J Korean Med Sci.
2021 Jan;36(2):e15. 10.3346/jkms.2021.36.e15.
Impact of Cardiovascular Risk Factors and Cardiovascular Diseases on Outcomes in Patients Hospitalized with COVID-19 in Daegu Metropolitan City
- Affiliations
-
- 1Department of Internal Medicine, Kyungpook National University Hospital, Daegu, Korea
- 2Department of Internal Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 3Department of Internal Medicine, Daegu Fatima Hospital, Daegu, Korea
- 4Department of Internal Medicine, Keimyung University Dongsan Medical Center, Daegu, Korea
- 5Department of Internal Medicine, Daegu Catholic University Hospital, Daegu, Korea
- 6Department of Internal Medicine, Yeungnam University Hospital, Daegu, Korea
- KMID: 2510588
- DOI: http://doi.org/10.3346/jkms.2021.36.e15
Abstract
- Background
Data regarding the association between preexisting cardiovascular risk factors (CVRFs) and cardiovascular diseases (CVDs) and the outcomes of patients requiring hospitalization for coronavirus disease 2019 (COVID-19) are limited. Therefore, the aim of this study was to investigate the impact of preexisting CVRFs or CVDs on the outcomes of patients with COVID-19 hospitalized in a Korean healthcare system.
Methods
Patients with COVID-19 admitted to 10 hospitals in Daegu Metropolitan City, Korea, were examined. All sequentially hospitalized patients between February 15, 2020, and April 24, 2020, were enrolled in this study. All patients were confirmed to have COVID-19 based on the positive results on the polymerase chain reaction testing of nasopharyngeal samples. Clinical outcomes during hospitalization, such as requiring intensive care and invasive mechanical ventilation (MV) and death, were evaluated. Moreover, data on baseline comorbidities such as a history of diabetes, hypertension, dyslipidemia, current smoking, heart failure, coronary artery disease, cerebrovascular accidents, and other chronic cardiac diseases were obtained.
Results
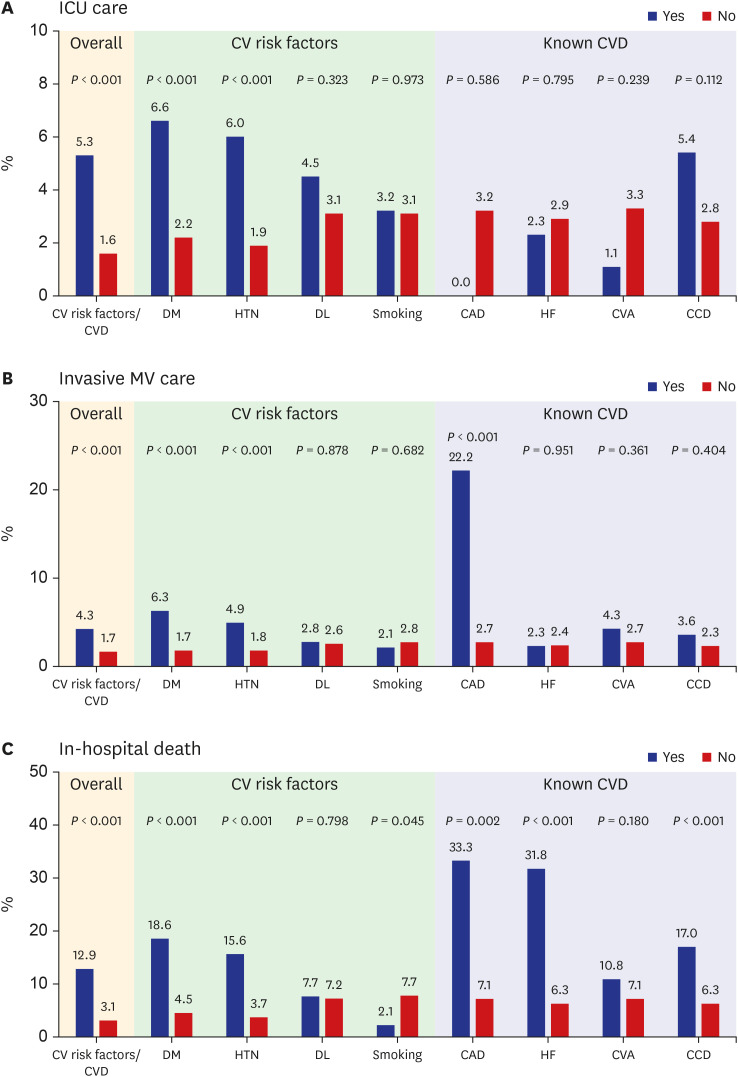
Of all the patients enrolled, 954 (42.0%) had preexisting CVRFs or CVDs. Among the CVRFs, the most common were hypertension (28.8%) and diabetes mellitus (17.0%). The prevalence rates of preexisting CVRFs or CVDs increased with age (P < 0.001). The number of patients requiring intensive care (P < 0.001) and invasive MV (P < 0.001) increased with age. The in-hospital death rate increased with age (P < 0.001). Patients requiring intensive care (5.3% vs. 1.6%; P < 0.001) and invasive MV (4.3% vs. 1.7%; P < 0.001) were significantly greater in patients with preexisting CVRFs or CVDs. In-hospital mortality (12.9% vs. 3.1%; P < 0.001) was significantly higher in patients with preexisting CVRFs or CVDs. Among the CVRFs, diabetes mellitus and hypertension were associated with increased requirement of intensive care and invasive MV and in-hospital death. Among the known CVDs, coronary artery disease and congestive heart failure were associated with invasive MV and in-hospital death. In multivariate analysis, preexisting CVRFs or CVDs (odds ratio [OR], 1.79; 95% confidence interval [CI], 1.07–3.01; P = 0.027) were independent predictors of in-hospital death adjusting for confounding variables. Among individual preexisting CVRF or CVD components, diabetes mellitus (OR, 2.43; 95% CI, 1.51–3.90; P < 0.001) and congestive heart failure (OR, 2.43; 95% CI, 1.06–5.87; P = 0.049) were independent predictors of in-hospital death.
Conclusion
Based on the findings of this study, the patients with confirmed COVID-19 with preexisting CVRFs or CVDs had worse clinical outcomes. Caution is required in dealing with these patients at triage.after
Keyword
Figure
Cited by 1 articles
-
Letter to the Editor: Impact of Cardiovascular Risk Factors and Cardiovascular Diseases on Outcomes in Patients Hospitalized with COVID-19 in Daegu Metropolitan City
Eftychios Siniorakis, Spyridon Arvanitakis, Antonios Katsianis, Ioannis Nikolopoulos
J Korean Med Sci. 2021;36(15):e113. doi: 10.3346/jkms.2021.36.e113.
Reference
-
1. World Health Organization. WHO Director- General's opening remarks at the media briefing on COVID-19 - 11 March 2020. Updated 2020. Accessed March 12, 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.2. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020; 395(10223):497–506. PMID: 31986264.
Article3. Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020; 323(11):1061–1069. PMID: 32031570.
Article4. Ruan Q, Yang K, Wang W, Jiang L, Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020; 46(5):846–848. PMID: 32125452.
Article5. Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020; 395(10229):1054–1062. PMID: 32171076.
Article6. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020; 180(7):934–943. PMID: 32167524.
Article7. Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020; 382(18):1708–1720. PMID: 32109013.8. Fang Z, Yi F, Wu K, Kang Wu, Lai K, Sun X, et al. Clinical characteristics of coronavirus pneumonia 2019 (COVID-19): an updated systematic review. MedRxiv;Updated 2020. Accessed August 7, 2020. https://www.medrxiv.org/content/10.1101/2020.03.07.20032573v2.9. Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020; 323(13):1239–1242. PMID: 32091533.10. Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, et al. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol. 2020; 109(5):531–538. PMID: 32161990.
Article11. Xiong TY, Redwood S, Prendergast B, Chen M. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020; 41(19):1798–1800. PMID: 32186331.
Article12. Zheng YY, Ma YT, Zhang JY, Xie X. COVID-19 and the cardiovascular system. Nat Rev Cardiol. 2020; 17(5):259–260. PMID: 32139904.
Article13. Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D. Structure, function, and antigenicity of the SARS-CoV-2 spike glycoprotein. Cell. 2020; 181(2):281–292.e6. PMID: 32155444.
Article14. Turner AJ, Hiscox JA, Hooper NM. ACE2: from vasopeptidase to SARS virus receptor. Trends Pharmacol Sci. 2004; 25(6):291–294. PMID: 15165741.
Article15. Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020; 323(20):2052–2059. PMID: 32320003.
Article16. Siddiqi HK, Mehra MR. COVID-19 illness in native and immunosuppressed states: A clinical-therapeutic staging proposal. J Heart Lung Transplant. 2020; 39(5):405–407. PMID: 32362390.
Article17. Libby P, Loscalzo J, Ridker PM, Farkouh ME, Hsue PY, Fuster V, et al. Inflammation, immunity, and infection in atherothrombosis: JACC review topic of the week. J Am Coll Cardiol. 2018; 72(17):2071–2081. PMID: 30336831.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter to the Editor: Impact of Cardiovascular Risk Factors and Cardiovascular Diseases on Outcomes in Patients Hospitalized with COVID-19 in Daegu Metropolitan City
- Cardiovascular Imaging Asia in the Era of the COVID-19 Outbreak
- Impact of solid organ transplantation on the effectiveness of COVID-19 vaccination in hospitalized patients with COVID-19: a propensity score-matched cohort study
- Cardiovascular Manifestations of COVID-19
- Preparations for the Assessment of COVID-19 Infection and Long-Term Cardiovascular Risk