De Heyning PH. Validity of a new feedback method for the VEMP test. Acta Otolaryngol. 2006; 126:796–800.
Article12. Rosengren SM. Effects of muscle contraction on cervical vestibular evoked myogenic potentials in normal subjects. Clin Neurophysiol. 2015; 126:2198–2206.
Article13. Lee KJ, Kim MS, Son EJ, Lim HJ, Bang JH, Kang JG. The usefulness of rectified VEMP. Clin Exp Otorhinolaryngol. 2008; 1:143–147.
Article14. Lee SU, Kim HJ, Choi JY, Koo JW, Kim JS. Abnormal cervical vestibular-evoked myogenic potentials predict evolution of isolated recurrent vertigo into Meniere’s disease. Front Neurol. 2017; 8:463.
Article15. Rosengren SM, Colebatch JG, Straumann D, Weber KP. Why do oVEMPs become larger when you look up? Explaining the effect of gaze elevation on the ocular vestibular evoked myogenic potential. Clin Neurophysiol. 2013; 124:785–791.
Article16. Piker EG, Jacobson GP, Burkard RF, McCaslin DL, Hood LJ. Effects of age on the tuning of the cVEMP and oVEMP. Ear Hear. 2013; 34:e65–e73.
Article17. Maxwell R, Jerin C, Gürkov R. Utilisation of multi-frequency VEMPs improves diagnostic accuracy for Meniere’s disease. Eur Arch Otorhinolaryngol. 2017; 274:85–93.
Article18. Rauch SD, Zhou G, Kujawa SG, Guinan JJ, Herrmann BS. Vestibular evoked myogenic potentials show altered tuning in patients with Ménière’s disease. Otol Neurotol. 2004; 25:333–338.
Article19. Node M, Seo T, Miyamoto A, Adachi A, Hashimoto M, Sakagami M. Frequency dynamics shift of vestibular evoked myogenic potentials in patients with endolymphatic hydrops. Otol Neurotol. 2005; 26:1208–1213.
Article20. Winters SM, Berg IT, Grolman W, Klis SF. Ocular vestibular evoked myogenic potentials: frequency tuning to air-conducted acoustic stimuli in healthy subjects and Ménière’s disease. Audiol Neurootol. 2012; 17:12–19.
Article21. Sandhu JS, Low R, Rea PA, Saunders NC. Altered frequency dynamics of cervical and ocular vestibular evoked myogenic potentials in patients with Ménière’s disease. Otol Neurotol. 2012; 33:444–449.
Article22. Manzari L, Burgess AM, McGarvie LA, Curthoys IS. Ocular and cervical vestibular evoked myogenic potentials to 500 Hz fz bone-conducted vibration in superior semicircular canal dehiscence. Ear Hear. 2012; 33:508–520.
Article23. Rosengren SM, Aw ST, Halmagyi GM, Todd NP, Colebatch JG. Ocular vestibular evoked myogenic potentials in superior canal dehiscence. J Neurol Neurosurg Psychiatry. 2008; 79:559–568.
Article24. Govender S, Fernando T, Dennis DL, Welgampola MS, Colebatch JG. Properties of 500Hz air- and bone-conducted vestibular evoked myogenic potentials (VEMPs) in superior canal dehiscence. Clin Neurophysiol. 2016; 127:2522–2531.
Article25. Roditi RE, Eppsteiner RW, Sauter TB, Lee DJ. Cervical vestibular evoked myogenic potentials (cVEMPs) in patients with superior canal dehiscence syndrome (SCDS). Otolaryngol Head Neck Surg. 2009; 141:24–28.
Article26. Kim JS. When the room is spinning: experience of vestibular neuritis by a neurotologist. Front Neurol. 2020; 11:157.
Article27. Jeong SH, Kim HJ, Kim JS. Vestibular neuritis. Semin Neurol. 2013; 33:185–194.
Article28. Kim HA, Hong JH, Lee H, Yi HA, Lee SR, Lee SY, et al. Otolith dysfunction in vestibular neuritis: recovery pattern and a predictor of symptom recovery. Neurology. 2008; 70:449–453.
Article29. Shin BS, Oh SY, Kim JS, Kim TW, Seo MW, Lee H, et al. Cervical and ocular vestibular-evoked myogenic potentials in acute vestibular neuritis. Clin Neurophysiol. 2012; 123:369–375.
Article30. Kim JS, Kim HJ. Inferior vestibular neuritis. J Neurol. 2012; 259:1553–1560.
Article31. Park JY, Choi SY, Choi JH, Choi KD. Vestibular neuritis selectively involving posterior canal and utricle. J Neurol. 2018; 265:1940–1942.
Article32. Lopez-Escamez JA, Carey J, Chung WH, Goebel JA, Magnusson M, Mandalà M, et al. Diagnostic criteria for Ménière’s disease. J Vestib Res. 2015; 25:1–7.33. Sperling NM, Paparella MM, Yoon TH, Zelterman D. Symptomatic versus asymptomatic endolymphatic hydrops: a histopathologic comparison. Laryngoscope. 1993; 103:277–285.34. Wu CL, Young YH. Vestibular evoked myogenic potentials in acute low-tone sensorineural hearing loss. Laryngoscope. 2004; 114:2172–2175.
Article35. Singh NK, Barman A. Frequency-amplitude ratio of ocular vestibular-evoked myogenic potentials for detecting Ménière’s disease: a preliminary investigation. Ear Hear. 2016; 37:365–373.36. Murofushi T, Tsubota M, Suizu R, Yoshimura E. Is alteration of tuning property in cervical vestibular-evoked myogenic potential specific for Ménière’s disease? Front Neurol. 2017; 8:193.
Article37. Lempert T, Olesen J, Furman J, Waterston J, Seemungal B, Carey J, et al. Vestibular migraine: diagnostic criteria. J Vestib Res. 2012; 22:167–172.
Article38. Espinosa-Sanchez JM, Lopez-Escamez JA. New insights into pathophysiology of vestibular migraine. Front Neurol. 2015; 6:12.
Article39. Zaleski A, Bogle J, Starling A, Zapala DA, Davis L, Wester M, et al. Vestibular evoked myogenic potentials in patients with vestibular migraine. Otol Neurotol. 2015; 36:295–302.
Article40. Makowiec KF, Piker EG, Jacobson GP, Ramadan NM, Roberts RA. Ocular and cervical vestibular evoked myogenic potentials in patients with vestibular migraine. Otol Neurotol. 2018; 39:e561–e567.
Article41. Dlugaiczyk J, Habs M, Dieterich M. Vestibular evoked myogenic potentials in vestibular migraine and Ménière’s disease: cVEMPs make the difference. J Neurol. 2020; Jun. 3. [Epub]. DOI:10.1007/s00415-020-09902-4.42. Salviz M, Yuce T, Acar H, Taylan I, Yuceant GA, Karatas A. Diagnostic value of vestibular-evoked myogenic potentials in Ménière’s disease and vestibular migraine. J Vestib Res. 2016; 25:261–266.
Article43. Radtke A, Lempert T, Gresty MA, Brookes GB, Bronstein AM, Neuhauser H. Migraine and Ménière’s disease: is there a link? Neurology. 2002; 59:1700–1704.44. Murofushi T, Tsubota M, Kitao K, Yoshimura E. Simultaneous presentation of definite vestibular migraine and definite Ménière’s disease: overlapping syndrome of two diseases. Front Neurol. 2018; 9:749.
Article45. Balatsouras DG, Ganelis P, Aspris A, Economou NC, Moukos A, Koukoutsis G. Benign paroxysmal positional vertigo associated with Meniere’s disease: epidemiological, pathophysiologic, clinical, and therapeutic aspects. Ann Otol Rhinol Laryngol. 2012; 121:682–688.
Article46. Mandalà M, Santoro GP, Awrey J, Nuti D. Vestibular neuritis: recurrence and incidence of secondary benign paroxysmal positional vertigo. Acta Otolaryngol. 2010; 130:565–567.
Article47. Oya R, Imai T, Takenaka Y, Sato T, Oshima K, Ohta Y, et al. Clinical significance of cervical and ocular vestibular evoked myogenic potentials in benign paroxysmal positional vertigo: a meta-analysis. Eur Arch Otorhinolaryngol. 2019; 276:3257–3265.
Article48. Kim EJ, Oh SY, Kim JS, Yang TH, Yang SY. Persistent otolith dysfunction even after successful repositioning in benign paroxysmal positional vertigo. J Neurol Sci. 2015; 358:287–293.
Article49. Lee JD, Park MK, Lee BD, Lee TK, Sung KB, Park JY. Abnormality of cervical vestibular-evoked myogenic potentials and ocular vestibular-evoked myogenic potentials in patients with recurrent benign paroxysmal postitional vertigo. Acta Otolaryngol. 2013; 133:150–153.
Article50. Yetiser S, Ince D, Gul M. An analysis of vestibular evoked myogenic potentials in patients with benign paroxysmal positional vertigo. Ann Otol Rhinol Laryngol. 2014; 123:686–695.
Article51. Minor LB, Solomon D, Zinreich JS, Zee DS. Sound- and/or pressure-induced vertigo due to bone dehiscence of the superior semicircular canal. Arch Otolaryngol Head Neck Surg. 1998; 124:249–258.
Article52. Ward BK, Carey JP, Minor LB. Superior canal dehiscence syndrome: lessons from the first 20 years. Front Neurol. 2017; 8:177.
Article53. Welgampola MS, Myrie OA, Minor LB, Carey JP. Vestibular-evoked myogenic potential thresholds normalize on plugging superior canal dehiscence. Neurology. 2008; 70:464–472.
Article54. Newlands SD, Vrabec JT, Purcell IM, Stewart CM, Zimmerman BE, Perachio AA. Central projections of the saccular and utricular nerves in macaques. J Comp Neurol. 2003; 466:31–47.
Article55. Kim HJ, Kim S, Park JH, Kim JS. Altered processing of otolithic information in isolated lateral medullary infarction. J Neurol. 2016; 263:2424–2429.
Article56. Venhovens J, Meulstee J, Verhagen WIM. Vestibular evoked myogenic potentials (VEMPs) in central neurological disorders. Clin Neurophysiol. 2016; 127:40–49.
Article57. Oh SY, Kim HJ, Kim JS. Vestibular-evoked myogenic potentials in central vestibular disorders. J Neurol. 2016; 263:210–220.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Principle and Methodology of Vestibular Evoked Myogenic Potential
- Clinical Applications of Vestibular Evoked Myogenic Potentials in Vestibular Disorders
- Characteristics of Vestibular Evoked Myogenic Potentials in Meniere's Disease
- Cervical Vestibular Evoked Myogenic Potential and Ocular Vestibular Evoked Myogenic Potential in Patients With Vestibular Neuritis and Acute Viral Labyrinthitis
- Vestibular-Evoked Myogenic Potentials: Sound- and Bone-Conducted Stimuli and Clinical Applications